1. Background
Primary teeth pulpotomy is ideally followed by stainless steel crown (SSC) placement (1, 2). SSCs are strongly superior to amalgam in respect to their durability, longevity and cost efficiency (2-4). But due to prefabricated entity and lack of marginal accuracy, they can’t provide adequate seal against over-time contamination (2). Moreover, in deep mesio-distal cavities, one deficiency of SSC is the short height which can’t completely cover the proximal area. Another situation that may occur during oral performance is occlusal perforation of SSCs placed in heavy stress bearing area which often makes treatment failed.
So much the better, if the hard-setting cement placed over the capping and beneath SSC has the inherent quality that reduces microleakage over the time. Nowadays, there are some materials such as MTA which can provide excellent seal (5-7). However, due to extra expense, it isn’t a routine pulp dressing material in primary teeth. In this regard, pulpotomy-glass ionomer-SSC can be suggested as a valid and practical alternative to pulpotomy-SSC procedure.
In children, use of glass ionomers (GI) are of clinical importance because of in-office time shortening and fluoride release (8, 9). GI were introduced to dentistry at the end of 20th century (10). GI bind chemically to tooth substance, release fluoride, and have antibacterial activity (9, 11). On the other hand, the material has some drawbacks such as poor mechanical and unaesthetic properties (12). Over the course of time, the GI developed until the type of resin modified GI (RMGI) were introduced. RMGI have properties that overcome the drawbacks of self-cured GI (12). In pediatric dentistry, the rational of placing GI beneath the SSC, as a non-expensive material, is an attempt to maintain the pulp therapy successful by maximizing seal against microorganisms and prevent further interventions such as retreatment or extraction long before the natural time of exfoliation.
Researchers reported a high success rate of pulpotomized teeth restored with SSC (13). In a retrospective study, pulpotomy of the primary molars restored with resin-based materials showed lower success rate than SSC (14). In addition, in the assessment of the success rate of pulpotomy with formocresol in the primary molars restored with SSC and amalgam, it was showed that amalgam can be a suitable choice if the remaining life span of the tooth is less than 2 years (15).
