1. Background
An alternative therapy for children with end stage renal disease (ESRD) waiting for kidney graft is peritoneal dialysis (PD). PD catheters, being easily implanted transcutaneously, are expected to function for a reasonable lifespan. However, catheter related complications including infection, leakage, catheter dysfunction, and displacement remain to be dealt with (1).
Complications of PD come along with important and sometimes devastating morbidity, interference of medical care, decreased performance of dialysis, and eventually increase the rate of mortality. Moreover, lead to haemodialysis, increase the rate of hospitalization, and succeeding operation. These adverse effects restrict the durable survival of PD catheters in a third to half of cases after two years (2).
The optimal target for PD centers is a catheter survival rate of 80% for the first year after catheter implantation (3-5).
The international society for peritoneal dialysis (ISPD) guideline recommends the acceptable rate of peritonitis to be less than 0.67 episodes per patient-year at risk (equal to one incidence in 18 patient-months) (6).
The prevalence of chronic renal failure in Iranian children is 118.8 per million (7, 8) and since 1993 when continuous ambulatory peritoneal dialysis (CAPD) was first introduced in Iran, it has become the preferred renal replacement therapy (RRT) for neonates, infants, and young children (9). The aim of our study was to evaluate the trend of catheter survival of pediatric patients on PD and to estimate the rate of surgical complications due to catheter insertion.
2. Methods
Data of all children who underwent continuous peritoneal dialysis between 1993 and 2012 in Ali-Asghar Children’s hospital are evaluated in this retrospective study. Year 2005 is taken as cut point of comparison because prior to that time PD catheter could be inserted by all surgeons in our unit but according to latest PD consensus this policy has changed and only one expert surgeon was appointed to insert catheters. Inclusion criteria were 1) age less than 14 years, 2) severe chronic kidney disease delineated by creatinine clearance below 15 mL/min/1.73 m2 and admitted electively or emergently for uremic symptoms, fluid overload, or severe electrolyte imbalance, 3) patients under followed-up for at least six months. Patients referred from other centers for catheter insertion and those with follow-up period of less than six months or those who died in the first month of catheter insertion were excluded from outcome analysis. Patients whose renal function recovered after at least six months were included in the study.
The only catheters available for CAPD in children were soft curled swan neck Tenckhoff catheters with two Dacron cuffs for children and straight one for infants and neonates without stylet. Here is a brief description of open surgical technique: The suitable site of entrance was marked on the skin by placing the catheter on the midline surface of the abdomen. After that, one centimeter to the midline, a small incision was made. Then, partial omentectomy performed. Subsequently, the tip of catheter inserted and pushed to the pelvic space behind the bladder. After pursing around the catheter, the tunnel was created subcutaneously and the distal cuff was placed 2 cm of the exit site. Only adolescent patients were candidates for placement of catheters by laparoscopy that was recently started in our department. The patients were routinely followed every month for the first three months after surgery and then every three months by pediatric nephrologist.
Data including demographic characteristic of patients, surgical complications of CAPD and catheter outcome were collected from hospital records. For analysis, we assessed the incidence and aspect of complications including infection-related (peritonitis, tunnel infection) and catheter-related (leak, Dacron cuff extrusion, adhesion, dislocation, hernia). Peritonitis was illustrated based on the ISPD endorsement as the existence of at least two of the consecutive criteria: clinical presentation of peritoneal inflammation; a cloudy effluent with cells more than 100 cells/mm3, and positive culture of peritoneal fluid. Exit site infection was delineated as the existence of a purulent discharge from the sinus tract or pronounced swelling around catheter, reddening and/or tenderness. Leakage defined by pericatheter fluid leakage, hydrocele, genital edema, and pleural effusion). The patient information remained anonymous. According to training hospital policy, all care givers or parents signed a consent form for catheter insertion and the utilization of the data at the time of admission. It was a retrospective study; therefore no ethical approval was required.
