1. Background
Acute kidney injury (AKI) is a difficult prevalent disease that accounts for approximately 50% of consultations with nephrologist (1). The incidence is highly dependent on the setting, hospital vs. community acquired AKI. The severity and duration of AKI predicts its outcome (2). Although it is more prevalent in PICU; the new concern is medication associated AKI in non-ill children (3). After high nephrotoxic drug exposure residual damage and chronic kidney disease (CKD) have been demonstrated in two thirds of AKI patients after six months follow up (4).
AKI is also associated with longer hospitalization time, higher rate of mortality, and increased risk of chronic kidney disease in adulthood. As such, early diagnosis and treatment can potentially improve the outcome (5, 6). Unfortunately early distinction between functional and structural AKI is difficult on the basis of clinical findings and conventional laboratory parameters such as urine output, urine osmolality, fractional excretion of sodium, BUN to Cr ratio, urine sediment, etc. (7). The aim of a number of studies was to find more sensitive biomarkers to recognize AKI in the earliest stage. Biomarkers rise in different time-points of the kidney injury and each biomarker individually will not perform well in various types of AKI (8-10). Although a panel of all biomarkers perform the best to detect AKI in early or different stages; the present study was designed by emphasis on random measurement of a single biomarker. All new biomarkers have some limitations such as the influence of infection, durability of biomarker, and low precision in distinction of acute from chronic kidney disease (11).
Among all biomarkers, Neutrophil Gelatinase-Associated Lipocalin (NGAL) has most widely been studied. NGAL has high specificity to distinguish structural AKI from CKD, normal population and hypovolemic states, better prediction of excessive morbidity (12), the most powerful marker indicating the severity and duration of AKI (13), and an accurate marker for early detection of AKI in high risk cases such as sepsis patients (14, 15).
Calprotectin is a mediator protein of the innate immune system formed by complex of S100A8 and S100A9, two immune-regulatory calcium-binding proteins, found mainly in neutrophils and to a lesser extent in monocytes and reactive macrophages (16) and it is shown to protect against oxidative stress during inflammation (17). Additionally, renal collecting duct epithelial cells produce calprotectin and this marker is detectable in urine early after renal injury (18).
There is an increase in the amount of calprotectin in instances such as urinary tract obstruction, infection, rheumatoid arthritis, inflammatory bowel diseases, urethral carcinoma, bladder cancer, and probably in chronic kidney disorders (11, 19). There are few studies conducted in cisplatin induced ischemic kidney in rat and adult that show calprotectin could differentiate between pre-renal and ischemic acute kidney injury (20-24).
It has been shown that urinary calprotectin was superior to creatinine (Cr) for prediction of early renal ischemic injury and future renal function in patients with renal transplantation (25, 26). Moreover, animal study revealed that calprotecin has an essential role in development and severity of glomerulonephritis (27). Recently, Westhoff et al. studied the urinary biomarkers to differentiate between intrinsic and pre-renal AKI in children and found out that urinary calprotectin is a better detector (28).
Regarding the pitfalls for historic laboratory gold standard, FENa (in post ischemic ATN, ATN superimposed upon a chronic pre-renal disease, AKI due to radio contrast or pigments, acute glomerulonephritis, interstitial nephritis, and concurrent diuretic usage) and the paucity of pediatric studies, we conducted this study to evaluate the accuracy of calprotectin in differentiation between functional and structural AKI in pediatric population.
2. Methods
This is a prospective cross-sectional study conducted for a period of six months (September 2014 and March 2015) in two training hospitals (Namazi and Shahid Dastgheib) affiliated to Shiraz University of Medical Sciences. Seventy-five patients, aged from three months to 18 years, with diagnosis of acute kidney injury recruited from PICU, ward, and emergency room were enrolled in the study. Renal biopsy of all children with glomerular disease revealed accompanying tubulointerstitial inflammation. Twenty healthy children with no history of renal diseases, hypertension, or diabetes mellitus who had come to clinic for regular check-up were also included as control.
The study was approved by Ethics committee of Shiraz University of Medical Sciences (ID number 93-01-01-7154 dated 22.10.2015). Following explanation of the whole protocol in details, written consent was taken from parents before entering their children into the study.
