1. Background
The number of children requiring long term mechanical ventilation support which is a treatment option for children with chronic respiratory failure is increasing (1). This is a consequence of advancements in neonatal and pediatric intensive care services and technology that have led to the longer survival rates of critically ill patients as well as the development of medical equipment suitable for using at home. In previous decades, patients requiring long term mechanical ventilation have been primarily hospitalized in intensive care units. Prolonged length of stay in hospital has led to ineffective use of valuable beds, increased rates of nosocomial infection and costs. Additionally, hospitals and in particular pediatric intensive care units do not offer a suitable environment for the normal development of these children. Using mechanical ventilators at home allows patients with chronic respiratory failure to be discharged from hospital (2). Ventilation at home not only reduces bed occupation in intensive care units, but also helps to decrease hospital infection rates, and health expenditures, while helping to increase the patient’s physical and psychological functions and QoL (1, 3). Home care is a preferable alternative for children who are medically stable and require long term mechanical ventilation support. Furthermore, discharge of a child with home mechanical ventilator support leads to important changes in social life of his/her family (4). Before the discharge process, all care givers should be educated in patient care, potential problems and their solution. They should be in close contact with doctors and other medical staff (2). In this study, we try to demonstrate clinical characteristics and follow up results of pediatric patients who are dependent on invasive HMV support.
2. Methods
We performed a retrospective review of patients who were on invasive HMV in Hacettepe University Ihsan Dogramaci children’s hospital pediatric intensive care unit. Indication for HMV was determined by a pediatric intensivist and a pediatric pulmonologist. Before making a decision for the use of HMV, mechanical ventilation was weaned in all patients following the tracheostomy procedure. Patients were then prescribed with a mechanical ventilator and followed up for family education by doctors and nurses in our pediatric services before being discharged to home. There was no health care professional for caring these patients at home for 24 hours. Primary care was given by the parents.
The medical records were examined in terms age, diagnosis at admission, complications, length of stay in PICU, length of stay in hospital, routes of feeding, surgical procedures during hospitalization, rehospitalization, and duration of HMV. Patients’ BMIs were calculated using SD WHO Anthro, WHO Anthro plus computer programs.
The Local Ethics Board of Hacettepe University approved this study.
Statistical analysis was performed with SPSS 15 for Windows software using Kaplan Meier, and Pearson Chi-Square tests.
3. Results
We examined results of 61 patients who had been discharged with HMV from the pediatric intensive care unit. The median age of patients was 8.5 (minimum 2- maximum 196) months with 60% of them being younger than 12 months.
The decision for HMV was made after median 38 ± 37.2 days of mechanical ventilation in hospital. The median duration of follow up was 11 months (4 days-7.5 years). The most common reason of dependency on invasive HMV was found as central nervous system and neuromuscular diseases by 94%. Diagnoses of the patients are shown in Table 1. HMV was most commonly used in patients with spinal muscular atrophy (SMA) (11 patients).
| Underlying Disease | No. |
|---|---|
| Chronic lung disease | 3 |
| Congenital heart disease | 4 |
| Neuromuscular disease | |
| Muscular disease | |
| SMA | 11 |
| Muscular dystrophy | 2 |
| Non-specific myopathy | 5 |
| Myasthenia gravis | 1 |
| Metabolic disease | |
| Mitochondrial disease | 11 |
| Storage disease | 1 |
| D glyceric aciduria | 1 |
| Central nervous system disorders | |
| Hypoxic ischemic encephalopathy | 8 |
| Epilepsy | 4 |
| Cortical dysplasia | 4 |
| Coffin Siris syndrome | 1 |
| Subacute sclerosing panencephalitis | 1 |
| Neuronal ceroid lipofuscinosis | 1 |
| Joubert Syndrome | 1 |
| Eventration of diaphragm | 1 |
| Cervical mass | 1 |
Patients were hospitalized for mean 3 months. Patients receiving neurological and respiratory physiotherapy (cough assisting, percussions and vibrations) constituted 89% of all patients. The mortality rate was lower in this group compared to the patients who did not receive physiotherapy (51% vs. 80%, P < 0.01).
