1. Background
Gallstones are mostly known to be an adult disease. The incidence of gallstones in adults is 15% to 20% in the western societies. In recent years, it has been reported that the incidence of gallstones has increased in children (1-3). It is known that early diagnosis due to extensive use of ultrasonography is the main reason for higher incidence of pediatric gallstones. Still, risk factors, such as obesity, are also considered responsible (1).
While pediatric patients with gallstones are often diagnosed incidentally, some patients are admitted with the symptoms of gallstone complications (4). However, the reason why some patients develop gallstone complications has not been clearly defined. In addition, there is an ongoing debate on the risk factors for gallstone complications (2, 5).
Although cholecystectomy is recommended for complicated gallstones, the treatment of uncomplicated gallstone disease remains controversial. However, despite cholecystectomy, abdominal symptoms are not relieved in 1/3 of uncomplicated gallstone patients (6). Therefore, we think that these patients may be exposed to complications of cholecystectomy and unnecessary health expenses.
2. Objectives
In the present study, we aimed to investigate the effects of risk factors on gallstone-related complications and to identify the surgical indications in uncomplicated gallstone disease.
3. Methods
An approval of the local ethics committee was obtained for this study. The study was conducted in accordance with the principles of the Declaration of Helsinki.
Patients with gallstones who had surgery in the Pediatric Clinic of Sakarya University Faculty of Medicine between October 2011 and January 2018 were included in this retrospective study. Patients with preexisting choledochal cysts were excluded from the study.
Data including age and sex, weight and height, comorbidities, risk factors, symptoms, diagnostic methods, preoperative treatment, surgical treatment, complications, and pathology results of all patients were recorded from files.
3.1. Complaints
Patients were divided into two groups. Group 1 (Uncomplicated group), included patients without any gallstone complications from patient files. In group 2 (Complicated group), patients were admitted with complaints of gallstone complications (cholecystitis, common bile duct dilatation and pancreatitis) on admission. According to patients’ stories, all patients had applied to the hospital on their first complications attack.
3.2. Risk Factors
Risk factors for gallstones were searched regarding the studies of Gokce et al. (7) and Serdaroglu et al. (8). Obesity, family history, ceftriaxone usage, staying in the intensive care unit, total parenteral nutrition (TPN) usage, diabetes, ileum resection, the presence of Down syndrome, and history of cardiac surgery were investigated as risk factors.
After calculating body mass index (BMI) and evaluating Z-scores, patients were divided into three groups: Obese, overweight, and normal weight (9). Clinical and physical examination, and laboratory and monitoring techniques were used for diagnosis. All patients consulted the pediatric hematology unit for hematologic evaluation. Ultrasonography was used as the monitoring technique. The increase in gallbladder wall thickness and the presence of pericholecystic fluid in patients who were diagnosed using ultrasound were observed in favor of cholecystitis (10). Bile duct diameters of 6 mm and greater were considered as common bile duct dilatation (5), and all of the patients with choledochal dilatation were administered magnetic resonance imaging (MRI).
Cholecystectomies were done for patients with symptomatic gallstones with or without complications, and postoperative complications in both groups were recorded. Patients underwent laparoscopic cholecystectomies and conventional (open) surgeries. In group 2, patients underwent surgical treatment following medical treatment of complications. None of the patients required urgent cholecystectomy.