3. Results
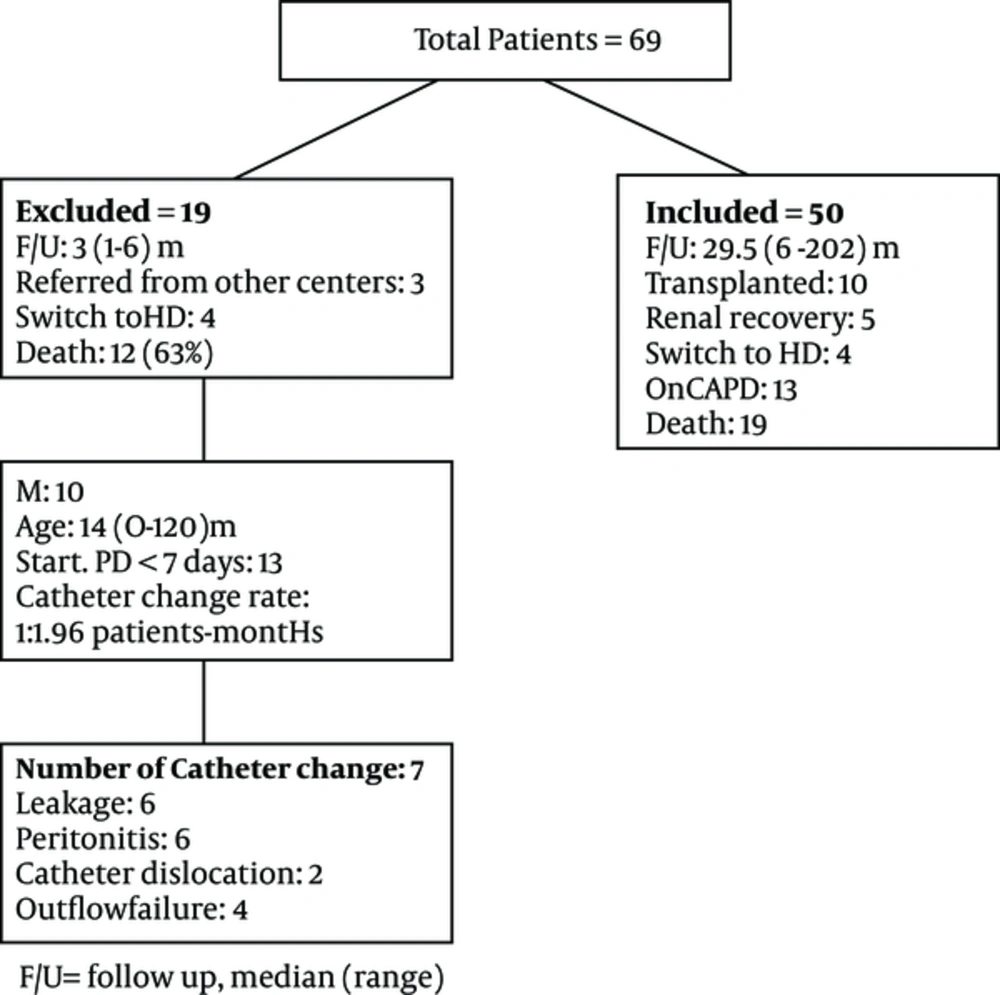
During a 19 year period 69 patients, underwent peritoneal dialysis catheter insertion. Of them 19 patients were excluded (Figure 1). At dialysis initiation the number of children was: aged 12 months or younger 18 (36%), between 12 and 24 months 12 (24%), and older than 2 years 20 (40%).
The most common underlying diseases were CAKUT and cystic kidney disease. Other underlying disorders of ESRD are summarized in Table 1.
