1. Background
Postural disorders are one of the most common diseases among pediatric population. Though some of them are typical for some periods of growth and development, others could result in serious health problems including impaired capability in life and career and reduced quality of life (1, 2). Most of the postural deformities start in childhood and their harmful effects could be continued till adulthood. Recent epidemiological studies have indicated that the prevalence of postural deformities has increased significantly over the past decades due to life style modification. The reported prevalence rate for the deformities has great variability ranging from 10 to 70% (3, 4).
Some factors including age, gender, and ethnicity, somatic structure of the bone joints and muscles and mental status are associated with the disorders (5). But recently the role of other factors related to life style such as physical inactivity, Increased time spent watching TV or playing video games, heavy backpacks, prolonged inadequate positions, as well as unhealthy diet have been demonstrated in this regard (6).
Obesity as a consequence of physical inactivity, Increased time spent watching TV or playing video games, and unhealthy nutrition accounts for the most important risk factors of postural deformities (7).
According to estimation of the World Health Organization, number of overweight and obesity in children would be increased to 70 million in 2025 and the increasing trend would be 30% higher in developing countries (8).
Evidences indicated that obesity could have negative effects on body stability, morphology of the locomotor system and plantar pressure (9). Thus, in addition to other reported metabolic and psychological consequences, musculoskeletal comorbidities are a frequent problem in overweight and obese children (10, 11).
Results of a recent review study indicated that obesity could increase the probability of occurrence of postural deformities in children (12). The authors recommended to improve the management process of childhood obesity to prevent its related complications including poor posture (12).
2. Objectives
Considering the increasing trend of obesity and its association with postural disorders in pediatric population as well as the fact that by providing baseline information about the prevalence of different postural deformities in normal weight and obese children we could develop proper interventions for management of obesity and prevention of postural disorders in children, we aimed to determine its prevalence rate among school children in Qom province.
3. Methods
This study was designed as a cross-sectional study conducted in Qom province from March 2015 - February 2016. Schoolchildren aged 6 - 7 years from primary schools of Qom province were enrolled. In order to have a representative sample, 1450 (620 girls and 830 boys) out of 20000 school children were selected by multi-stage clustering sampling method from all urban and rural regions of Qom province.
Ethics Committee of Qom University of Medical Sciences approved protocol of the study.
History of systematic or neurological diseases and musculoskeletal disorders or trauma in selected subjects was denied. In physical examination, those with congenital deformities, joint stiffness, joint hypermobility, history of fracture, lower limb operation or lower leg or foot dislocation were excluded.
The aims and methods of the study were described in details for both school authorities and parents of the selected children. Written informed consent was obtained from parents of the children.
Demographic characteristics were recorded by a trained health care staff. All participants were clinically examined by a general practitioner and anthropometric measurements including height, weight and body mass index (BMI) were performed and recorded. Presence of postural deformities of lower limb, including genu valgum, genu varum and flat foot were evaluated and recorded. Prevalence's of the deformities in different categories of weight status (normal, overweight and obese) were compared.
Mean of waist to hip ratio and skin fold thickness in students with and without lower extremities postural abnormalities were compared.
Height and weight of the children were measured in standing position with light cloths using SECA (Hamburg, Germany) stadiometer and scale. The BMI was calculated as the ratio of weight (kg) to height squared (m2). Weight status was categorized as underweight, normal weight, overweight and obese according to the World Health Organization standard growth curves (13).
Waist circumference (WC) and hip circumference (HC) were measured at the midway between the lower rib and the iliac crest and at the level of maximal protrusion of the gluteal muscles using a measuring tape. Waist circumference to hip ratio (WHR) was calculated by dividing WC to HC in cm.
For consistency of skinfold thickness measurement, in all participants the skin over triceps and calf of the right side was measured. A double layer of adipose tissue and its surrounding skin was pinched by the healthcare staff and its thickness was measured 1cm below the right angle of the pinched skin using the Holtain Skinfold Caliper (Crymmych, Dyfed, UK).
3.1. Assessment of Lower Limb Postural Deformities
For evaluation of lower limb postural deformities, the participants were asked to stand in the lateral and then anteroposterior plane. Genu valgum and genu varum, were evaluated in anterior view. The tibiofemoral angle (TF angle) was measured using a goniometer. For measurement of intercondylar (IC) and intermalleolar (IM) distance, the children were asked to stand in a position with both knees or ankles touching. The distances were measured using a tape.
Intermalleolar distance in normal children aged 2 - 11 years was mesured up to 8 cm and genu valgum up to 12 degrees (14). Distance between IM and IC more than 8 cm and 5 cm was considered as genu valgum and genu varum, respectively. The severity of genu valgum is graded as mild: 8 - 10 cm, moderate: 10 - 15 cm and severe: > 15 cm. The severity of genu varum is graded as grade I: 5 - 7.5 cm, grade II: 7.5 - 10 cm and grade III: > 10 cm (15).