After discharge, 28 patients were admitted to an emergency department on 66 occasions. Fever and respiratory distress were the most common (64%) causes of emergency admissions.
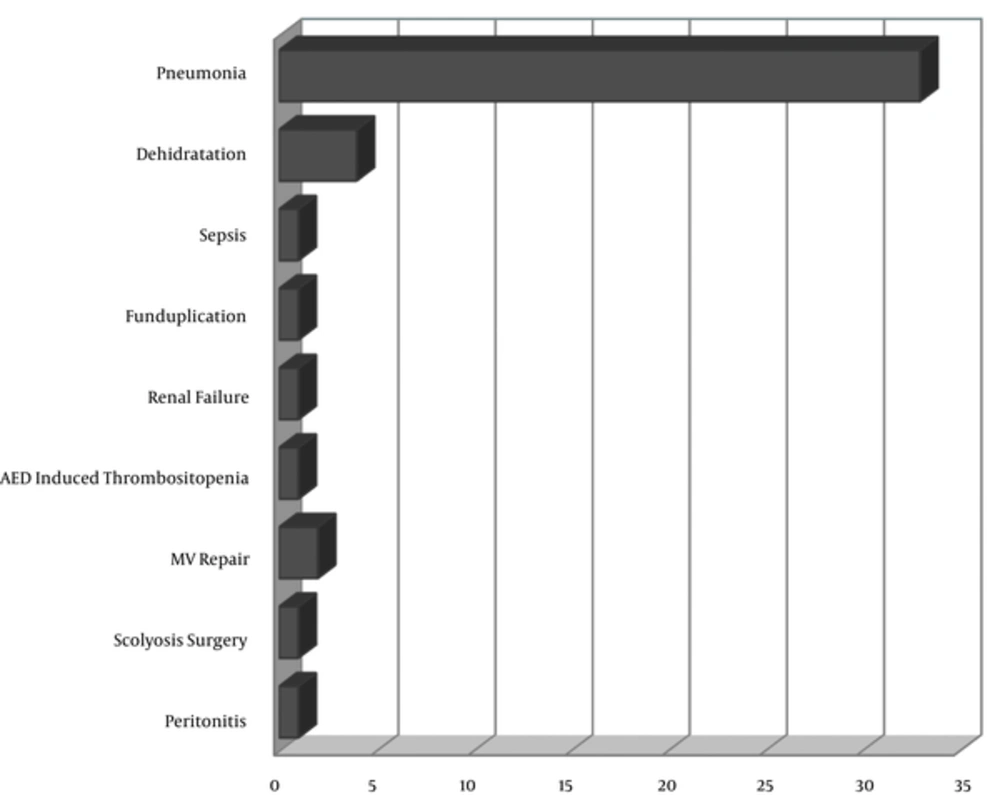
Twenty-three patients (37%) were rehospitalized on 45 occasions. The most common (75%) cause of rehospitalization was pneumonia. Causes of rehospitalization are presented in Figure 1.