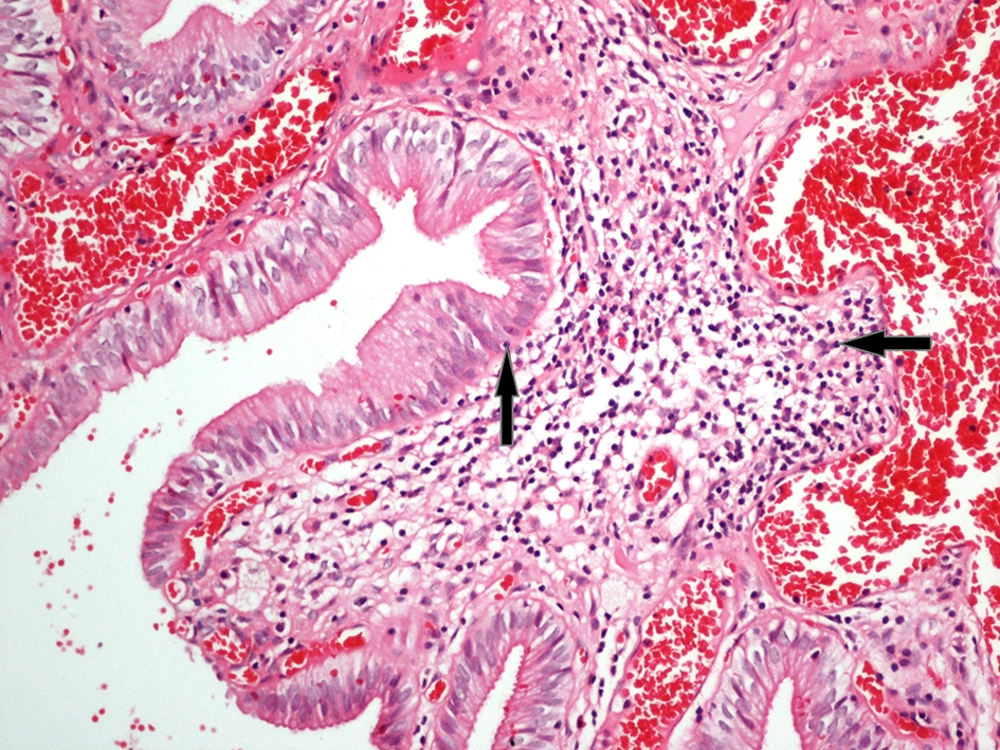
3.3. Histopathological Evaluation
The tissue samples for histopathological examinations were fixed in 10% neutral buffered formalin, embedded in paraffin wax, and cut into 5 mm sections. Hematoxylin and eosin were used to stain the specimens. The histological sections were examined for the presence of mononuclear inflammation, fibrosis, and metaplastic changes with a light microscope (Nikon Eclipse, Kanagawa, Japan) and photographed. In the histopathological evaluation, the previously defined criteria specified by Barcia (11) were used, and the same pathologist twice examined all tissue samples.
Patients were discharged within 3 to 9 postoperative days, and follow-up examinations were scheduled for ten days, one month, and six months after discharge; problems were recorded.
3.4. Statistical Analysis
The Mann-Whitney U-test was used to compare the patients’ ages and was presented as the mean ± standard deviation (SD). Categorical variables were compared by the chi-square test, presented as counts and percentages, and a P value < 0.05 was considered significant. Analyses were performed using commercial software (IBM SPSS Statistics, Version 23.0. Armonk, NY: IBM Corp.).
4. Results
Patient characteristics are shown in Table 1. A total of 72 patients who were admitted to the Pediatric Surgery Clinic of Sakarya University Educations and Research Hospital with a complaint of abdominal pain and diagnosed with gallstones were included in the study. The mean age of the patients was 158.14 ± 42.3 months (range: 38 to 205 months). The mean age of female and male patients was 163.6 ± 6.43 and 145.7 ± 17.93 months, respectively. The mean age of girls was higher than that of boys, but the difference was not statistically significant (P > 0.05). Fifty patients (69.4%) were female, and 22 patients (30.6%) were male (F/M = 2.27/1).
| Total | Group 1 (N = 40) | Group 2 (N = 32) | P Value | |
|---|---|---|---|---|
| Age | 158.14 ± 42.3 | 155.05 ± 41.74 | 162 ± 44.03 | 0.626 |
| Gender | 0.909 | |||
| Female | 50 (69.4) | 28 (70) | 22 (68.8) | |
| Male | 22 (30.6) | 12 (30) | 10(31.3) | |
| BMI | 0.273 | |||
| Normal | 54 (75) | 28 (70) | 26 (81.3) | |
| Obese | 18 (25) | 12 (30) | 6 (18.8) | |
| Risk factors | 0.442 | |||
| Absent | 26 (36.1) | 16 (40) | 10 (31.3) | |
| Present | 46 (63.9) | 24 (60) | 22 (68.8) | |
| Postop. complaints | 0.020 | |||
| Absent | 59 (81.9) | 29 (72.5) | 30 (93.75) | |
| Present | 13 (18.1) | 11 (27.5) | 2 (6.25) | |
| Pathology | 0.022 | |||
| Absent | 6 (8.3) | 6 (15) | 0 (0) | |
| Present | 68 (91.7) | 34 (85) | 32 (100) |
aValues are expressed as No. (%) or mean ± SD.