For evaluation of flat foot, navicular drop (ND) test was used. The navicular tuberosity was measured in non-weight bearing foot position with the subtalar joint in neutral position. The navicular height was measured in a full weight bearing position (standing) with 50% weight bearing on the foot.
3.2. Statistical Analysis
Obtained data was recorded and analyzed using SPSS version 21 software (SPSS Inc., Chicago, IL, U.S.A.). Continuous variables were presented as Mean ± SD. Qualitative variables were presented as number and percentage. Between groups comparison for continuous and qualitative variables was assessed using t Student and chi-square tests, respectively. The relation between occurrence of lower limb postural deformities and different studied variables was assessed using logistic regression test.
4. Results
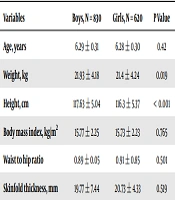
Demographic and anthropometric characteristics of studied population are presented in Table 1.
| Variables | Boys, N = 830 | Girls, N = 620 | P Value |
|---|---|---|---|
| Age, years | 6.29 ± 0.31 | 6.28 ± 0.30 | 0.42 |
| Weight, kg | 21.93 ± 4.18 | 21.4 ± 4.24 | 0.019 |
| Height, cm | 117.63 ± 5.04 | 116.3 ± 5.37 | < 0.001 |
| Body mass index, kg/m2 | 15.77 ± 2.25 | 15.73 ± 2.23 | 0.765 |
| Waist to hip ratio | 0.89 ± 0.05 | 0.91 ± 0.85 | 0.501 |
| Skinfold thickness, mm | 19.77 ± 7.44 | 20.73 ± 4.33 | 0.519 |
aValues are expressed as mean ± SD.
Genu valgum, genu varum and flat foot was found in 256 (17.7%), 351 (24.2%) and 194 (13.38%) of studied population. The severity of genu valgum in all children was mild and that of severity of genu varum was of grade I.
Prevalence's of different lower extremities postural abnormalities with regard to gender are presented in Table 2. Prevalence of genu valgum and genu varum was significantly higher in boys. 1021 (70.41%), 161 (11.11%) and 268 (18.48%) students were normal weight, underweight and overweight/obese, respectively.
| Postural Abnormalities | Boys, N = 830 | Girls, N = 620 | P Value |
|---|---|---|---|
| Genu valgum | 146 (17.6) | 110 (17.7) | 0.940 |
| Genu varum | 229 (27.6) | 122 (19.7) | 0.001 |
| Flat foot | 112 (13.5) | 82 (13.2) | 0.882 |
aValues are expressed as No. (%).
Table 3 shows the prevalence of postural abnormalities in normal weight, underweight, and obese/overweight students. Prevalence of flat foot and genu valgum was significantly higher in obese/overweight students (P < 0.001). Mean ± SD of waist to hip ratio and skin fold thickness in students with and without lower extremities postural abnormalities are presented in Table 4. Mean of skin fold thickness was significantly higher in students with genu valgum (P = 0.002).
| Postural Abnormalities | Underweight, N = 161 | Normal Weight, N = 1021 | Overweight/Obese, N = 268 | P Value |
|---|---|---|---|---|
| Genu varum | 52 (32.3) | 273 (26.7) | 26 (9.7) | < 0.001 |
| Genu valgum | 21 (13) | 131 (12.8) | 104 (38.8) | < 0.001 |
| Flat foot | 14 (8.7) | 130 (12.7) | 50 (18.7) | 0.007 |
| Postural Abnormalities | Number | Skinfold Thickness | P Value | Waist/Hip Ratio | P Value |
|---|---|---|---|---|---|
| With genu valgum | 256 | 23.39 ± 7.8 | < 0.001 | 0.890 ± 0.06 | 0.819 |
| Without genu valgum | 1194 | 18.51 ± 5.41 | 0.899 ± 0.62 | ||
| With genu varum | 351 | 18.22 ± 4.83 | 0.36 | 0.88 ± 0.08 | 0.511 |
| Without genu varum | 1099 | 19.74 ± 6.31 | 0.9 ± 0.05 | ||
| With flat foot | 194 | 19.88 ± 7 | 0.210 | 0.89 ± 0.04 | 0.831 |
| Without flat foot | 1256 | 19.30 ± 5.85 | 0.90 ± 0.6 |
Analysis of logistic regression indicated that a significant correlation existed only between occurrence of lower limb postural deformities and BMI [OR = 1.89, CI (95%) = 1.18 - 3.03].
5. Discussion
In this study, we evaluated the prevalence of some common lower limb postural deformities in a representative sample of children in Qom province and compared its rate in children with different weight categories.