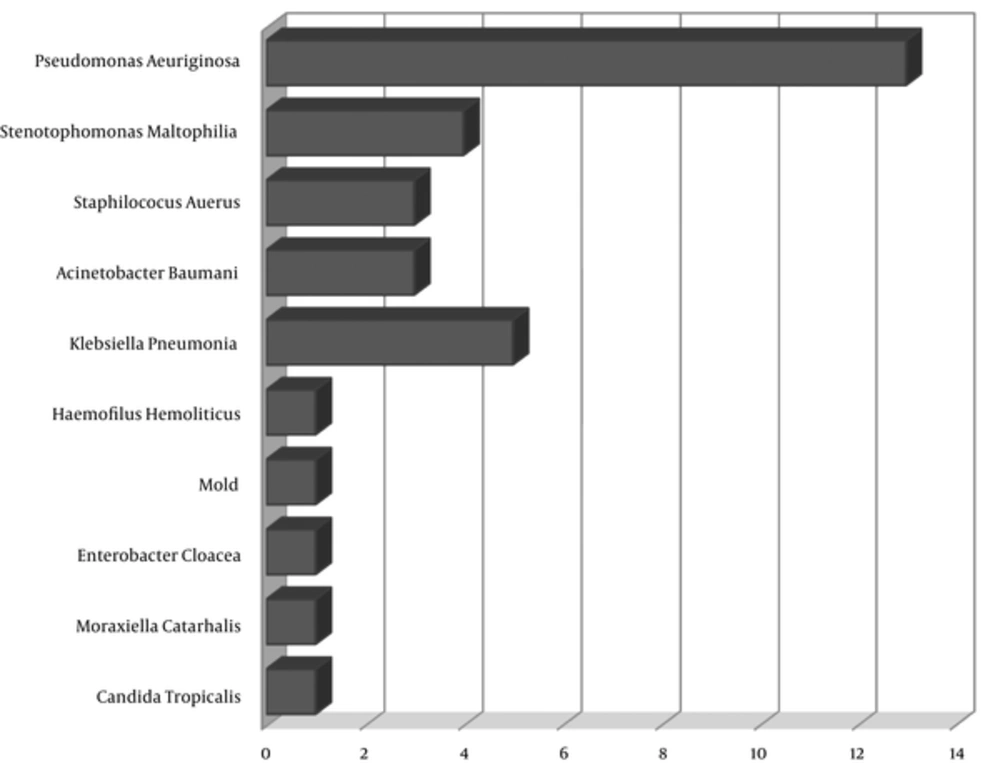
Deep tracheal aspiration (DTA) culture was obtained during rehospitalization due to pneumonia. Thirty three culture growths of various microorganisms were observed during hospitalization (Figure 2). The growth of multiple microorganisms was observed in DTA cultures of 6 patients. The mean hospitalization duration of patients with or without microorganism growth observed was found as 121 days and 69 days, respectively (P = 0.01). The length of hospitalization was extended with the increased growth rate of DTAs. Although the length of stay in hospital leads to an increase in the risk of culture growth among patients, it has no effect on rehospitalization (P > 0.05).
Tracheostomy tubes were changed over 1 - 3 months in 60% of patients. Patients whose tubes were changed in 80 ± 16 days had a higher rate of pneumonia than those with 38 ± 5.6 days in average (P < 0.01), but this did not affect DTA growth (P > 0.05).
The feeding routes of patients after discharge were also investigated. Only 7 patients were fed by oral route. Twenty-five percent of patients who couldn’t be fed by oral route had received gastrostomy tubes and the remaining patients (63%) had received nasogastric tubes. Emergency admissions due to fever (P < 0.05), rehospitalization (P < 0.05) and microorganism growth (P < 0.01) were observed more frequently in patients with gastrostomy tubes compared to patients fed via nasogastric tube.
After discharge, the patients gained weight, and their BMI scores rose to -0.45 from -0.96. Before HMV, 17 patients had a BMI under -2SD, whereas after discharge 7 patients were found to be within normal limits. All malnourished patients except one gained weight.
