1. Background
For pediatric population, abdominal pain is a common complaint in the emergency department (ED) (1). Abdominal pain was reported up to 6.2% of all pediatric emergency admissions (2). The most common etiology of acute abdominal pain in pediatric patients is acute appendicitis (3).
Diagnosis of the appendicitis is still controversial, and unfortunately clinicians have problems to arrive at a definitive diagnosis in adult and pediatric populations, even in perforated appendicitis (4). History and physical examination are still in the first line, but laboratory tests and imaging modalities are of great importance (5), because especially younger children have limitations in expressing themselves. Complete blood count (CBC) is in the first line of laboratory evaluation to diagnose appendicitis (6, 7). White blood cell count (WBC) is studied well in the literature, but recently, there are several CBC parameters such as red blood cell distribution width (RDW), mean platelet volume (MPV), and platelet distribution width (PDW) associated with the diagnosis of appendicitis (8-11). In recent studies, neutrophil-to-lymphocyte ratio (NLR) is reported associated with several surgical clinical conditions as appendicitis, acute mesenteric ischemia, and strangulated inguinal hernia (12-14).
2. Objectives
The current study aimed at evaluating the diagnostic value of NLP to diagnose acute appendicitis in the pediatric patients with abdominal pain.
3. Methods
The current retrospective, descriptive study was approved by local ethical committee and all procedures were performed according to Helsinki declaration. Hosting hospital was a tertiary health care setting with annual pediatric emergency visit of 150,000 cases. All data were collected retrospectively from the hospital database records.
Patients under 18 years old undergone appendectomy from January 1, 2012 to December 31, 2013 were screened for eligibility. Descriptive data including age, gender, and hospitalization time were recorded. Initial white blood cell count (WBC), hemoglobin (Hgb), hematocrit (Hct), platelet count (Plt), neutrophil count, and lymphocyte count were recorded as complete blood count (CBC) parameters at presentation. C-reactive protein (CRP) and fibrinogen were recorded as other acute inflammatory markers. As the gold standard of the diagnosis, histopathologic examination reports were recorded and accordingly, patients were divided into acute appendicitis (AA) and non-appendicitis (NA) groups.
All patients with sufficient data were included in the study. Exclusion criteria were age ≥ 18 years, abdominal trauma, lack of enough data, having additional diseases affecting hematologic system (including lymphoma, leukemia, and bone marrow malignancies), or other chronic inflammatory diseases (including tuberculosis, Henoch-Schönlein purpura), and any autoimmune disorders.
CBC was performed with ABX Pentra XL 80 hematology analyzer (Horiba Instruments Inc., California, USA) as a routine process in the hosting facility. But, NLR was calculated for each subject via dividing neutrophil count to lymphocyte count.
3.1. Statistical Analysis
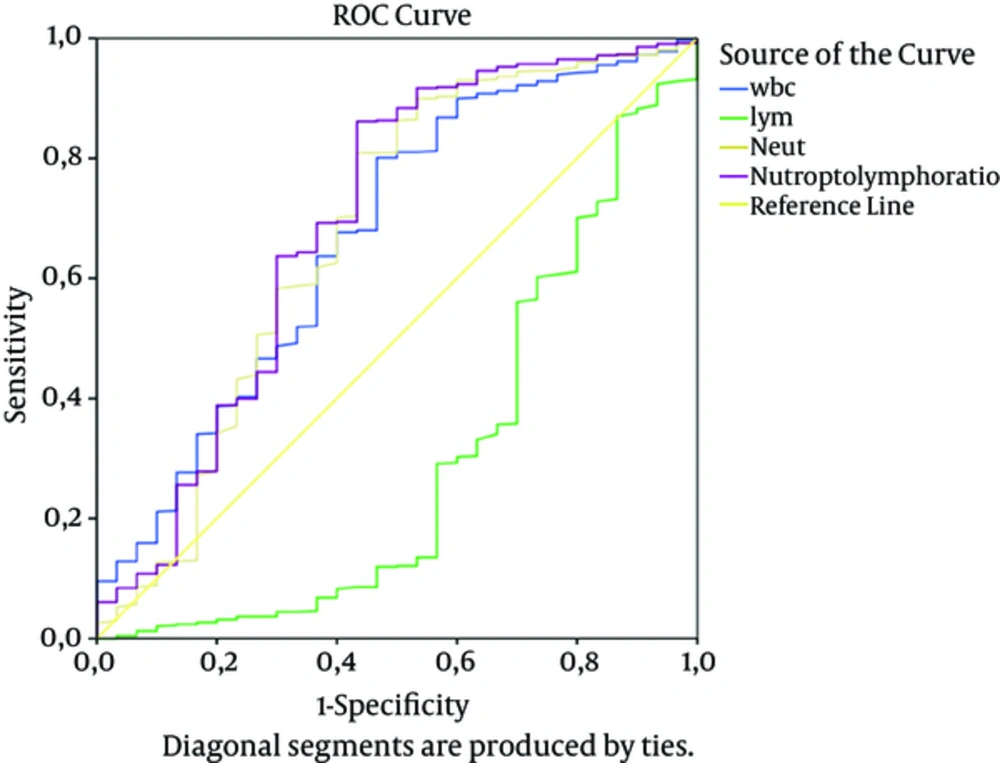
Frequency was used to present descriptive statistics for categorical variables. Mean ± standard deviation (SD) was used to express continuous data with normal distribution. Primary and secondary data were compared by Chi-square test and the Student t test in the acute appendicitis and non-appendicitis groups. To assess the diagnostic utility of the studied parameters on acute appendicitis, receiver operating characteristic (ROC) curve analysis was performed. Statistical Package for the Social Sciences (SPSS) version 15.0 (SPSS Inc., Chicago, IL) was employed for statistical analyses, and a P < 0.05 was considered as statistically significant.
