1. Background
Congenital heart disease (CHD) is a multifactorial and polygenic disease, accounting for up to 30% of major congenital anomalies. It is considered the most common cause of childhood death due to congenital defects (1). It has been reported that the prevalence of births with CHD is about 4 to 50 per 1,000, with the highest prevalence as 9.3 per 1,000 live births in Asia (2). Almost 30% of these cases need corrective/palliative cardiac surgery (3). The mortality rate has recently declined dramatically due to improved surgical techniques and postoperative care (4). However, the literature shows that neurodevelopmental problems are common in infants with CHD undergoing cardiac surgery and up to 50% of surviving children will have a variety of impaired neurodevelopmental abnormalities (5-8).
Neurological injuries are likely to occur preoperatively, intraoperatively, or postoperatively. With preoperative neuroimaging and neurological examination, brain abnormalities are detected in a significant percentage of infants with CHD. These brain abnormalities are the results of intrauterine hemodynamic alterations, concomitant congenital brain abnormalities, and acquired brain injuries related to prolonged cyanosis or hypo-perfusion state after birth (9). However, most injuries occur postoperatively, leading to impaired white matter maturation and mental or psychomotor developmental delay (3, 5). Early manifestations of these injuries in neuroimaging include intraparenchymal hemorrhage (IPH), infarction, and Periventricular Leukomalacia (PVL) (6). They all can occur due to hemodynamic instabilities, embolisms, or severe hypoxemia (10). Besides, it has been corroborated that the risk of postoperative seizure, the presence of ischemic lesions on magnetic resonance imaging (MRI), and abnormal neurologic examinations can increase during the first year after surgery (4, 6, 11, 12).
All these findings emphasize the importance of potential neurologic disabilities in high-risk infants with CHD. Therefore, identifying high-risk children for neurodevelopmental sequelae could be helpful.
2. Objectives
In this study, we focused on postoperative neurologic complications detected in brain computed tomography (CT) scan after corrective/palliative cardiac surgery in infants with CHD.
3. Methods
3.1. Study Design
This retrospective cross-sectional hospital-based study examined children with a history of CHD, undergoing corrective/palliative cardiac surgery from May 2015 to May 2016. We assessed abnormal neurologic recovery in the early postoperative period by brain CT scans.
3.2. Data Collection and Analysis
We examined the medical history of patients with CHD undergoing corrective/palliative cardiac surgery to select children assessed by brain CT scans due to abnormal neurologic recovery. It was the policy of our cardiac intensive care unit to obtain neurologic consultation for every child with suspected neurologic manifestations in the early postoperative period. Patients with brain CT scans after discharge were excluded from the study.
The documents were studied to extract brain CT scan findings and control CT scans (if any). All findings were evaluated by a consultant radiologist. We used the patients’ medical documents to record the demographic variables, including gender, age (< 1 month, 1 - 12 months, or > 12 months), past medical history (type of heart disease, concomitant anomaly, diagnosed genetic disorders, previous hospitalization), surgery details (duration of cardiac bypass), type of neurologic manifestation leading to brain CT scan, and postoperative coagulopathy requiring treatment.
Statistical analysis was performed using SPSS 16.0 software (SPSS Inc., Chicago, IL, USA). Statistical significance was considered as a p-value of less than 0.05.
3.3. Ethical Concerns
This study was approved by the Tehran University of Medical Science Ethics Committee and all data were kept confidential. There was no further intervention. The brain CT scan as a diagnostic procedure was ordered by neurologists.
4. Results
From 734 cases undergoing corrective/palliative cardiac surgery during a year, 40 symptomatic patients were assessed with a brain CT scan (5.44%) and requited for our study (Table 1). Among them, 12 (of 162) cases were in the age subgroup of < 1 month, 14 (of 268) cases in the age subgroup of 1 - 12 months, and 14 (of 304) cases in the age subgroup of > 12 months. The mean age of the patients was 14.6 months, ranging from 1 month to 6 years. Patients younger than one month had the most probability of presenting with abnormal neurologic symptoms and being assessed by brain CT scans (7.4%). In terms of gender, 22 patients were male (55%) and 18 were female (45%). According to our evaluations, 23 (57.5%) cases had abnormal findings in their brain CT scans. Of them, 12 cases were female with a mean age of 13.2 months and 11 were male with a mean age of 5.5 months. Four patients had associated CNS anomalies, including dandy walker, corpus callosum agenesis, calcification in bilateral centrum semiovale white matter, lissencephaly, and pachygyria. All of them had preoperative neurological imaging and underwent postoperative imaging because of their abnormal neurologic recovery and acute neurologic symptoms; moreover, their acute brain CT scan changes were analyzed. There were two cases with cerebral atrophy, both of which had cyanotic heart disease. These three patients died before discharge, all of whom presented with a neurologic manifestation of seizure. One of the three patients had cerebral atrophy in the brain CT scan and no other acute pathology was found in their imaging. The mortality rate of patients undergoing cardiac surgery was 6.4%. However, the mortality rate of patients with abnormal neurologic symptoms was slightly higher (7.5%).