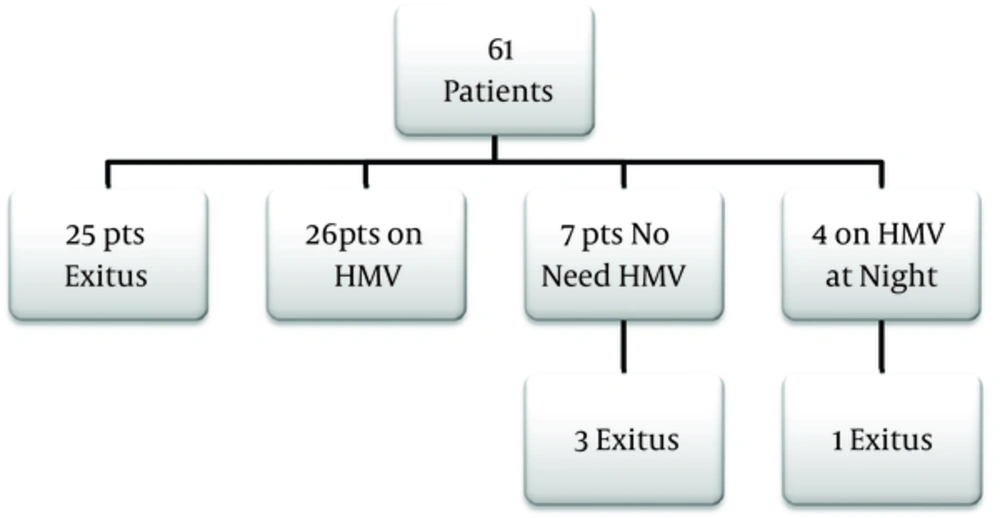
Complications were observed in 21 (46%) patients during follow up. The most common complications included disconnection and ventilator malfunction. Before discharge from hospital these patients were mechanical ventilator dependent the whole 24 hours, after a median of 11 months, there was no further need for HMV in 7 patients, while 4 patients continued to use HMV only at nights. Three patients who discontinued HMV and one patient who needed night ventilation died from primary diseases.
HMV was no longer necessary in 12% of patients ventilated for neurological reasons and 50% for chronic pulmonary diseases. Outcomes of these patients are outlined in Figure 3. Overall mortality rate was calculated as 46.7% including HMV independent patients. Mortality was related to primary disease in 22 (75%) patients, while 7 patients died because of tracheostomy related complications.
4. Discussion
Artificial ventilation efforts have been started for the first time as early as 1541. Today, mechanical ventilators can be used at home owing to the developments in technology. It has been proved since 1970s that these devices can be used at home for medically stable patients suffering from chronic respiratory failure (5). HMV allows patients to go home and grow and develop in their natural environment (6). In the past two decades, more and more patients with chronic respiratory failure have been treated with HMV (7).
In the present study, the most common (94%) diseases leading to chronic respiratory failure were found as central nervous system and neuromuscular diseases with the most common diagnosis being SMA. Prognosis of type 1 SMA is very poor and it is known that 80% of patients die before 12 months of age (8). The most common cause of death in these patients is respiratory insufficiency. In the present study, 18% of the patients were diagnosed with type 1 SMA who are alive at mean age of 6.3 (4, 9 - 12, 6) years. The prognosis of these patients can be improved using HMV support systems.
In our country, there is also an important problem in that, 42% of pediatric intensive care unit beds are occupied by patients requiring chronic medical care, while 24% of these patients are medically stable who can receive supportive treatment at home (9). HMV is a way of discharging these patients from intensive care units.
Gowans and colleagues have reported that the median age of patients on HMV was 6 months in a national survey conducted in Utah (10). Similarly, sixty percent of our patients were under one year of age. This is resulted from HMV requirement emerged in patients with congenital anomalies, metabolic and neurodegenerative diseases early in life. This is also an important warning for commercial institutes that provide home ventilators and ventilators in the market which are suitable for small infants.
Because primary disease was of neurologic origin in 90% of the patients, gastroesophegeal reflux (GER) was found to be the leading (28%) cause of comorbidity. GER may cause complications such as vomiting, esophagitis or aspiration, thus it is a medical condition that must be treated medically or, if necessary, surgically. However, patients with neurological diseases have a higher rate of surgical complications (11). Therefore, it should be performed only on patients who cannot be treated with medical therapy (12).
After the establishment of respiratory support, it is important to solve feeding problems in these patients. Most (63%) of our patients have been fed via nasogastric tube. Feeding through nasogastric tube involves several risks such as aspiration to the airway, aggravation of GER, sinusitis, malposition and obstruction. Although in the present study we found higher rates of emergency admissions, rehospitalization and microorganism growth with the nasogastric tube, it seems to be an association, rather than causation. Gastrostomy must be the first choice for patients who need chronic respiratory support and cannot be fed by oral route. As mentioned above, GER should be investigated before any gastrostomy procedure and should be performed simultaneously in the case of GER fundoplication.