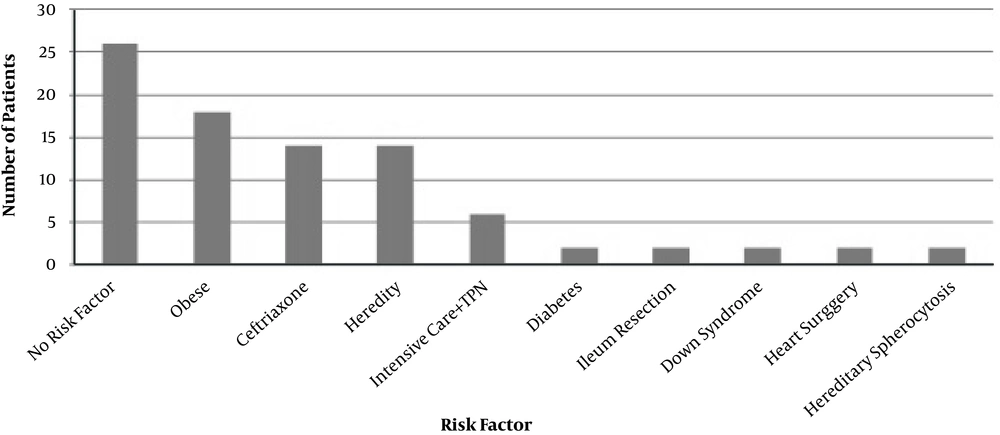
4.1. Risk Factors
Among the patients with gallstones, 46 patients (63.9%) had at least one risk factor, whereas 26 patients (36.1%) did not have any risk factors. Two patients had hereditary spherocytosis in the hematologic etiology and underwent cholecystectomy along with splenectomy. A family history of gallstones was also present in ten patients (13.8%). The other risk factors were obesity, ceftriaxone usage, staying in the intensive care unit, TPN usage, diabetes, ileum resection, the presence of Down syndrome, and a history of cardiac surgery. Also, eight patients had two risk factors (Figure 1).
Eighteen patients (25%) were obese with a Z-score > 2 (BMI > 30 kg/m2), and 14 patients (19.4%) were overweight with a Z-score > 1 (BMI > 25 kg/m2). Forty patients (55.6%) were normal weight. However, only obese patients were considered as the risk group.
4.2. Patient Groups
Group 1 (Uncomplicated group) had forty patients (55.6%) and did not have any complications on admission. Group 2 (complicated group) had thirty-two patients (44.4%) and at least one gallstone complication on admission. Twenty-eight of complicated (group 2) patients had the findings of cholecystitis, four patients had the findings of pancreatitis, and eight patients had common bile duct dilatation. However, none of the patients who were diagnosed with common bile duct dilatation had a choledochal cyst. All patients had abdominal pain on admission, fourteen patients had nausea and vomiting, six patients had jaundice, two patients had uneasiness, and eighteen patients had undergone a sonographic Murphy’s sign. And, we started treatment for complicated gallstones.
Six obese patients were admitted with complications; however, there was no significant correlation between obesity and complication on admission (P = 0.273). Twenty-two patients who had complications on admission also had risk factors, but there was no significant correlation between the risk factor and complication on admission (P = 0.442). Two patients (2.7%) underwent open surgery, whereas 70 patients (97.2%) underwent laparoscopic surgery.
Complaints of thirteen patients (18.1%) continued in the postoperative period. Eleven (27.5%) of patients did not have any gallstone complications, and there was a significant correlation between the uncomplicated group and postoperative complaints (P = 0.020). Nine patients (56.25%) in the risk-free group had continued complaints during the postoperative period (P = 0.001).
Postoperatively two patients (2.7%) had complications. One of the patients was in the gallstone complication group and the other was in the uncomplicated group. There was no significant correlation between gallstone complications and postoperative complications.
Chronic cholecystitis findings were identified in all but six pathological specimens. Among these specimens, 91.7% (n = 66) had inflammation (Figure 2), and 64.7% (n = 44) had fibrosis. None of the patients had metaplasia. Six patients (15%) had normal pathology specimens in the uncomplicated group (P = 0.022). Of these six patients, five patients did not have any risk factors, one patient had ceftriaxone risk factor, and there was a significant relationship between risk-free and normal pathology specimens (P = 0.019).
5. Discussion
The incidence of cholecystectomy has risen in the last 20 years. According to a UK study, the frequency ranges between 0.78 and 2.7/100,000 in children who are under 16 years old (12-14). Some authors have suggested that the incidence of gallstones in males and females are similar, while others have reported gallstones are four times more common in males than females (7, 12). In addition, studies on adults have shown that the incidence of gallstone formation increases with estrogen levels in female patients (15). In the present study, it was observed that gallstones were more frequent in girls, which might be related to their higher estrogen levels.