2. Objectives
In pulpotom it is relevant to propose GI build up beneath SSC, whilst seen as being slightly more time-consuming, as an alternative to the conventional technique of pulpotomy-SSC. Considering the fact that SSC is the restoration of choice and, until recently, there is no published research; the present study was designated to evaluate the clinical and radiographic success rate of either pulpotomy-SSC or pulpotomy-GI Build up-SSC.
3. Methods
The study was approved by the Review Board of Zahedan University of Medical Sciences (IR.ZAUMS.REC.1395.41) and registered in the Iranian Registry of Clinical Trials (IRCT201609226105N6).
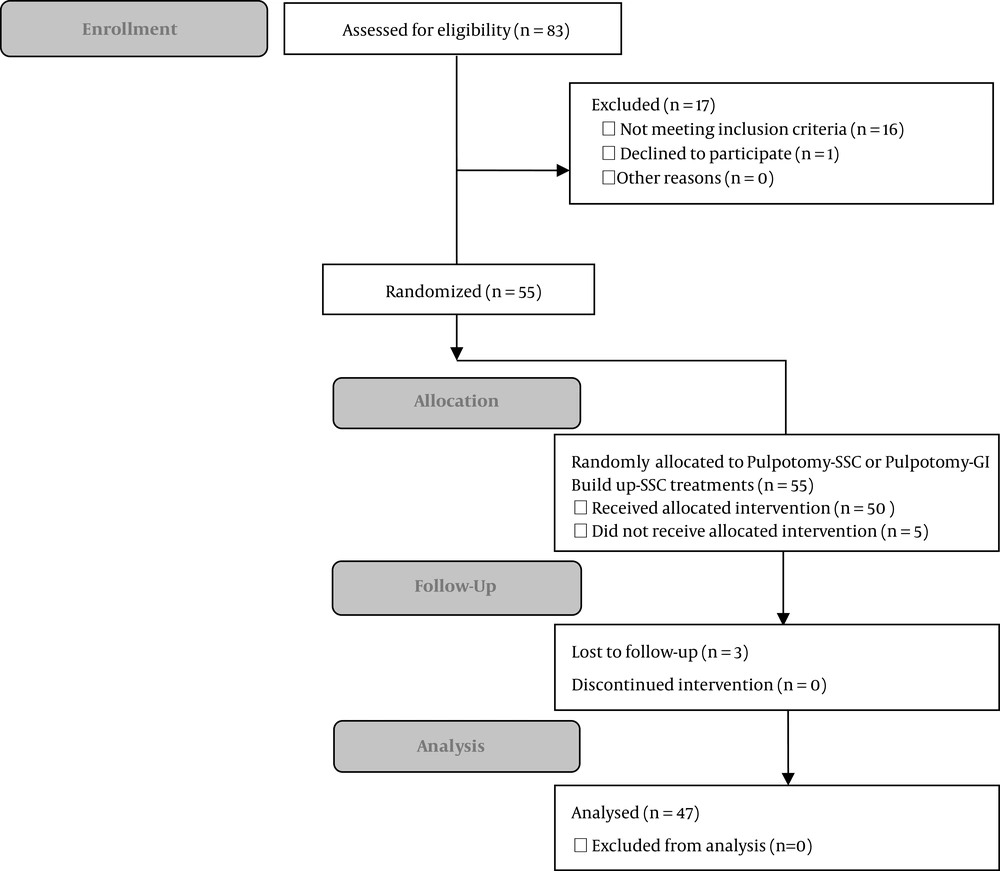
For this randomized clinical trial, split-mouth design study, 4- to 8-year-old children, referred to the Pediatric Department of Zahedan Dental School between December 2016 and March 2017, with following criteria were enrolled. The inclusion criteria were: both primary mandibular second molars requiring pulpotomy demonstrating caries varying from one surface to restorable extensively carious lesions, matched in both teeth of each child (having the same surfaces of caries involvement and same remaining tooth structure after caries excavation in both teeth), complete physical health and cooperation during the treatment. Eligibility for pulpotomy were confirmed based on clinical and radiographic examinations (PA radiography). Based on one study (16), considering a power of 90% and type I error of 0.05, a total of 55 children were selected as the sample population. Among 83 attended children, 66 met the criteria. A final sample size of 55 was calculated using a table of random numbers (Figure 1).
After providing explanations, informed consent forms were signed by the parents. To treat both teeth of each child, the teeth were randomly assigned into two methods using the coin flip. The procedures were performed in the Pediatric Department of Zahedan Dental School.
Pulpotomy-SSC (P/SSC) (Control): After injection, rubber dam isolation and caries removal, access cavity was prepared. The coronal pulp was excised and residual pulp tissue was rinsed with normal saline. After establishing hemostasis, fixation of the residual pulp was performed using a 1:5 diluted Buckley’s FormoCresol® solution (Buckley’s FormoCresol® Sultan Healthcare, Hackensack, NJ, USA) for 1 minute. A hard-setting zinc oxide-eugenol (ZOE) (IRM, Dentsply Caulk, Milford, Del, USA) was then used as dressing and entire-cavity filling material (Figure 2). The crown was restored with SSC (3M ESPE, St. Paul, MN, USA) using GI luting cement (GC, Tokyo, Japan).