4. Results
During the study period, a total of 658 patients met the inclusion criteria. In the AA group, there were 628 patients with a mean age of 11.35 ± 3.68 years; in the NA group, there were 30 patients with a mean age of 11.23 ± 4.64 years. There was no difference between the 2 groups regarding age, gender, and hospitalization time (P = 0.872, 0.182, and 0.713, respectively).
WBC was elevated in both groups, but it was higher in the AA group (15.94 ± 7.07×103 /mm3) than the NA group (12.66 ± 4.81×103/mm3) (P = 0.012). Lymphocyte counts were significantly lower and neutrophil counts significantly higher in the AA group than the NA group (P < 0.001 for both). NLR was also significantly higher in the AA group than the NA group (P = 0.008). Hgb, Htc, RDW, MPV, platelets count, fibrinogen, and CRP levels did not show any difference between the 2 groups (P = 0.248, 0.420, 0.929, 0.498, 0.148, 0.253, and 0.227, respectively) (Table 1).
| Variables | Non-appendicitis Group (n = 30) | Appendicitis Group (n = 628) | P Value |
|---|---|---|---|
| Age | 11.23 ± 4.64 (-1.48 - 1.25) | 11.35 ± 3.68 (-1.87 - 1.64) | 0.872b |
| Gender (female/male) | 13/17 | 199/429 | .182c |
| Hospitalization time, day | 3.97 ± 2.29 (-0.89 - 1.31) | 3.76 ± 2.99 (-0.69 - 1.11) | 0.713b |
| WBC, ×103 /mm3 | 12.66 ± 4.81 (-5.85 - -0.72) | 15.94 ± 7.07 (-5.15 - -1.41) | 0.012b |
| Lymphocyte, % | 24.72 ± 22.68 (8.34 - 16.08) | 12.51 ± 9.61 (3.71 - 120.71) | < 0.001b |
| Neutrophil, % | 70.28 ± 16.51 (-14.09 - -4.77) | 79.71 ± 12.51 (-15.66 - -3.20) | < 0.001b |
| NLR | 6.48 ± 6.58 (-6.40 - -0.97) | 10.16 ± 7.44 (-6.20 - -1.16) | 0.008b |
| Hemoglobin, mg/dL | 12.69 ± 1.32 (-0.82 - 0.21) | 12.99 ± 1.41 (-0.81 - 0.19) | 0.248b |
| Hematocrit, % | 4.08 ± 0.75 (-2.32 - 0.97) | 4.50 ± 0.18 (-2.24 - 0.89) | 0.420b |
| RDW, % | 13.92 ± 1.34 (-0.36 - 0.39) | 13.91 ± 1.02 (-0.49 - 0.52) | 0.929b |
| MPV, fL | 7.51 ± 0.95 (-0.46 - 0.22) | 7.63 ± 0.92 (-0.48-0.25) | 0.498b |
| Platelet, ×103 /uL | 325.83 ± 118.44 (-8.65 - 57.43) | 301.44 ± 88.51 (-20.32 - 69.10) | 0.148b |
| Fibrinogen, mg/dL | 123.41 ± 156.87 (-256.40 - 67.73) | 217.75 ± 215.61 (-239.80 - 51.14) | 0.253b |
| CRP, mg/dL | 150.98 ± 567.97 (-2023.84 - 482.05) | 921.87 ± 3184.71 (-1121.15 - -420.63) | 0.227b |
Abbreviations: CI, Confidence Interval; CRP, C-Reactive Protein; MPV, Mean Platelet Volume; NLR, Neutrophil-to-Lymphocyte Ratio; RDW, Red Cell Distribution Width; SD, Standard Deviation; WBC, White Blood Cell Count.
aValue are expressed as Mean ± SD, (95% CI).
bThe Student t test for independent samples.
cChi-square test.
