1. Background
Attention deficit hyperactivity disorder (ADHD) is one of the most common behavioral disorders that is characterized by a persistent and impaired pattern of inattention and/or hyperactivity/impulsivity (1). There are three subtypes of this disorder (combined, inattentive, and hyperactive). ADHD requires more attention due to its high prevalence (2). It has been estimated that ADHD affects 3% to 5% of children of primary school age (3).
Children with ADHD have shown deficiencies in many physical activities in comparison with normally developing children. For instance, children with ADHD perform gross and fine motor control tasks as well as motor coordination worse than typical developing children (4-6). Poor postural control has been also reported in children with ADHD (7). Balance and postural control can be defined as “the ability to maintain the center of mass over the base of sup-port” (8). In other words, Balance is defined as the ability to maintain postural stability while standing and in motion.
Over the last decade, some researchers have examined the balance ability in children with ADHD. Their results have shown that children with ADHD have significantly less balance control than children without ADHD (5, 9-13). Mao et al. (14) demonstrated that children with ADHD had a weaker performance in mechanical horseback riding and the balance subdivisions of the movement assessment battery for children (MABC) and the Bruininks-Oseretsky test of motor proficiency (BOTMP) task compared to children without ADHD.
In relation to the various effects of exercise training in children with ADHD, Verret et al. (15) examined the impact of 10-week physical activity program on behavioral and psychological functions of children with ADHD. The researchers concluded that exercise training improved muscular capacity, motor skills, behavior, and cognitive functions in children with ADHD. In a systematic review and meta-analysis, Cerrillo-Urbina et al. (16) explored that short-term aerobic exercise interventions had a positive effect on attention, hyperactivity, impulsivity, anxiety, executive function, and social disorders of ADHD children.
Children with ADHD compared to normally developing children are more likely to be injured in physical activities (17). Furthermore, Balance is a fundamental necessity for sports, daily activities, and protection from injury (18). With regard to balance disturbance in children with ADHD, improving balance probably can help these children in many activities. Previous studies have not investigated the effect of a physical activity program on the balance of these children.
2. Objectives
Therefore, the present study investigated the effects of specific balance training on postural control in children with ADHD. Having considered the studies discussed above, the present study sought to answer this question: can the balance training improve the postural control of these children?
3. Methods
3.1. Participants
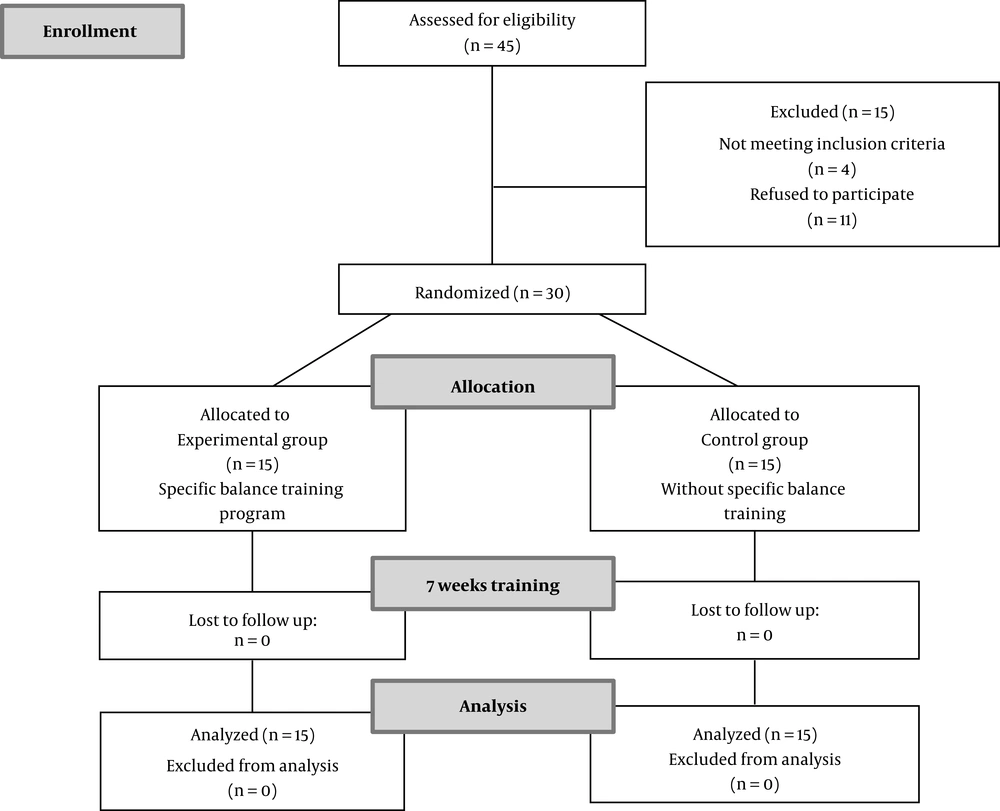
The study consisted of 30 male children with ADHD (8.58 ± 0.93 years old) who were also diagnosed with ADHD-C (combined type) in the Pediatric Neurology Clinic. Inclusion criteria included having ADHD based on the clinic approval, the age range of 7 to 10 years, normal intelligence and educational status. Participants who were diagnosed with specific conditions such as nervous system malfunction, impaired hearing, vertigo, prior surgical operations, or head injury were excluded from the study since these conditions could potentially affect balance performance. Children with other disorders such as developmental coordination disorder (DCD), learning disorders, autism, and intellectual disabilities were also excluded from the study. The sample size was calculated using G*Power software, and it was assumed α = 0.05 and (1-β) = 0.95. Based on the results, 15 children were assigned to a participant blinding method for each group (experimental and control). Figure 1 shows a CONSORT flow diagram of participants through the intervention. Before the study began (in the briefing session), parents signed informed consent forms in accordance with the procedures approved by the Ethics Committee of Arak University of Medical Sciences (no.: IR.ARAKMU.REC.1398.013).