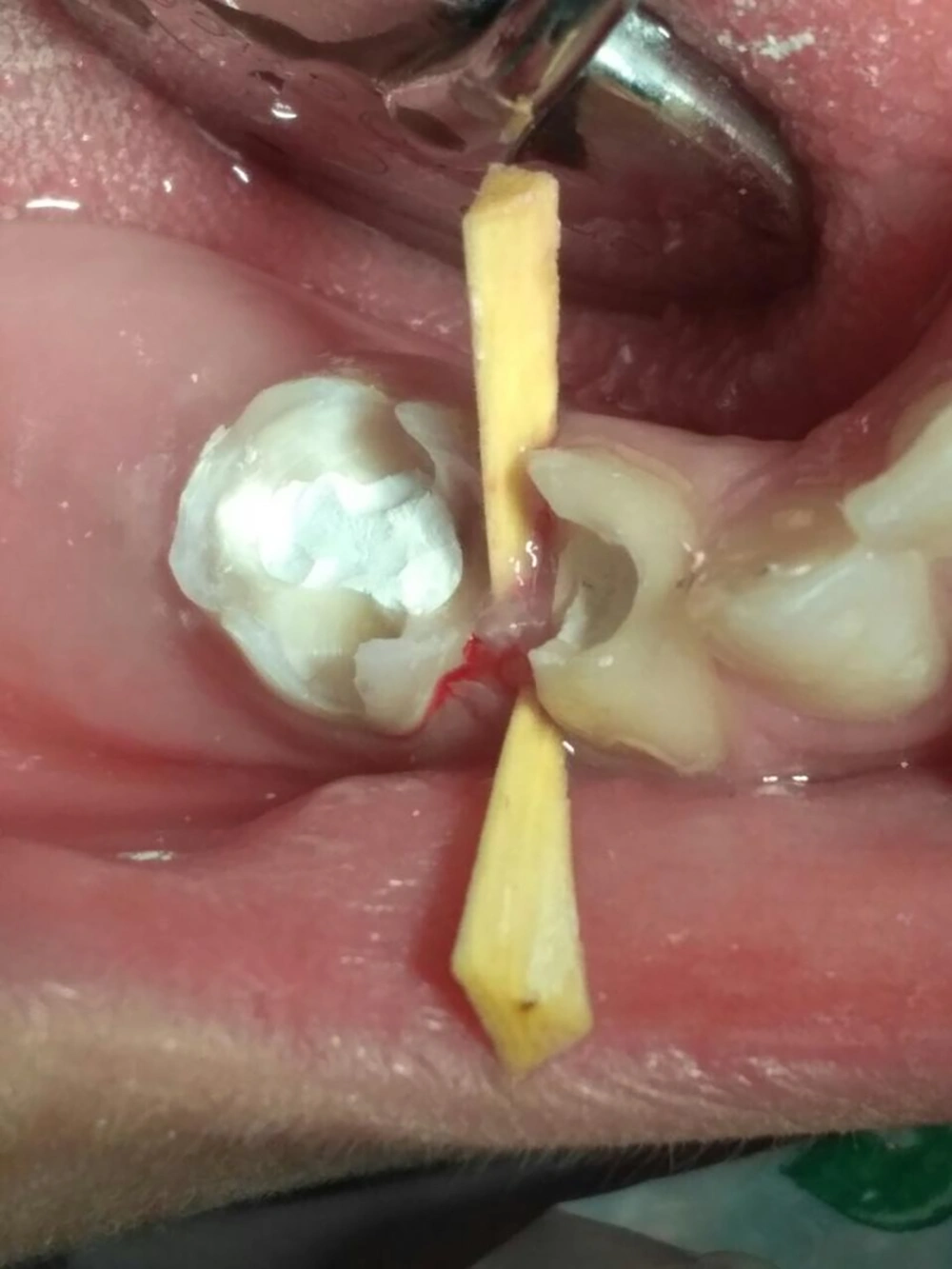
Pulpotomy-GI build up-SSC (P/GI/SSC) (Case): The pulpotomy procedure was similar to that of the control. After dressing the radicular pulp with the hard-setting ZOE, the light-cured reinforced restorative GI (GC Fuji II LC CAPSULE, Tokyo, Japan) was applied by layering technique to rebuild the crown. GI was cured using a Coltolux light curing unit (Coltene AG, Altstatten, Switzerland) for 40 seconds each layer (Figures 3 and 4). SCC (3M ESPE, St. Paul, Minn, USA) was placed using GI luting cement (GC, Tokyo, Japan).
In cases of poor cooperation, need for adjunctive pulpal analgesia, or when hemostasis was impossible, the subject was excluded from the study.
One dental student recruited children, assigned their teeth into methods, scheduled the operation time, and supervised them throughout the trial. The evaluation of the subject's eligibility, deposition of anesthesia, completion of pulpotomy, and restoration were conducted by one experienced pedodontist. Each tooth was completely treated in a single session. The time interval between both sides were 1 week. The clinical and radiographic examinations were conducted at 6 months postoperatively. The success was evaluated by the same treatment provider who acted as the blind outcome assessor. The participants were also blinded.
Redness or swelling of vestibular area, tenderness upon percussion, tenderness upon touching of the vestibulum, tooth mobility, fistula, abscess, periodontal ligament (PDL) widening, loss of lamina dura, internal or external root resorption, and radiolucency of furcation or periapical area were failure criteria. Evidence of at least one finding was considered as failure. Clinical examinations were performed under the light of dental unit, using a mirror. Radiographs were prepared using the parallel technique so that intraradicular and periapical areas could be seen. The intra-rater reliability was confirmed through reevaluation of the 10% of the radiographs. Data were analyzed using the SPSS (17) (SPSS, Inc, Chicago, IL, USA) and the Fisher's exact test. P value of 0.05 was considered as significant.