| Variables | < 2005, N = 14 | > 2005, N = 36 | P Value |
|---|---|---|---|
| Age, median (range), mo | 11 (3 - 72) | 24 (1 - 192) | 0.083 |
| Male, No. (%) | 7 (50) | 23 (62) | 0.52 |
| Weight, Kg, mean (SD) | 8 (3.5) | 12 (8) | NS |
| Height, cm, mean (SD) | 89.5 (11.2) | 83 (20) | 0.027 |
| Underlying disease, No. (%) | 0.7 | ||
| CAKUT | 5 (36) | 11 (31) | |
| CNS | 3 (21) | 5 (14) | |
| Cystic disease | 3 (21) | 10 (28) | |
| Cystinosis | 0 | 1 (3) | |
| Hyperoxaluria | 0 | 3 (8) | |
| HUS | 3 (21) | 4 (11) | |
| Tubulopathy | 0 | 2 (5) | |
| Hypertension, No. (%) | 0.057 | ||
| SBP or DBP > 95% for age, height, sex | 8 of 12 (67) | 11 of 32 (33) | |
| eGFR, mL/min/1.73m2, mean (SD) | 9 (2.2) | 9.5 (5.6) | NS |
Abbreviations: CAKUT, Congenital Abnormality of Kidney and Urinary Tract; CNS, Congenital Nephrotic Syndrome; DBP, Diastolic Blood Pressure; HUS, Hemolytic Uremic Syndrome; SBP, Systolic Blood Pressure.