3.2. Procedure
Before any intervention began, the participants were instructed on how to perform the test in a briefing session. The participants did warm-up exercises and were then trained on how to stand on the balance test system. Afterward, all participants took both static and dynamic balance tests. To assign participants to training groups, matched random sampling was used. According to this method, participants were first matched according to their pre-test scores and then randomly assigned into an experimental and a control group, each comprising 15 members. The experimental group participated in seven weeks of a specific training program (the training protocol is presented in the next section) conducted three times a week on every alternate day under the supervision of two experienced coaches at the school. The control group did not engage in any exercise over the seven-week period but continued to practice normal activities. Participants did not attend any physiotherapy or occupational therapy sessions. Every training session lasted about one hour and consisted of 10 minutes of warm-up, 10 minutes of stretching exercises, 30 minutes of select balance training, and 10 minutes of cool-down. After the completion of the training program, both groups participated in the posttest, whereby the static and dynamic balance was measured across the three indices. All tests were performed under the guidance of a therapist. A similar protocol has been used in previous studies (15).
3.3. Training Protocol
Training focused mainly on specific postural control and balance exercises. The balance-training program consisted of static and dynamic training such as standing movements (swinging the arms back and forth together rhythmically, bending and straightening the knees), standing on one leg (on the floor and the foam step), walking (in straight lines, for-ward and backward, then along curves and then with abrupt changes of direction, through the space made by two facing benches), walking on the rope (first with open eyes and then with closed eyes), walking on the balance beam with open hands, standing on the balance board with closed and open eyes, jumping on the hula hoop rings with one leg and two legs, training with a Swiss ball (for example: sitting on the Swiss ball, single leg supine bridge, abdominal crunch and so on), rolling, walking, hopping, skipping, galloping, jumping, and some balance games to increase variety in training sessions. Such training has also been used in previous studies (19). Each child performed all these exercises in one session. During these sessions, the above mentioned exercises were presented in a variety of ways and forms of the games so that the children would be more willing to perform. Due to the age of children and the research conditions, progressive exercises were not used.
3.4. Postural Outcome Measure
Postural sway was measured using the Biodex balance system. The rotating platform moves in anterior-posterior and mediolateral directions. The rotation of the platform exposes the participants to variable surfaces, which helps researchers examine dynamic postural control in the participants (20). The stability of the surface may be adjusted from state 1 (the most unstable state or dynamic state) to state 12 (most stable state or static state). In this study, the stability of the surface was set at state 1 and state 12 based on initial measurements. The test included 3 attempts, each taking 20 seconds with 10-second intervals between attempts. The system calculates the stability index at the end of the test (21). The large postural sway indicates a poor balance. The measurements of the Biodex balance system were obtained for three indices, the anteroposterior stability index (AP), the mediolateral stability index (ML), and the overall index (OV).