AKI was defined by abrupt increment of serum Cr at least 0.3 mg/dL from the baseline serum Cr within 48 hours of assessment (29).
Patients were categorized into two groups of functional (pre-renal) and structural (intrinsic) AKI. Structural AKI included ischemic injury, sepsis, glomerulonephritis, and hemolytic uremic syndrom. Decline in serum Cr to the baseline after fluid repletion in less than 48 hours was attributed to functional (pre-renal) injury.
The exclusion criteria were obstructive uropathy, urinary tract infection, malnutrition, renal transplantation, chronic kidney diseases, and malignancy.
Serum Cr was measured by Jaffe method. eGFR was calculated by Schwartz formula ((Height (cm) × 0.55 )/ Plasma cr (mg/dL)) (30). Serum Cr level was measured at the time of zero of entrance and then daily, afterwards. In our laboratory it takes three hours from the blood draw to receive the results of serum Cr.
Having had the diagnosis of AKI; urine sample (10 mL) would be collected simultaneously with blood sample on the second day of admission. Then, the samples were frozen (-20°C, no centrifugation) for assessment of calprotectin level. Urinary levels of calprotectin were quantified using an enzyme-linked immunosorbent assay (ELISA) kit (PhiCal® Calprotectin, catalogue number K 6928; Immundiagnostik AG, Bensheim, Germany) according to the manufacturer’s protocol. The coefficient of variation for duplicate measurements using this ELISA kit was < 6%. To take the current concentration status of the urine into account, urinary Cr was assessed and then calprotectin/Cr ratio was calculated. Urine and serum sodium were measured by Flame photometry with Hycell PHF-104. Fractional excretion of sodium was calculated by using the formula (UNaxPcr/PNaxUcr) × 100. The level below 1% was considered as pre-renal and above that as intrinsic or renal AKI.
2.1. Statistical Analyses
Data were presented as mean ± standard deviation (SD) or median (range) with 95% confidence intervals. The comparison of variables was done by using ϰ2 or Fisher’s exact test for proportions and unpaired t-tests for means. A value of P < 0.05 was considered as statistically significant. Receiver-operating characteristic (ROC) curves were constructed to determine the accuracy of urinary calprotectin and calprotectin/Cr ratio to detect children with intrinsic AKI. Sensitivity, specificity, and positive and negative predictive values were estimated.
3. Results
From among 75 children with clinical diagnosis of AKI, 45 were classified as structural and 30 as functional AKI. In addition, 20 healthy children were enrolled in the control group. Table 1 depicts the demographics data, etiology, renal parameters and calprotectin measurements in the children with AKI and controls. Mean urinary calprotectin was 36 times higher in structural than in functional AKI, and 44 times higher than those in healthy children (P < 0.001). Additionally, there was no statistically significant difference between functional AKI and healthy subjects regarding calprotectin/Cr ratios (P = 0.21). By considering urine calprotectin to Cr ratio as the distinguishing biomarker, it was revealed that the ratio in structural AKI was about 140 times higher than that in functional AKI (P < 0.001).