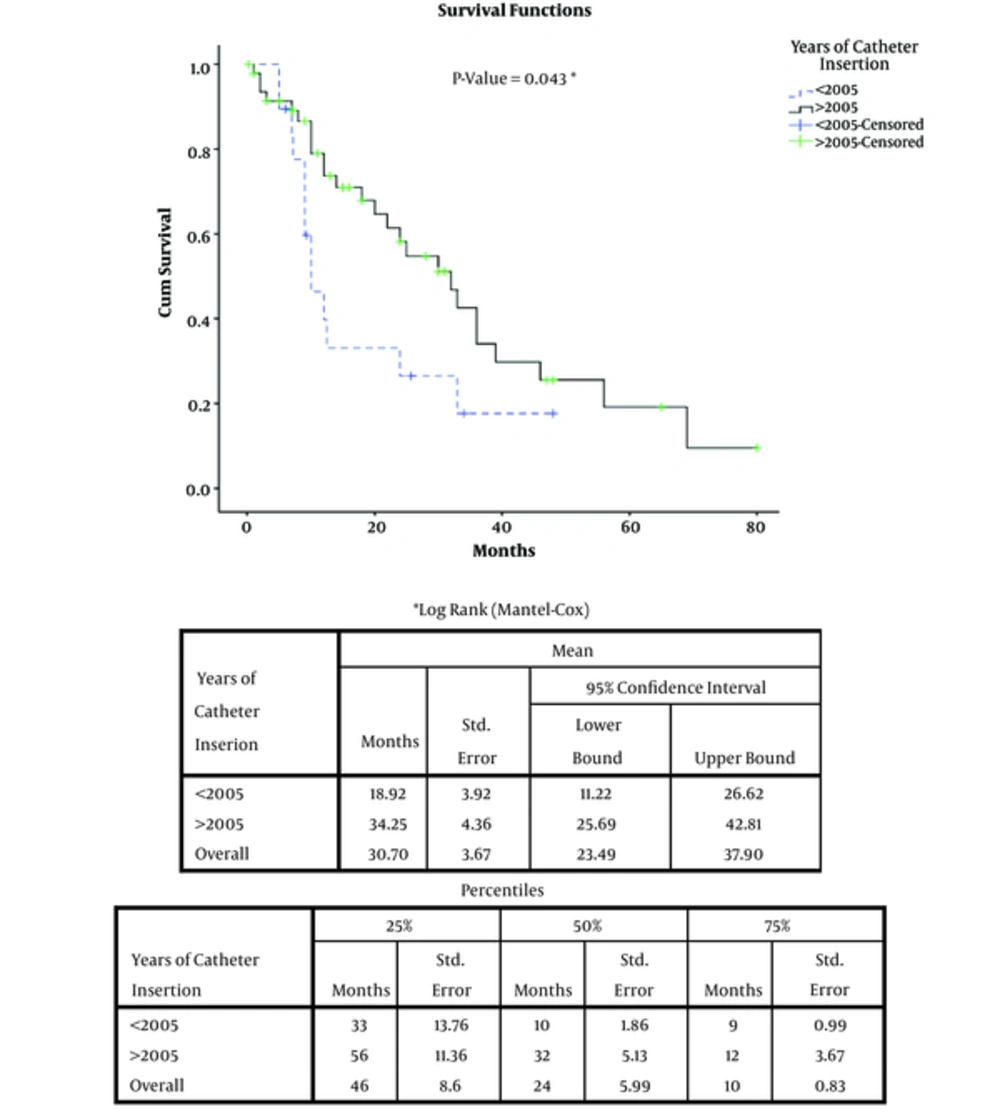
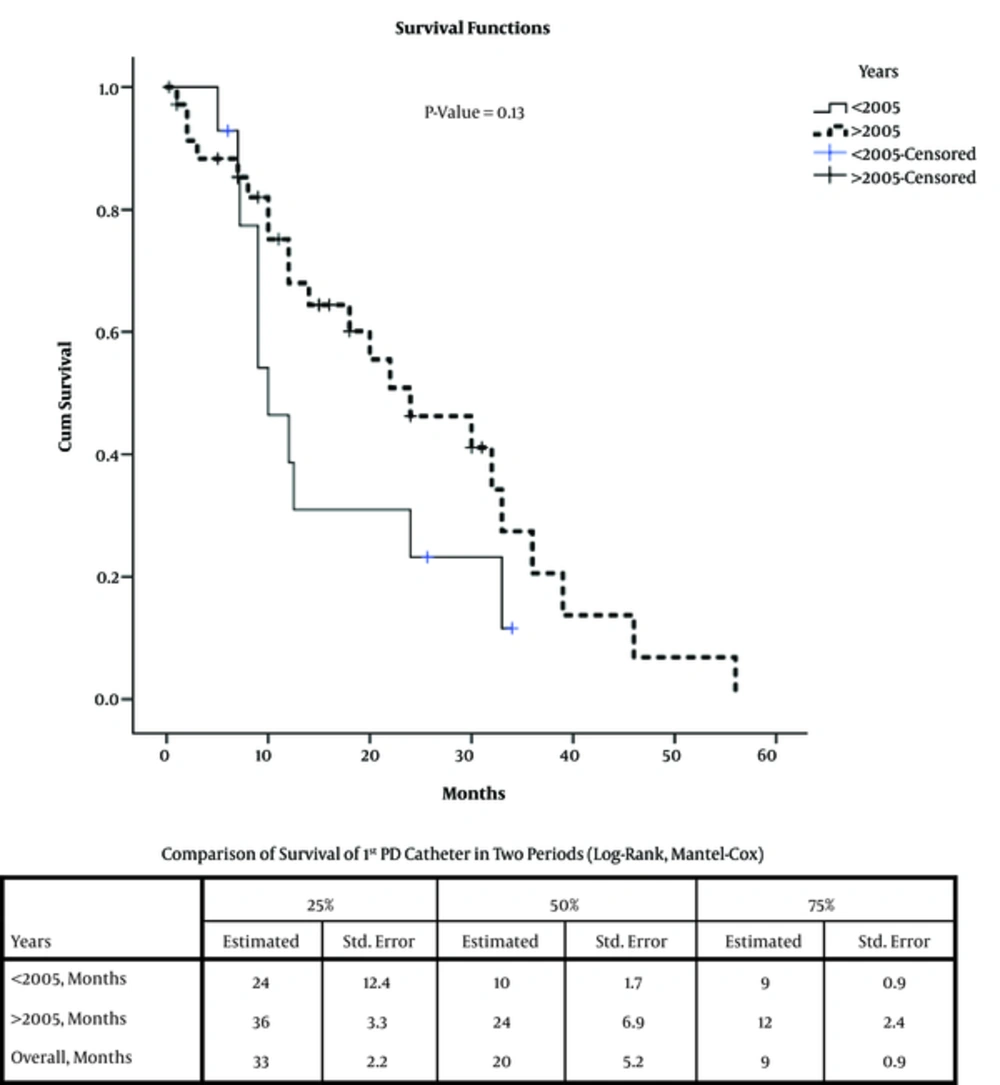
Totally 86 catheters were inserted, Table 2 shows the number of catheter changes. The changes took place because of surgical complications and the outcome of patients. Figure 2 shows the cumulative catheter-related survival of PD in two time periods. The 75% catheter survival improved from nine months in the first period to twelve months after that (P value < 0.05). The same improvement was seen in the first catheter survival; however it was not statistically significant (Figure 3). While catheter related reason was the most common cause of catheter removal or changes before 2005, afterward renal recovery was the dominant reason. Unfortunately, infection comprised still more than one fifth of catheter removals. Hernia developed in more than one third of patients. The median time for hernia occurrence was five (1 - 13) months after initiation of dialysis.