3.5. Data Analysis
For analysis of data, we used the Kolmogorov-Simonov test for normality of data at baseline. We used independent t-test to compare the characteristics of children with ADHD and controls at baseline. To compare the participants’ performance in pre- and post-test, two groups (experimental vs control) × two postural conditions (stable/unstable) × two test conditions (pre- and post-test) mixed design ANOVA was used. Before these analyses, we carried out Mauchly’s test of sphericity. We also used eta-squared to calculate effect sizes. Statistical significance was set at P < 0.05.
4. Results
Table 1 describes the characteristics of the participants.
| Characteristic | Children with ADHD (N = 15) | Control Group (N = 15) | P Value |
|---|---|---|---|
| Age, y | 8.07 ± 1.03 | 8.13 ± 1.30 | 0.87 |
| Height, cm | 125.5 ± 10.12 | 124.6 ± 9.24 | 0.79 |
| Weight, kg | 24.73 ± 4.39 | 23.73 ± 4.21 | 0.53 |
| BMI | 16.41 ± 3.23 | 15.86 ± 1.33 | 0.21 |
| IQ | 98.8 ± 9.39 | 95.9 ± 9.99 | 0.41 |
| Educational status | 18.93 ± 0.70 | 19 ± 0.77 | 0.80 |
Abbreviations: BMI, body mass index; IQ, intelligence quotient.
aValues are expressed as mean ± SD.
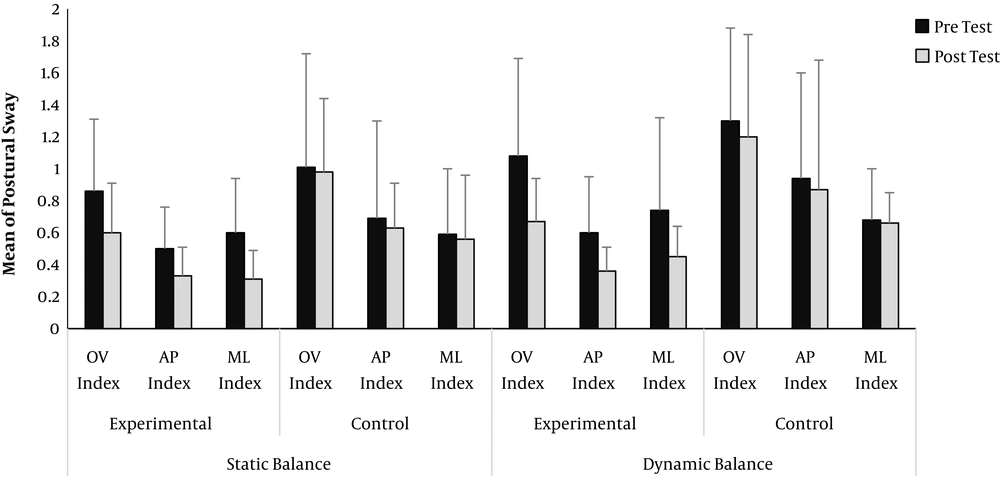
Table 1 shows that the participants in the two groups did not have significant differences in their characteristics. Figure 2 shows the mean performance of the postural sway of two groups in the pretest and posttest in three indices.
Figure 2 shows that the postural sway of the experimental group have decreased in the post-test. After confirming the normality of the data, the mean scores of balance overall index in the pre- and post-tests were analyzed with mixed design ANOVA. In overall index of balance (OV), the results showed that the practice sessions had a significant main effect, F (1, 28) = 17.19, P = 0.001, η2 = 0.38, and postural condition, F (1, 28) = 4.94, P = 0.03, η2 = 0.15. Also, there was a significant interaction effect between the groups and test condition, F (1, 28) = 12.28, P = 0.002, η2 = 0.30). The main effect of the group was also significant, F (1, 28) = 7.80, P < 0.0019, η2 = 0.21. These results showed that in the overall index (OV) the performance of the experimental group was significantly better than the control group. In other words, the training protocol improved the OV index of balance in the experimental group during the practice sessions.
