1. Background
Ovarian torsion is a rare condition in girls that lacks a specific symptom, which delays diagnosis. The prevalence of ovarian torsion is about 2.7% in patients with acute abdominal pain and 4.9 in 100,000 people in the general population (1, 2).
Because the ovary has a gangrenous appearance and its color changes, oophorectomy is the recommended surgical procedure in most cases. However, since 1946, scattered research has been conducted on ovarian preservation in ovarian torsion with promising results and it was believed that even in the presence of dark and nonviable ovary it can be preserved (3).
2. Objectives
Since this organ has a significant role in producing hormones and fertility in women, this study was conducted to evaluate the effectiveness of ovarian preservation without oophorectomy in pediatric age group and careful follow-up of the operatively treated patients.
3. Methods
The study population consisted of all girls below 18 years old who underwent laparotomy in Children’s Medical Center, Tehran, with a diagnosis of acute abdomen from January 2017 to August 2018, in whom an ovarian torsion was suggested. The level of the tumor marker was measured in all patients before surgery. All subjects underwent ovarian detorsion and fixation to the posterior abdominal wall and biopsy specimens were obtained for histopathological evaluation. All the parents were informed about the study and informed consent was obtained from them. Conventional and Doppler sonographies were done three months later to follow up the patients.
The data were analyzed with the SPSS software according to the study objectives. Descriptive statistics are presented as absolute and relative frequency for qualitative variables and mean and standard deviation for quantitative variables. To compare the data and extract causal relationships, t-test and Mann-Whitney were used for quantitative variables if the data were distributed normally and non-normally respectively, and chi square test was used for qualitative variables.
4. Results
During 20 months from January 2017 to August 2018, eighteen patients with a diagnosis of ovarian torsion underwent surgery. The age range of the patients was 4 - 13 years with a mean age of 8.1 years. Four cases (23.5%) were below 5 years, 7 patients (41.2%) were 5 - 10 years, and 6 patients (35.3%) were above 10 years.
The tumor marker level was measured in all patients before the operation, and patients with abnormal levels were excluded from the study. The preoperative tumor marker level was abnormal in only one patient in whom pathological evaluation showed malignancy after surgery. This patient was excluded from the study and analysis was done on the remaining 17 patients.
The patients’ symptoms included abdominal pain (n = 17, 100%), vomiting (n = 15, 88.2%), nausea (n = 2, 11.8%), and fever (n = 1, 5.9%). The duration of the symptoms was 1 - 3 days (mean = 2.11 days).
All patients underwent ultrasound examination, which resulted in the diagnosis and surgical treatment in 14 cases (82.4%). Sonography did not help with diagnosis in three patients (17.6%) and imaging was carried out with CT scan.
Of 17 torsion cases, 6 (35.3%) were on the left side and 11 (64.7%) on the right side. The size of the cyst ranged from 6.5-8 cm (mean = 5.97 cm) on ultrasound and 4 - 9 cm (mean = 6.35 cm) according to intraoperative measurements, indicating no significant difference (P value = 0.069).
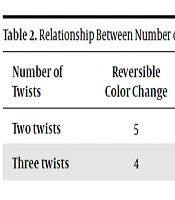
Of 17 torsion cases, 8 (47.1%) had two twists and 9 (52.9%) three twists. Nine cases (52.9%) had reversible color change within 10 minutes after detorsion and warming and 8 cases (47.1%) showed irreversible color change. The mean duration of surgery was 47.6 minutes (range = 30 - 90 minutes).
The patients had no postsurgical complications and were discharged within 2 - 4 days (mean = 2.29 days).
All patients underwent control sonography (conventional and Doppler) three months after the operation, which showed ovarian tissue with good arterial flow in 15 cases (88.2%). The ovaries were not detected in two patients (11.8%). Table 1 shows the relationship between the cyst size and number of twists using Student t-test.
| No. (%) | P Value | ||
|---|---|---|---|
| Cyst < 5 cm | Cyst > 5 cm | ||
| Two twists | 3 (17.6) | 5 (29.4) | 0.669 |
| Three twists | 3 (17.6) | 6 (35.29) | 0.665 |
The results showed no significant correlation between the duration of symptoms and intraoperative findings (P value = 0.23). Table 2 presents the relationship between number of twists and intraoperative findings.
| Number of Twists | Reversible Color Change | Irreversible Color Change | P Value |
|---|---|---|---|
| Two twists | 5 | 3 | 0.25 |
| Three twists | 4 | 5 |
Because of lack of reports on the size or volume of the ovary on pre-operative ultrasound, we compared the volume of the affected ovary in addition to Doppler ultrasound findings with the healthy contralateral ovary (Table 3).
| Number | Mean | P Value | |
|---|---|---|---|
| Volume of affected ovary (operated on) | 17 | 2.42 | 0.014 |
| Volume of healthy ovary | 17 | 3.17 |
There was a significant difference in volume between the healthy and affected ovaries (P value = 0.014), which resulted from not visualizing two ovaries on ultrasonography. After excluding these two cases, a P value of 0.0001 was obtained, indicating that the preserved ovary could reach its appropriate volume for age in three months.