Sixty percent of patients who had lower mortality among all patients were given respiratory physiotherapy by a respiratory physiotherapist and then their parents have been trained by a physiotherapist to be able to give physiotherapy. In concordance with our study, Ntoumenopoulos et al. have reported a decreased incidence of ventilator associated pneumonia in patients who had respiratory physiotherapy (13). This result is supported by Pattanshetty and Gaude in a randomized study conducted in 2010 (14).
Families of our patients have complained about the absence of a specialized team that will help in emergency conditions. In Italy, a specialized team consisting of a nurse, a physiotherapist, a social worker, a pediatrician, and a doctor experienced in ventilation were reported by Rocca. This team is present during education, before discharge, and during follow up of the patients. This team visits patients 27 times a year and evaluates patients 3 times a year in average (15).
The readmission of these patients to hospital is another problem. Patients have been admitted to the emergency department many times, due to fever and respiratory distress. Whereas in a national survey performed in Switzerland, the most common cause of hospital admission was only routine control (16). Foundation of a multidisciplinary team to follow such patients may decrease the emergency department admissions and may solve simple problems at home. Furthermore, rehospitalization due to pneumonia was observed in 75% of cases. Rehospitalization of these patients can be expected because of the severity of their underlying disease, but pneumonia as a reason for hospitalization may be rather due to the insufficient patient care. Education of family members or care givers about tracheotomy care, aseptic precautions during aspiration and monitoring of infectious symptoms is also an important issue.
DTA cultures have been obtained from the patients admitted to hospital with pneumonia. Although patients admitted to hospital were coming from home, microorganisms isolated from DTA cultures of these patients were mostly multi-drug resistant gram negative microorganisms that were used to detect nosocomial infections.
All the patients included in this study were receiving invasive mechanical ventilation support at home and all were ventilated via tracheostomy tube. There is no consensus on the frequency of tube changes for children (17). The advantages of frequent tube changes include decreased airway infection and/or airway granulomas, and reduced incidence of tube occlusion by secretions. On the other hand, possible stretching of the tracheostomy stoma in case of cuffed tracheostomy tubes and patient discomfort are the main disadvantages (17). It is widely accepted that flexible PVC tubes can be used for 3 - 4 months before being changed.
There has been a rapid increase in the growth rate of patients who have received ventilator support due to respiratory failure (17). We demonstrated weight gain and increased BMI values in almost all malnourished patients after discharge. This indicates that HMV helps children to catch up their growth potentials. Sufficient caloric intake must be provided, while keeping carbohydrates below 60% of the daily caloric intake, especially for patients with chronic respiratory failure.
Ventilation requirement may disappear in diseases such as obstructive sleep apnea, bronchopulmonary dysplasia, and chronic respiratory diseases by age (18). Likewise, we observed that 7 patients discontinued 24 hour ventilation and 4 patients required ventilator support only at night. Half of patients with pulmonary diseases discontinued HMV, whereas only 12% of patients with neuromuscular diseases did not require HMV. This is an important data that could be shared with the patients’ families, especially of those with pulmonary diseases, to encourage and motivate them at the time of making decision for HMV. All our patients weaned from home ventilation succeeded as a result of their family’s observation of a decreased need for ventilation support. It is important for the multidisciplinary team that, patients should be supervised during the weaning period in order to minimize any complications and increase the success rate of weaning.
Mortality reported in HMV by Edwards et al. was 20% (19). In our study, this rate was found as 47.7%. The higher rate of mortality compared to the literature was due to the use of HMV for patients with a shorter life expectancy as well as severity of underlying diseases.
4.1. Conclusion
HMV allows discharge of ventilator dependent patients who no longer need hospital care. In this study, we demonstrated that the development and growth of patients with HMV could be maintained in their natural environment. The survival rate and QoL of these patients can be improved by family education concerning any complications encountered at home and the support of nutrition and care rehabilitation programs. A multidisciplinary team should be organized to join follow up of the patients at home.