| Variables | < 2005, N = 14 | > 2005, N = 36 | P Value |
|---|---|---|---|
| Number of catheters re-inserted | NS | ||
| 0 | 7 | 21 | |
| 1 | 4 | 9 | |
| 2 | 2 | 5 | |
| 3 | 1 | 0 | |
| 6 | 0 | 1 | |
| Technique of Catheter insertion, No. (%) | |||
| Laparoscope | 0 | 4 (4.6) | |
| 1st catheter survival, months | 0.12 | ||
| 25% | 24 | 36 | |
| 50% | 10 | 24 | |
| 75% | 9 | 12 | |
| Reason of catheter change, No. (%) | 0.35 | ||
| Catheter related | 6 (43) | 7(19) | |
| Infectious related | 3 (21.4) | 9 (24) | |
| Renal function recovery/renal transplant | 3 (21.4) | 14 (38) | |
| Outcome, No. (%) | 0.52 | ||
| Transplanted | 1 (7) | 9 (24) | |
| Renal recovery | 2 (14) | 3 (8) | |
| On CAPD | 3 (21) | 10 (27) | |
| Switch to HD | 2 (14) | 2 (5) | |
| Death | 6 (43) | 13 (35) | |
| Surgical complications | NS | ||
| Hernia, No. (%) | 6 (42.8) | 13 (36) | |
| Incisional | 1 | 4 | |
| Inguinal | 3 | 9 | |
| Umblical | 2 | 0 | |
| Outflow failure, No. (%) | 10 (77) | 12 (25) | 0.001, RR: 1.69 (1.14 - 2.5) |
| Leak, No. (%) | 8 (57) | 15 (40.5) | 0.28 |
| Pleural effusion | 1 | 1 | |
| hydrocele | 0 | 4 | |
| Time to leak (months, median (range) | 5.5 (1 - 10) | 6 (1 - 27) | NS |
| Persistent peritonitis | 3 (21) | 17 (47) | 0.11 |
| Start PD immediately (< 7days), No. (%) | 9 (64) | 10 (27) | 0.23, RR: 2.37 (1.23 - 4.59) |
Catheter reinsertion rate improved from 1 per 30.76 (before 2005) to 1 per 63.72 patient-months (after 2005). The median (range) follow up of patients was 29.5 (6 - 126) months.
Seven cases of outflow failure were due to fibrin clot in 2, rotation of catheter in 2, and adhesions in 3 cases. Figure 2 shows the 25%, 50% and 75% survival of the first PD catheter survival in two time period. There was improvement of survival after in the years after 2005 but the difference was not significant.
The rate of peritonitis was one per 7.5 patients-month (before 2005) and declined to one per 56.89 patients-month. Causative organisms for peritonitis in our patients are summarized in Table 3.