In anteroposterior stability index (AP), the results showed that the practice sessions had a significant main effect, F (1, 28) = 8.20, P = 0.008, η2 = 0.22. These results indicate that the training protocol improved the AP index of balance in the experimental group during the practice sessions. The main effect of the group was also significant, F (1, 28) = 5.48, P = 0.02, η2 = 0.16. These results also showed that in the anteroposterior stability index (AP) the performance of the experimental group was significantly better than the control group.
In mediolateral stability index (ML), the results showed that the practice sessions had a significant main effect, F (1, 28) = 7.12, P = 0.01, η2 = 0.20, and postural condition, F (1, 28) = 4.12, P = 0.04, η2 = 0.14. Also, there was a significant interaction effect between the groups and test condition, F (1, 28) = 8.16, P = 0.008, η2 = 0.22. These results indicate that the training protocol improved the ML index of balance in the experimental group during the practice sessions.
5. Discussion
The present study investigated the effects of balance specific training on the postural control of children with ADHD. The results showed that the training protocol improved the static and dynamic balance in children with ADHD compared to the pretest. In other words, in all three indices (overall, anteroposterior, and mediolateral), the experimental group outperformed the pre-test in the post-test. In addition, the performance of the experimental group in dynamic and static balance in the post-test was better than the control group.
The most important finding of this study was that the specific balance training improved static and dynamic balance of ADHD children. In other words, the use of balance training in the form of the game had a significant effect on the balance of these children. For example, one of our exercises was using a Swiss ball. In this regard, researchers argue that balance training, especially training on moving surfaces (such as a Swiss ball), can have a positive effect on postural and balance control. For example, Cug (22) examined the effect of practicing with Swiss balls and showed that such training significantly enhanced balance. Considering that previous studies have shown that there are disturbances in the parts of the cerebellum in children with ADHD (23, 24), damage to these parts leads to weakness in balance and postural control (14), muscle stiffness, and uncoordinated movements (25). Balance exercises (e.g., standing on one leg, walking on the balance beam with open hands, standing on the balance board with closed and open eyes, jumping on the hula hoop rings with one leg and two legs, training with a Swiss ball, etc.) are likely to improve the balance of children with ADHD.
There are several reasons why children with ADHD have poor balance control. Shorer et al. (11) attributed the problem of balance in ADHD children to the increased threshold for identifying postural sway by peripheral sensory receptors and cerebral dysfunction. Different cerebellar regions have important roles in motor control, balance, walking, and motor coordination (26). Some studies stated that low cerebellar volume in children with ADHD compared to healthy children is a probable reason for the lack of balance in these children (27, 28). Neuroimaging studies have pointed to abnormalities of the brain parts, such as the prefrontal cortex and Basal ganglia, which can lead to weaker sensory motor control and processing (23, 24, 29). These disorders can affect the balance of children with ADHD, because balance control is influenced by the neuromuscular system and related sensory systems, such as the somatosensory, vestibular, and visual systems (30). In this research, we used a balance specific training protocol, which has not been used in previous studies. For example, Verret et al. (15) used an aerobic, muscular, and motor skills exercise program protocol. The results of this study showed that the use of balance exercises in a more complete protocol, and the involvement of sensory sys-tems in children with ADHD are essential.
5.1. Conclusions
The results of this study indicate that balance training can improve the balance of children with ADHD. It is possible that using balance exercises in the form of games and in leisure time will contribute to the postural control and balance of children with ADHD.
5.2. Research Limitations
This study had some limitations. It is probable that participants in the groups, despite the researchers’ emphasis, participated in training programs outside the exercise protocol, which was out of the control of the researchers. In the future it may be interesting to explore further the effect of balance training in other motor capabilities, as fine coordination skills and function (as suggested by the International Classification of Functioning, Disability and Health) in the children with ADHD. Furthermore, well design case-control studies are requested to ensure the scientific validity of the balance training program and delineate the optimal protocol; for instance it will be necessary to increase the number of children with ADHD tested and to add a group of normally developing children for a corrected comparison.