| Variables | Functional (N = 30) | Structural (N = 45) | Control (N = 20) | P Value |
|---|---|---|---|---|
| Gender, No. (%) | 0.97 | |||
| Female | 15 (50) | 23 (51.1) | 10 (50) | |
| Male | 15 (50) | 22 (49.9) | 10 (50) | |
| Age, y; median, range | 7.5 (1 - 17) | 6 (1 - 17) | 10 (1 - 17) | 0.61 |
| BMI, kg/m2; median, range | 18.9 (5 - 23) | 18.7 (12 - 22.5) | 19.6 (13.3 - 28) | 0.53 |
| Origin of AKI, No. (%) | ||||
| Dehydration by gastroenteritis | 30 (100) | |||
| Hypotension-induced ATN | 15 (33.3) | |||
| Sepsis-induced ATN | 15 (33.3) | |||
| Crescentic Glomerulonephritis | 4 (8.8) | |||
| Lupus Nephritis | 2 (4.4) | |||
| Hemolytic Uremic Syndrome | 5 (11.1) | |||
| Glomerulonephritis | 4 (8.8) | |||
| Renal parameters; median, range | ||||
| eGFR, mL/min/1.73 m2 | 66 (38 - 100) | 30 (10 - 60) | 143 (110 - 190) | < 0.001 |
| Pcr, mg/dL | 1.1 (0.7 - 1.6) | 1.8 (1.3 - 5) | 0.5 (0.3 - 0.88) | < 0.001 |
| P Na, mmol/L | 141.5 (136 - 145) | 141 (136 - 145) | 141 (136 - 145) | 0.39 |
| UNa, mmol/L | 97 (6 - 165) | 80 (6 - 163) | 75 (30 - 120) | 0.98 |
| FENa, (%) | 1 (0.06 - 6.5) | 7 (0.18 - 53) | 0.7 (0.2 - 3) | < 0.001 |
| U Calprotectin, ng/mL | 28.5 (5 - 230) | 1240 (100 - 8180), Glomerular: 1040 (150 - 7940), ATN:1260 (100 - 8180) | 33 (5 - 210) | < 0.001 |
| U Calprotectin/Ucr, (ng/mL)/(mg/dL) | 94 (5 - 628) | 19352 (158 - 107000), Glomerular: 2020 (166 - 56714), ATN:6800 (158 - 107000) | 155 (16 - 8400) | < 0.001 |
Abbreviations: BMI, Body Mass Index; eGFR, Estimated Glomerular Filtration Rate; FENa, Fractional Excretion of Sodium; Pcr, Plasma Creatinin; PNa, Plasma Sodium; UNa, Urine Sodium.
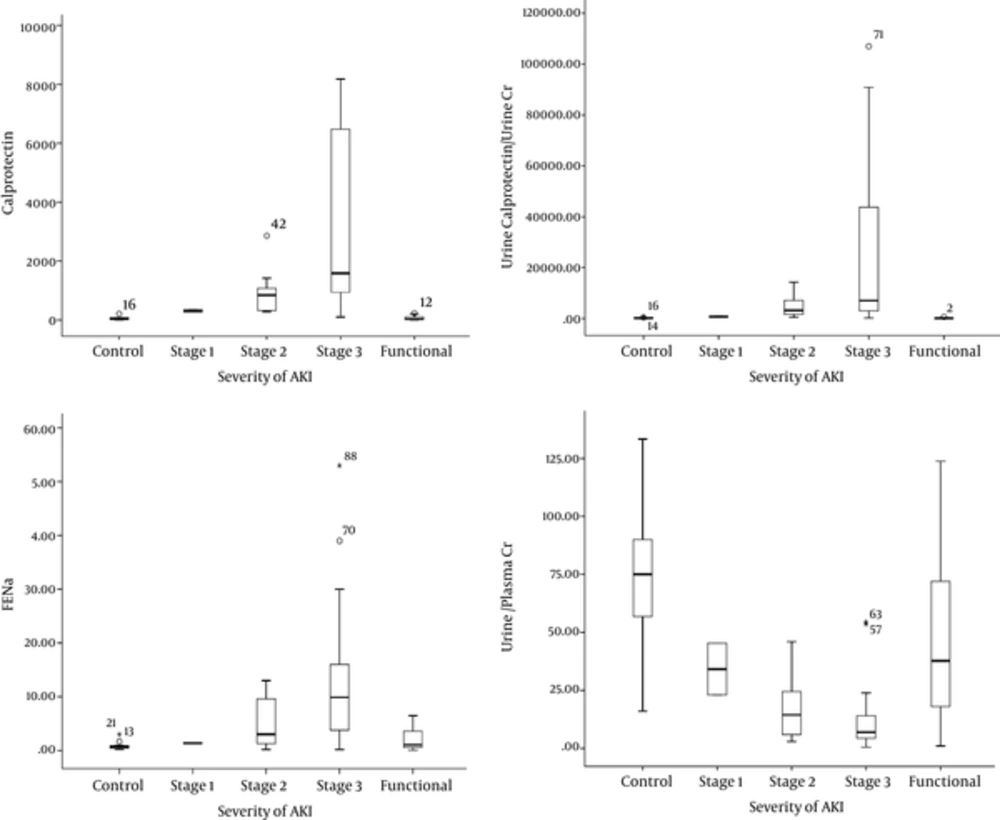
We assessed the level of calprotectin, FENa and urine/plasma Cr in different severity of AKI. As shown in Figure 1, median urinary calprotectin was rising by intensification of the severity of AKI. (P < 0.001). This was also true for FENa.