| Age Subgroup, mo | Mortality | Total | |||
|---|---|---|---|---|---|
| < 1 | 1 - 12 | > 12 | |||
| Patients undergoing cardiac surgery | 162 | 268 | 304 | 47 | 734 |
| Patients with abnormal neurologic recovery | 12 | 14 | 14 | 3 | 40 |
Age Distribution and Mortality Rates
Cardiac anomalies undergoing corrective/palliative surgery could be categorized as tetralogy of fallot (TOF), transposition of great arteries (TGA), arc obstruction (coarctation or interruption), atrial septal defect (ASD), ventricular septal defect (VSD), patent ductus arteriosus (PDA), anomalous pulmonary venous return, miscellaneous anomalies, and complex anomalies. The most frequent heart anomaly was TGA with 11 cases (27.5%), which is considered the most common cause of cardiac surgery in the first month of life. The second most common anomaly was TOF (17.5%) and the other common anomalies were ASD, VSD, PDA, and arc obstruction, with equal rates (15%).
Acute neurologic manifestations leading to brain CT scans included seizure, headache, clonus, abnormal deep tendon reflex, paresis/hypotonia, and loss of consciousness. The most common neurologic manifestations were seizure (67.5%) and paresis/hypotonia (17.5%). The seizure was the most common symptom in the age group of 1 - 12 months, occurring in 85.71% of the cases. Data are shown in Table 2.
| SAH | SDH | IPH | IVH | Ischemic Infarction | Diffuse Brain Edema | Normal | |
|---|---|---|---|---|---|---|---|
| TGA | 8 | 2 | 4 | 2 | 0 | 0 | 3 |
| TOF | 2 | 0 | 0 | 1 | 1 | 0 | 4 |
| Arc obstruction | 4 | 0 | 0 | 1 | 1 | 1 | 1 |
| ASD/VSD/PDA | 2 | 0 | 0 | 0 | 0 | 0 | 4 |
| TAPVC/PAPVC | 1 | 0 | 0 | 0 | 1 | 1 | 0 |
| Miscellaneous | 2 | 0 | 1 | 0 | 0 | 1 | 3 |
| Complex | 0 | 0 | 1 | 0 | 1 | 0 | 1 |
Type and Frequency of Pathologies in Brain Computed Tomography of Patients with Abnormal Neurological Symptoms in the Postoperative Period After Cardiac Surgery for Congenital Heart Disease
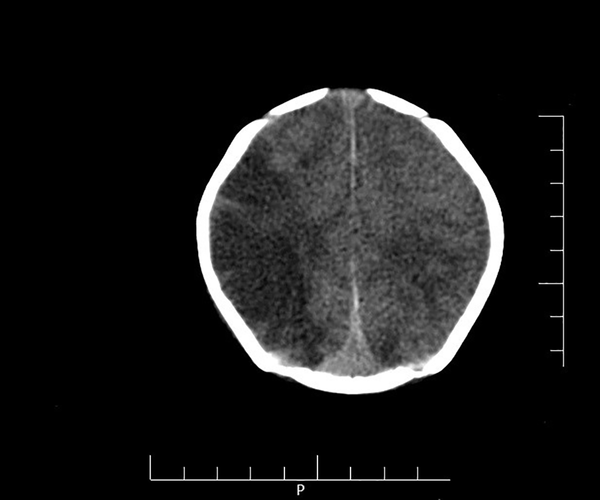
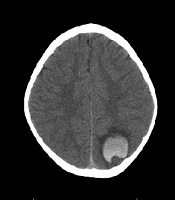
Abnormal brain CT scan findings included intracranial hemorrhage (such as subarachnoid hemorrhage (SAH), subdural hematoma (SDH), intra-ventricular hemorrhage (IVH) and IPH, ischemic infarction, and diffuse brain edema (Figures 1 and 2). The most frequent pathology in brain CT scans of patients presenting with seizure was SAH with a P value of 0.007. Besides, the seizure was the most accurate predictive of having abnormal findings among other neurologic complications leading to brain CT scans (77.77% abnormal neuroimaging findings among them). The most common findings in brain CT scans included SAH (82.6%), IPH (26.08%), and ischemic infarction (17.39%). The prevalence of intracranial hemorrhage was not statistically different between age groups.
There was no correlation between the type of heart anomaly and brain CT scan abnormalities while patients with a history of arc obstruction or TGA were more likely to have abnormal brain CT scan findings (5 of 6 arc obstruction cases (83.33%) and 8 of 11 TGA cases (72.72%)). Data also suggested that bypass times of over 180 min could significantly increase the risk of having abnormal findings in brain CT scans (P value = 0.03), particularly IPH (P value = 0.016).
Treatment was required in 57.5% of the patients for their postoperative coagulopathy. The rate of coagulopathy was significantly higher in the age group of 1 - 12 months (P value = 0.021). Although coagulopathy in the postoperative period did not have a significant correlation with abnormal findings in brain CT scans, the presence of coagulopathy concomitant with seizure would significantly increase the possibility of intracranial hemorrhage (P value = 0.049).