Finally, it should be mentioned that all cases of ovarian torsion were fixed to the posterior abdominal wall after detorsion and there were no cases of recurrence. Moreover, a wedge biopsy was obtained from each ovary during the operation, which, except one case (5.9%) with a report of dysgerminoma, all included benign cysts including benign cystadenoma (n = 1), hemorrhagic cysts (n = 13), premature teratoma (n = 2), and benign mucinous cyst (n = 1).
5. Discussion
Ovarian torsion is a rare condition in girls with no specific symptoms, causing a delay is diagnosis. It should be differentiated from appendicitis, renal calculi, mesenteric lymphadenitis, gastroenteritis, and ectopic pregnancy (4, 5).
Since ovarian torsion is a surgical emergency, it should be taken care of immediately. The most common symptom is lower abdominal pain (6). Nausea and vomiting, mild fever, and leukocytosis are other signs and symptoms. The best diagnostic modality so far is color Doppler ultrasound of the ovarian vasculature.
The first diagnostic step, which is inexpensive and readily available with little radiation exposure, is ultrasound, which has a sensitivity of 82.4% for ovarian torsion according to the results of this study that is consistent with the sensitivity reported in other studies (50% - 75%). On the other hand, there was not much difference between the ultrasound report of the ovarian size and intraoperative findings, indicating the precision of ultrasound results.
In this study, the odds of torsion were higher for the right ovary (64% versus 35%), which is consistent with the literature and is due to the presence of the sigmoid colon on the left side. Moreover, as for the tumor marker, there was consistency between the tumor marker result and pathology report in 16 out of 17 cases (94%). Therefore, it could be concluded that this tumor marker helps surgeons make better decisions.
The results of this study showed no correlation between the cyst size and number of twists. However, from a clinical point of view, larger cysts were prone to more twists, requiring for a prompt action. This clinical and statistical difference may be the result of the small sample size of this study; the literature indicates too, that the larger the cysts, the higher are the odds of torsion.
According to intraoperative observations of the surgeon and his assessment of the extent of necrosis, severe discoloration was seen in 8 cases, which did not improve after detorsion and warming. However, only two (25%) of these ovaries were not visualized on control sonography, indicating that the surgeon’s intraoperative assessment of the extent of necrosis is not an accurate criterion for the removal of ovaries and ovarian preservation should be considered with any level of color change. Several studies have also shown the effectiveness of detorting ischemic ovaries (1, 7). ACOG committee opinion about adolescents’ adnexal torsion is saving the torsed ovary except for severely necrotic ones (8).
Unfortunately, there was no report of the size or volume of the affected ovaries on preoperative sonography for comparison with postoperative size and volume. However, postoperative comparison of the volume of the affected and contralateral healthy ovary showed no significant difference in size; moreover, Doppler sonography was also unremarkable, indicating that the affected ovary can continue its normal growth after detorsion.
Another important finding of this study was lack of any correlation between the duration of symptoms and intraoperative findings, which are consistent with the hypothesis that tissue changes in torsion may occur in less than 2 hours. This can be due to torsion de-torsion process (that sometimes occurs spontaneously) or recirculation after de-torsion. Furthermore, no correlation was found between the number of twists and intraoperative findings, indicating that ovarian artery compression has no relationship with the number of twists and cannot serve as a criterion for making decisions for surgery. However, it seems logical to assume that a larger number of torsions increases the odds of arterial compression.
An important point is to obtain biopsy samples from the affected ovary during surgery, because there are reports of the cystic ovarian involvement in ovarian malignancies (its prevalence of 5.9% in this study).
In this approach, the patients undergo control Doppler ultrasound for blood flow assessment and conventional sonography for ovarian size assessment three months after the operation. However, different follow-up durations are reported in the literature (9). In this study, since most of the patients were from long distances and several long-term follow-ups were not possible, the mean duration of the follow-ups reported in the literature, i.e. three months, was selected.
Another point in this study was oophoropexy, which has not been studied extensively (10-12). Oophoropexy was done as part of the surgical procedure in this study and the affected ovary was fixed to the posterior abdominal wall. There was no report of torsion recurrence in our patients. There were also no cases of abscess formation on postoperative assessments that is in line with the literature. Therefore, the surgeon should not abandon ovarian preservation for fear of abscess formation in the future.
A limitation of this study was the low prevalence of ovarian torsion in the general population and therefore in girls below 18 years, resulting in a small sample size. Therefore, it is recommended that these studies be conducted in several centers. Moreover, some patients did not return for follow-up due to the long distance or lack of knowledge about its importance; these patients were encouraged to return for follow-up through repeated phone calls and reminding its importance.
5.1. Conclusions
Ovarian preservation after detorsion is a safe approach to treatment of ovarian torsion in children. However, long-term follow-up is necessary to determine the status of fertility. If the contralateral ovary is healthy and intact, no definite conclusion can be drawn on the normal function of the involved ovary.