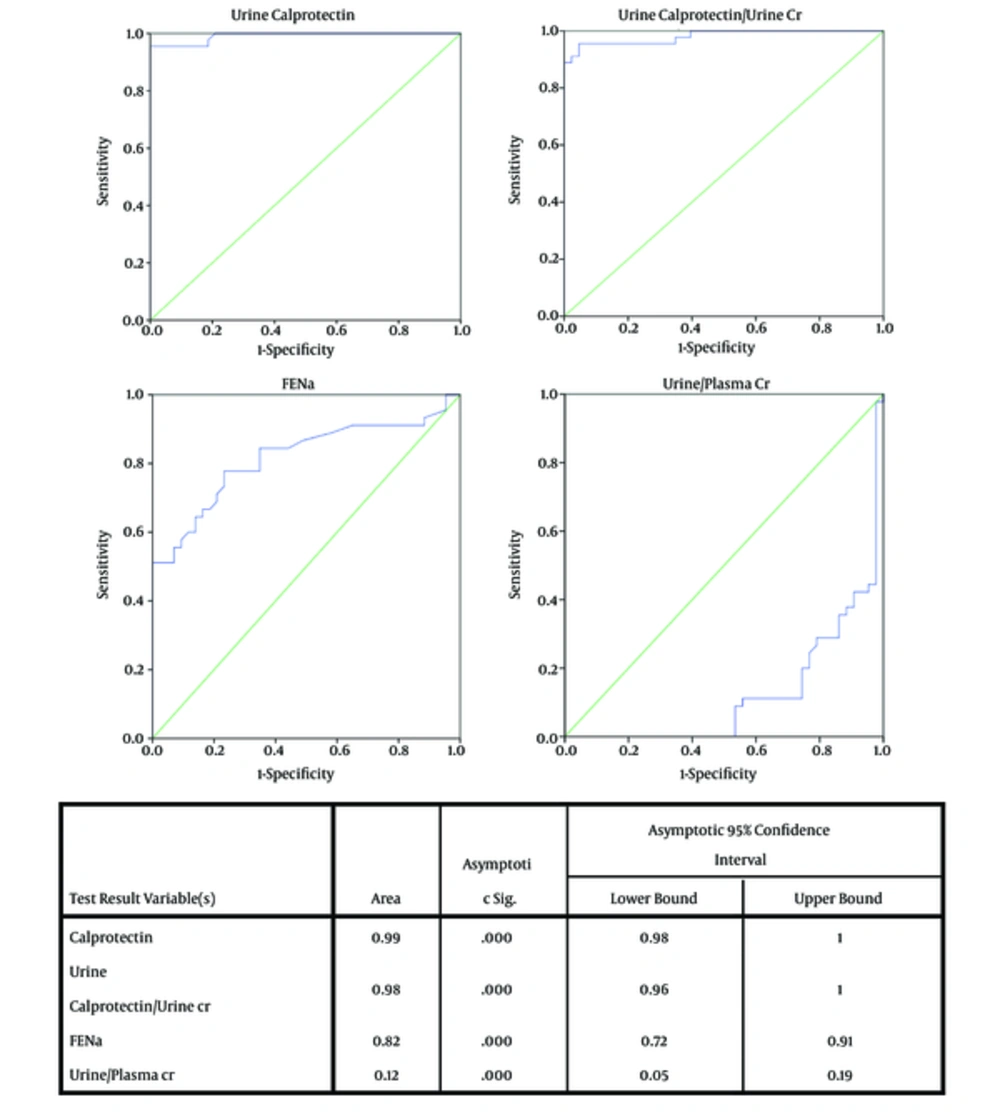
Receiver-operating characteristic (ROC) curves were constructed to determine accuracy of urinary calprotectin and calprotectin/Cr ratio to detect children with structural AKI (Figure 2) compared to FENa. The ROC curve function was better for urine calprotectin and its ratio to Cr. The optimal cut off value of urinary calprotectin for differentiation of functional and structural AKI was 230 ng/mL (sensitivity: 95.6% and specificity: 100% positive predictive value (PPV): 100%, negative predictive value (NPV): 93.8%). Besides, the cut off value of urine calprotectin/Cr ratio achieved was 383 ng/mL with sensitivity and specificity of 96.7%, PPV of 97.7%, and NPV of 96.7%. The ROC function was better than FENa and urine/plasma Cr.