5. Discussion
The literature has proven infants’ neurodevelopmental sequela either before or after cardiac surgery for CHD (3, 5, 6, 8, 10-21). As the CHD prognosis improves by successful surgery and postoperative management, the importance of neurologic impairment is not negligible. These neurologic damages were documented using neuroimaging techniques either before or after cardiac surgery. Previous studies have used MRI (1) or CT scans to find brain injuries (2, 3). This study demonstrated that the incidence of neurologic symptoms in the early postoperative period after cardiac surgery was 5.5 per 100 cases and the incidence of acute neurologic manifestation depicted in brain CT scan was 3 per 100 cases.
Severe paresis/hypotonia, seizure, reduced alertness, stroke, chorea, and microcephaly have been reported as common neurological complications (4). As reported in the literature, the seizure is the most common postoperative complication (5-7). Our study also showed seizures and paresis/hypotonia as the most common neurologic symptoms. In addition, seizure was a considerable predictive factor for having abnormal findings on brain CT scans. Beyond the effect of the background brain pathology, seizure itself affects the neurodevelopment in infants, which can alter the brain maturation with more severe insults in the underdeveloped brain presenting with abnormal points in follow-up MRIs (4, 11, 14, 22). Furthermore, perioperative seizure has been found to be a risk factor for a worse neurodevelopmental outcome (5-7). Considering seizure as the most prevalent neurologic manifestation, especially in lower age groups, it raises the concern about later neurologic outcomes. With improvement in surgical techniques and postoperative management, the incidence of cryptogenic seizure (without defined pathology) is decreasing. In this study, 22.22% of the patients presenting with seizure did not show obvious pathology in their initial brain CT scans. However, brain MRI would better characterize some pathologies, which were not evident in brain CT scans. The risk of an acute neurologic symptom, particularly seizure, has shown to be associated with the type of heart anomalies (22). It has been also reported that the frequency of motor disabilities increases in the presence of cyanotic heart defects (21). We found no significant association in this field but based on our findings, cyanotic heart disease deserved specific attention both due to its greater prevalence in comparison with non-cyanotic heart disease and because of higher frequency of neurologic complications and abnormal neuroimaging postoperatively.
Based on our data, intracranial hemorrhage and ischemic infarction were the most common abnormal findings in brain CT scans with an incidence of about 2.8 and 0.5 per 100 cases of cardiac surgery, respectively. These two findings were also the most frequent underlying pathologies in patients presenting with seizures. Other studies found the incidence of early post-cardiac surgery infarction to be about 1 per 185 cases, which is similar to our results (19).
Based on neuroimaging studies, cerebral ischemic insults as mild (PVL) or focal (arterial infarct) lesions showed an increased incidence following cardiac surgery. Arterial infarctions are less common after cardiac surgery in children than in adults. The infarctions are usually thromboembolic in origin with air, fat, platelet, or iatrogenic emboli from cardiopulmonary bypass as common sources (8). Periventricular leukomalacia has been reported to exist in the MRIs of more than 50% of neonates after cardiac surgery (6). Variables associated with stroke in these patients include older age, longer bypass time, duration of postoperative hospital stay, and the number of operations (9). Other brain lesions presenting in MRIs include parenchymal hemorrhage, infraction, diffuse brain abnormalities, hypoxic-ischemic encephalopathy, and focal cortical injuries, which have shown in some studies to be associated with prolonged deep hypothermia in infants, especially those under one month of age (16, 20).
Chock et al. reported no correlation between intraoperative events and neurological complications after surgery (10). However, some studies found different consequences and showed that bypass times of longer than 60 min were associated with a higher risk of neurologic injuries (9, 11, 12), which was true about the duration of surgery and higher patient’s age, resulting in an increased risk of infarction (9). Our study revealed that prolonged bypass time (> 180 min) was considerably associated with the presence of abnormal features in brain CT scans, particularly SAH. We found no significant correlation between other intraoperative variables and brain CT scan findings.
The presence of coagulopathies in the early postoperative period has not shown significant associations with abnormal neuroimaging findings. However, coagulopathy in association with seizure can increase the possibility of intracranial hemorrhage. This could be an area of concern about the role of coagulopathies in neurologic complications. Regarding the high prevalence of coagulopathy (50%), this issue needs specific attention, especially in lower age groups due to the greater prevalence of coagulopathy and brain vulnerability to injuries.
According to the inherent difficulty in the evaluation of neurologic status in critically ill patients, given heavy sedation and failure of the immature brain to localize damages, we should take care of the underestimation of neurologic complications. Finally, some children may die in the hospitalization period due to brain insults before neuroimaging and establishing the etiology. Missing these cases could be a major limitation of our study.
5.1. Conclusions
Our study revealed seizure as the most common neurologic manifestation in the early postoperative period of corrective/palliative cardiac surgery for CHD and the intracranial hemorrhage as the most common underlying pathology in patients with abnormal neurologic recovery. Moreover, SAH and IPH were the most frequent types of intracranial hemorrhage, in sequence. Although seizure is common in patients with CHD in the perioperative period, co-presentation of seizure and coagulopathy should be a great concern for physicians to evaluate acute neurologic events more carefully.
.jpg)