ROC curves are given in Figure 1, and AUC values for WBC, neutrophil ratio, lymphocyte ratio, and NLR were 0.669, 0.675, 0.300, and 0.694, respectively. According to ROC curves, cutoff value of NLR was 3.5. Sensitivity, specificity, positive likelihood ratio, negative likelihood ratio, positive predictive value, and negative predictive value were 84.2%, 56.7%, 1.94, 0.28, 97.6%, and 14.7%, respectively according to a cutoff value of 3.5 for NLR.
5. Discussion
The result of the current study indicated that higher NLR levels may be a good marker in the diagnosis of acute appendicitis in pediatric population. Although WBC, neutrophil count, and lymphocyte count seem beneficial as a calculated value, NLR increased the individual diagnostic significance of the neutrophil and lymphocyte counts.
In a retrospective study, Kucuk et al. reported that NLR could be useful to diagnose adult patients with acute appendicitis. Their data suggested that the cutoff value of NLR was 1.71:1 to diagnose acute appendicitis with a sensitivity of 97% and specificity of 87% (15). Their data also suggested that NLR increased the AUC values compared to individual neutrophil count and lymphocyte count. Markar et al., reported similar data in their study on adult patients with appendectomy. Their cutoff value for NLR was 6.0 with a sensitivity and specificity of 71% and 80%, respectively (16); and their data were compatible with those of the current study supposing the increased diagnostic accuracy of NLR compared to its determinants.
Besides the diagnosis, NLR was reported valuable to predict severity of the AA. Yardimci et al., found that NLR levels were higher in patients with complicated appendicitis in adult population. With a cutoff value of 7.95, NLR was detected in the cases with complicated appendicitis, with a sensitivity and specificity of 78% and 67%, respectively (17). Kahramanca et al., reported the cutoff value of NLR to diagnose the AA as 4.68, but in the same study, as a subgroup analysis, NLR showed a good performance to differentiate between complicated and non-complicated appendicitis with a cutoff value of 9.85, supposing that the higher NLR, the higher complication rates (18). Timing of appendectomy is sometimes controversial, especially in pediatric patients. Although there are no data on pediatric patients, NLR can be useful to monitor the subjects with acute appendicitis.
In their retrospective cohort study, Kelly et al. compared the adult and pediatric patients who underwent emergent appendectomy. According to their data, NLR was a good indicator to predict severity of appendicitis and estimate the length of the stay time; cutoff value was higher in the pediatric population (7.53, sensitivity: 80%, specificity: 55%) compared with that of the adults (6.35, sensitivity: 85%, specificity: 48%) (19). The current study did not evaluate the severity of appendicitis, but there was no difference in the length of stay between the AA and NA groups.
Yazici et al., retrospectively evaluated pediatric patients who underwent appendectomy and compared different cutoff values for NLR. According to their data, a cutoff value of 3.5 seems valuable (sensitivity: 90%, specificity: 88%) to diagnose AA in pediatric patients (20). Their results were consistent with the current study data, supporting the reliability of NLR to diagnose acute appendicitis.
Not only diagnosis, but also exclusion is important. Wang et al., reported that absence of the left shift had a negative predictive value of 90% to exclude appendicitis in the pediatric patients with non-traumatic abdominal pain (21). The current study data showed a negative predictive value of 14.7% in the pediatric population with appendicitis. However these 2 studies had distinct results; Wang et al., assessed left shift as a categorical (yes/no) value, but the current study results were based on continuous data.
NLR was reported valuable in the outcome prediction of postoperative phase in the elderly with a higher cutoff value (22.85) than adult and pediatric populations. But, with this cutoff point, NLR was reported as an independent factor in the 30-day postoperative mortality estimation of the elderly (22). The current study did not have a follow-up period and therefore, it could not assess the mortality or outcomes.
5.1. Limitations
It was a retrospective study and randomization was not performed. Complications were not recorded specifically. There was a limited number of subjects in the control group.
5.2. Conclusion
The current study demonstrated that NLR seems a valuable marker to diagnose acute appendicitis in the pediatric population. Despite the high-tech modalities, as a simple test, CBC is still of great importance to evaluate abdominal pain. Physicians should assess as many different clues as possible, and NLR seems to become increasingly important.