Even at the same level of serum Cr and eGFR, FENa had an overlap for the functional and structural AKI. Therefore, it was not a reliable marker to be used on its own to differentiate these two classes of AKI.
4. Discussion
This study shows that urinary calprotectin has a good performance by a cut-off value of 230 ng/mL, in differentiation of structural and functional AKI in pediatric population with high sensitivity (95.6%) and specificity (100%).
The traditional definition of AKI is based on history, clinical feature, and laboratory tests. According to the results, the patients were classified into pre-renal (functional), post-renal, or structural (intrinsic) AKI. The implication of such criteria for accurate diagnosis has some limitations. These parameters might be influenced by the time of drawing blood or taking urine samples, fluid therapy, diuretic therapy and even the superimposition of AKI on an underlying renal disease. Even the validity of these parameters to put a patient in functional or structural group was not verified histologically (31).
In our study, fractional excretion criteria of 1% could classify at least 15.6 % patients in structural and half of the patients in functional group correctly. By considering urine/plasma Cr, about 27% of structural and 24% of functional AKIs were misclassified.
Basu et al. studied the combination functional (plasma Cystatin C) and tubular damage (urine NGAL) biomarkers to predict the severity and persistency of AKI defined by KDGOI in 345 children after cardiopulmonary bypass. For both entities the likelihood ratios of combination biomarkers were greater than changes of serum Cr from baseline (32).
The presence of a biomarker and its reliability and accuracy in this challenging situation is crucial. Nicolas et al. studied the value of single measurement of NGAL in comparison to alpha1-microglobulin, alpha1-acid glycoprotein, FENa, and serum Cr to recognize intrinsic AKI from pre-renal, CKD and healthy in 635 adults in emergency setting. The study revealed that NGAL was superior to other biomarkers and it was also predictive of the outcome (12).
There are few studies on the role of urinary calprotectin in discrimination between functional and structural AKI. The majority were done in adult setting or experimental study in animals. Heller F et al. showed high accuracy of urinary calprotectin for diagnosis of intrinsic AKI. They demonstrated that the cut-off level of 300 ng/mL has a sensitivity of 92.3% and specificity of 97.1% in predicting intrinsic AKI (21).
Seibert FS et al. demonstrated that high urinary calprotectin with cutoff value of 440 ng/mL is able to differentiate between pre-renal and intrinsic AKI (22). There is no study on children but one has recently been published by Westhoff et al. They compared urinary calprotectin, NGAL and KIM-1 in AKI children defined by pRIFLE and neonates defined by KDIGO. The study indicated calprotectin was superior to two other biomarkers to recognize structural AKI (28). In our study, we found that the level of random urinary calprotectin was correlated with the severity of AKI and its median was progressively higher in injury and failure class of AKI. Yet, in the same level of Cr and eGFR in functional (pre-renal) and structural (intrinsic) AKI, urine calprotectin was higher in structural group (P value < 0.05). These findings in our study might be helpful to discriminate these two entities especially when the traditional markers are not helpful to do the correct classification. Albeit, it might be helpful to estimate the severity of AKI.
Limitations of study were as follows: Exclusion of patients with malignancy as the levels of calprotectin have been studied in some malignancies such as breast cancer, urothelial and bladder carcinoma. Hence, we did not enter this group of patients due to uncertainty for the impact of underlying diseases as confounding factor for calprotectin measurement as a biomarker of AKI. Because of inadequate budget we could not measure the other new biomarkers along with urine calprotectin simultaneously. This entity may need another prospective study with combination of biomarkers; single measurement of calprotectin at the time of AKI diagnosis and lack of serial measurements, small sample sizes, lack of simultaneous measurement of NGAL, the absence of histological confirmation in the majority of study groups (except glomerulonephritis), and lack of immnuohistochemical study for calprotectin in structural AKI are other potential limitation of the present study.
4.1. Conclusion
Calprotectin could accurately diagnose structural from functional AKI. Its level increases in proportion with severity of AKI.