| Etiology | < 2005, N = 14 (36 Episodes) | > 2005, N = 36 (40 Episodes) | P Value |
|---|---|---|---|
| Gram Positive, No. (%) | 17 (47.2) | 11 (27.5) | 0.07 |
| SAU | 4 | 6 | |
| Enterobacter | 0 | 2 | |
| MRSA | 10 | 0 | |
| CONS | 3 | 3 | |
| Gram Negative, No. (%) | 3 (8.3) | 15 (37.5) | 0.003, 95%CI (8.7 - 47.1) |
| E. coli | 1 | 4 | |
| Pseudomonas | 1 | 6 | |
| Klebsiella | 0 | 3 | |
| Acinetobacter | 1 | 2 | |
| Fungal, No. (%) | 1 (2.7) | 4 (10) | 0.2 |
| Candida albicans | 1 | 1 | |
| Mucomycosis | 0 | 1 | |
| Culture Negative, No. (%) | 15 (41.6) | 10 (25) | 0.12 |
| Peritonitis rate | 1 per 7.5 patients-month | 1 per 56.89 patients-month |
Abbreviations: CONS, Coagulase Negative Streptococcus; MRSA, Methicillin Resistant Staphylococcus Aureus; SAU, Staphylococcus Aureus.
4. Discussion
This study revealed that first catheter survival improved dramatically compared to the previous study in Iran (9) but it is still much lower than that in other developing countries (10, 11).
In our study the first year catheter survival was about 75% and it was comparable to the registry of Italy. The catheter reinsertion rate decreased from 1 per 31 to one per 64 patient- month. A large multicenter registry in Italy reported the outcome of 503 surgically inserted catheter in children. The first year catheter survival was 78% and the rate of catheter reinsertion was one per 17.9 patient-months. In their registry leakage and dislocation were followed by infection as the most frequent complication after surgery (12).
Al Salum et al reported 63 catheter insertions in 48 children with a catheter insertion rate of one per 9.65 patient-months (13). Peritonitis was the main complication among PD patients in Saudi Arabia. Median catheter survival of 27 Indian children on CAPD was 9.11 months, of whom, ten children younger than five years old had catheter obstruction due to omentum block (14). In TUPEPD registry the majority of catheters implanted with open surgical technique and the overall first catheter survival was 95%. The outcome was much better than in our center (15, 16). A six-year report of dialysis in children from Saudi Arabia, states that 19 out of 48 patients on CAPD had PD failure and the cause was obstruction in half of the cases (17).
In the first period of study about two thirds of catheters had outflow failure. The outflow failure rate declined to 20% in the second period of study. However, we routinely do partial omentectomy, the main cause of outflow failure was adhesion and then catheter dislocation in both periods. The five year technique survival was 50% in our study that was lower than the national reports. Although the catheter survival improved in the second period of study but the rate was still below the standard level (18). A multicenter report of presternal catheter for PD in Poland had a median catheter survival of 72 months (19). Complications related to technique were relatively low in our study compared to other studies which could be attributed to our increased experience, since more and more cases of pediatric ESRD patients receive PD in our country.
One of the best advantages was significant reduction in peritonitis rate when we compared the in two periods of study. It had declined from one per 7.5 patient-months to one per 56.9 patients- month. This improvement is related to good nursing care, improvement in connection system, re-evaluation of techniques every six months by the dialysis nurse, screening for staphylococcus carrier and appropriate treatment before catheter insertion, we did not have any case of MRSA peritonitis after 2005 but unfortunately the rate of gram negative peritonitis doubled in the second period of study. Regarding to peritonitis rate of TUPEPD that was one per 15.5 patient-months to one per 63 patient-months, our result was comparable. (16).
One of the major post catheter complications was the occurrence of hernia and leakage. That the frequency of them had not changed much. We did not find any relation between leakage and malnutrition ((P value: 0.2; OR: 1.68(95% CI: 0.58 - 4.8)) or the early onset of dialysis ((P value = 0.054, OR: 2.84 (95% CI: 0.96 - 8.37)).
The main limitation of this study was its being a retrospective study and the high rate of drop outs or missing cases because some patients had been referred from other centers for catheter insertion. This study showed that despite the fact that our technique and experience is improving the management of catheter and infections related to it are still weak and need to be addressed in order to reach the standard CPD care.
4.1. Conclusion
This study showed that although improvement in our technique has been accomplished and complications related to technique of insertion are declining; management and care of the catheter in order to reduce peritonitis is still insufficient and more should be done to educate nurses and parents and care givers in this regard.