We found genu valgum, genu varum and flat foot with a prevalence of 7.7%, 24.2% and 13.38%, respectively. Genu varum was the most common postural deformity in our province children. Different studies from different regions worldwide and also from different cities of Iran have reported various results in this field (16, 17). Mirzaei and Salimi have showed that the prevalence of flat foot, genu varum and genu valgum was 3.4%, 43.08% and 1.9% respectively, among guidance school children (16). Zakeri et al. have reported that the prevalence of genu valgum, genu varum and flat foot among 6 - 9 years old school children of Abadan was 8.9%, 18.1% and 25.7%, respectively (17). Pourghasem et al. found the prevalence of flat foot among 6 - 10 year-old school children of Babol 21.8% (18). Differences in the results of studies may be due to a different study population, different definitions of skeletal disorders as well as the time of the study. In addition, nutrient intakes that protect the skeleton vary in geographical areas, which can explain the difference in the prevalence of skeletal disorders in different regions.
We evaluated the prevalence of some common lower limb deformities in obese and overweight children including genu valgum, genu varum and flat foot. The prevalence of overweight and obesity was 18% - 19%. This is in the range of reported prevalence rates for overweight and obesity in Iran and other countries (19, 20).
Our findings reveal a significant correlation between occurrence of lower limb postural deformities and BMI. In our studied population, the prevalence of genu valgum and flat foot was higher in overweight and obese than in normal weight and underweight children. In addition, mean of skinfold thickness was significantly higher in children with genu valgum than those without.
Several studies have indicated that the rate of musculoskeletal problems is higher in obese/overweight children. Though the reported feature of musculoskeletal problems or postural disorders in obese/overweight children has great variability in different studies (21, 22), some evidences, as reported by Kurl et al., have showed that deformities of lower extremities are more frequent in this group of children and of which those related to ankle and foot are more common (21).
Our results regarding the higher rate of genu valgum in obese and overweight children were similar to some previous reports (23-25). Rahmani Nia and colleagues in Guilan, Iran, demonstrated that overweight/obesity and increased level of BMI result in increased loading of the knees and lower limb leading to higher rate of genu valgum among obese/overweight high school girls (23). Kuni et al. in Germany have examined 46 overweight and 42 non-overweight children and indicated that genu valgum was more common in overweight girls (24).
Regarding the higher skin fold thickness in children with genu valgum, there was no report for comparing our results, but it seems that elevated skin fold thickness, which is considered as a sign for increased body fat, is associated with higher frequency of genu valgum. The rate of flat foot also was higher in obese/overweight children than normal weight and underweight ones. Results of previous reports in this field are not similar, but most of them have reported higher rate of flat foot in obese children. Ezema et al. in Nigeria have demonstrated that obesity is a risk factor for flat foot (26). Chang et al. in a nationwide study in Taiwan, have found that the prevalence of flat foot was 1.39 - 2.66 times higher in obese/overweight children (27). In a study in Isfahan-Iran, Sadeghi-Demneh et al. concluded that obesity is associated with higher rate of foot and ankle deformities including flat foot (28). In a recent study in Tehran, Borimnejad et al. have reported a 20% prevalence rate for flat foot among elementary school children and showed a significant association between flat foot and BMI (29). Evans and Scutter in a study in Australia in 7 - 10 years old school children have observed that obese children had less flat feet (30). Observed differences between different studies is mainly due to the evaluation methods, different age and sex groups as well as ethnicity or lifestyles. Sabharwal et al., in a study showed that there is an association between increased BMI and onset of tibia vara at < 4 years of age, this result suggests the theory that compressive forces across the physis are responsible for the resultant varus deformity (31).
We found genu varum more common in children and more frequent among boys. Previous studies indicated that the rate would be affected by different factors including age, sex, ethnicity as well as different method of evaluation (32, 33). Shohat et al. showed that in adult population genu varum was significantly more prevalent among males than females (16.2% vs. 4.4%) (34).
In the present study genu varum was significantly less prevalent among overweight/obese children. The results of this study are consistent with other studies that were conducted in adults and showed that the prevalence of genu varum is less prevalent among overweight and obese subjects (34).
The implication of current study is that postural deformities should be screened in overweight and obese children as a high-risk population. Moreover, both children and their parents should be informed about the complications of obesity and importance of its proper management and prevention. Given the fact that musculoskeletal development of the children mainly plateaus after the age of 9 years (35), it is recommended to develop routine screening program for postural deformities between the ages of 7 - 9 years.
The main limitation of current study was including only 5 - 7 years old children. Our results would have been more helpful if all elementary school's children were included. However, this study is considered as a pilot study for planning future similar studies in both elementary and high school children as well as adolescents. Further, considering the cross sectional design of this study, our results could not provide causal relationship between obesity and mentioned deformities, so, prospective longitudinal studies are recommended for obtaining more accurate results in this field. The strength of current study was its large sample size and method of sampling which provided us a representative sample of children in the mentioned age group.
5.1. Conclusions
The findings of this study showed that prevalence of genu valgum and flat foot is higher in overweight/obese children. Our results indicated that in addition to early diagnosis and timely treatment of the deformities to prevent their progress and related complications, developing and validation of a multidisciplinary care for obese and overweight children to reduce the occurrence of obesity related musculoskeletal is of importance. Further, appropriate targeted educational and interventional studies should be provided for both schoolchildren and health care professionals to promote their information on the impact of overweight and obesity on the foot and lower limb function as well as healthy lifestyle.