The rate of patients who did not have risk factors ranges between 23.2% and 52.5% in the literature (7, 8, 16). In the current study, we did not identify any risk factors in 36.1% of the patients. Although obesity was one of the most common risk factors, the use of ceftriaxone and genetic susceptibility were also reported among significant risk factors in the studies (7, 17). We identified obesity as the most common risk factor, which was present in 25% of the patients. The other common risk factors we found were ceftriaxone use (13.8%) and genetic susceptibility (13.8%). According to some reports, hemolytic anemia is also a common risk factor (18, 19). However, recent studies have reported that hemolytic anemia is not considered among common risk factors (11). Similarly, we found a hematological cause in only two patients (2.7%).
Patients with gallstones are admitted to hospitals with various complications. The most common complications are cholecystitis, choledocholithiasis, and pancreatitis (13). Gokce et al. (7) reported that cholecystitis is the most common complication. In the current study, 44.4% of the patients had complications with cholecystitis being the most common one. Previous studies showed that 25.1% to 58% of the patients with gallstones were admitted with complications to hospitals (13, 20). The relationship between gallstone complications and risk factors for gallstones has not been extensively investigated. Only Tuna Kirsaclioglu et al. (2) have researched the risk factors and found they had a significant effect on the development of complications. However, in the current study, we found that risk factors had no impact on gallstone complications.
Gallstone treatment in pediatric patients is dependent on symptoms (5). Medical and surgical treatment is used in pediatric gallstones. Ursodeoxycholic acid (UDCA) is used in medical treatment and dissolves gallstones in 19% - 37% of cases. Some studies have reported that UDCA had no effect on gallstones and some had an effect. There is no consensus on the medical or surgical treatment of pediatric gallstones (21, 22). Cholecystectomy was an adopted treatment in all pediatric patients with symptomatic gallstone and gallstone complications (5, 11). However, the indications for cholecystectomy in gallstone disease have undergone major revisions in recent days. Nowadays, patients with complicated gallstones are recommended for cholecystectomies as in previous guidelines. Some authors, however, have suggested that uncomplicated symptomatic gallstone disease should be treated conservatively in some patients (6). As a result, the application of cholecystectomies in patients with no typical symptoms (asymptomatic patients) is an ongoing matter of debate (5, 12). In the current study, we performed cholecystectomies on the patients, but some complaints (27.5%) continued during the postoperative period in the uncomplicated group. Also, nine of these patients did not have any risk factors, and there were significant relationships between complaints and risk factors. We think that the cholecystectomy decision should be re-evaluated before children with uncomplicated and risk-free gallstones undergo surgery.
Postoperative complications rates are 2% - 17% in adult patients and include bile leakage, intra-abdominal bleeding and abscess, intestinal perforation, and hernia (16, 23). The most common complication is bile duct injury, but little has been published about postoperative complications for children who undergo laparoscopic cholecystectomy (24). In the present study, only two of the postoperative patients (2.7%) had complications. Some authors think postoperative complication rates are related to the severity of complicated gallstones (16, 24). However, cholecystectomies performed as soon as possible result in less morbidity in patients with acute cholecystitis (6), and we think the low number of postoperative complications is because patients had fewer complication episodes.
According to the literature, cholecystitis is the main diagnosis in the histopathological examination done after a cholecystectomy. The rate of chronic cholecystitis varies between 64.8% and 92.3%. However, these studies examined pathological findings and cholecystitis in adults (11, 25). In the present study, the rate of chronic cholecystitis was 91.7%, but six of the patients who had no chronic cholecystitis were in the patient group without complication. There were also significant correlations between postoperative complaints and pathology specimens in the uncomplicated group. Therefore, we believe that cholecystectomy is unnecessary for some patients in the uncomplicated group.
Inability of current patients to number is the limitation of the present study. Therefore, a well-designed, prospective, multicentered, extensive study is needed. Another limitation is that the morphological and biochemical features of gallstones were not correlated with their clinical presentation and development of complications.
In conclusion, laparoscopic cholecystectomy should be a successful treatment method in children; however, some complaints persisted in risk-free and uncomplicated gallstones. Therefore, we think if there are no risk factors in uncomplicated patients, they should not receive surgery but be closely monitored instead.