4. Results
Among the subjects, 2 who received one allocated treatment because of poor cooperation, 2 who demonstrated pain during the procedure (indicative of pulpal inflammation and hyperemia), and one who did not show clot formation were excluded. All subjects in whom both teeth had been treated returned for follow-up, except for three children (one girl and two boys). Finally, 47 subjects were available for follow-up evaluation. The mean age of them was 66.64 ± 10.97 months, including 20 girls and 27 boys. No clinical signs of failure were observed in both types of restorations.
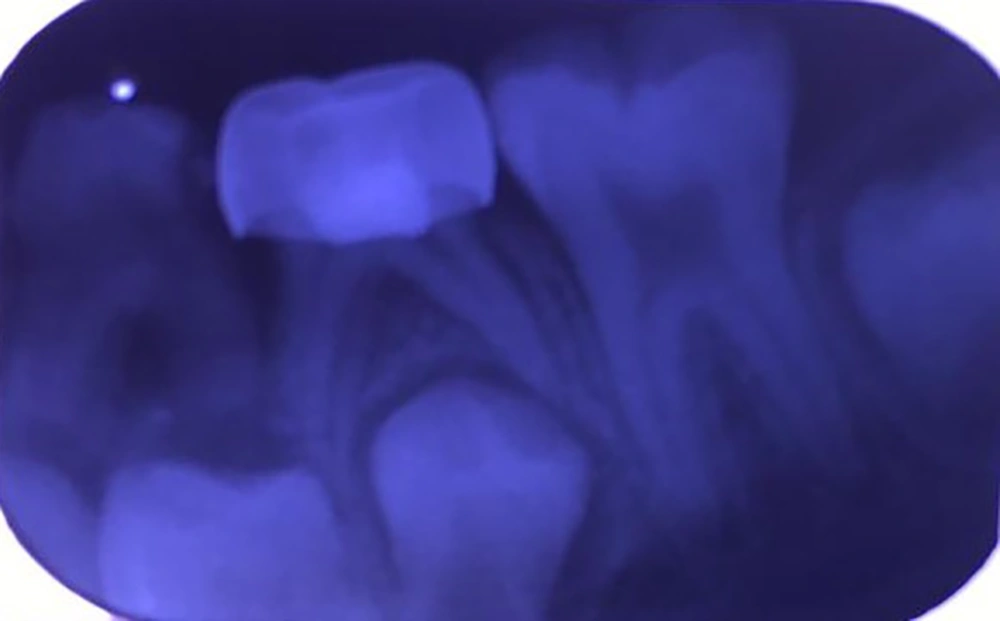
In radiographic interpretation, the intra-rater reliability was established by showing the kappa coefficient of 0.89. In the radiographies, no signs of external root resorption or periapical changes were observed; eight teeth in P/SSC and three teeth in P/GI/SSC showed failure. Figure 5 shows radiographic failure of one tooth in P/SSC technique (furcation involvement). Radiographic findings showed no evidence of failure in both teeth. No pulp canal obliteration (PCO) was reported. Data are shown in Tables 1 and 2. There was no significant difference in the radiographic success (P = 0.198).
| Type of Treatment | Radiographic Success, No. (%) | P Value | |
|---|---|---|---|
| Yes | No | ||
| Pulpotomy-SSC | 39 (82.9) | 8 (17.1) | 0.198 |
| Pulpotomy-GI build up-SSC | 44 (93.6) | 3 (6.4) | |
| Cases of Failure Based on Type of Treatment | Types of Failure | |||
|---|---|---|---|---|
| PDL Widening | Loss of Lamina Dura | Furcation Involvement | Internal Resorption | |
| Pulpotomy-SSC | ||||
| Case 1 | - | - | * | * |
| Case 2 | * | - | - | - |
| Case 3 | - | - | * | * |
| Case 4 | - | * | - | * |
| Case 5 | - | - | * | * |
| Case 6 | - | - | * | - |
| Case 7 | - | * | - | * |
| Case 8 | - | - | - | * |
| Pulpotomy-GI Build Up-SSC | ||||
| Case 1 | - | - | * | * |
| Case 2 | - | - | * | - |
| Case 3 | - | - | - | * |
5. Discussion
All the teeth had clinical success of 100%. All SSCs were intact. In the radiographies, the evidence favored P/GI/SSC, although no significant difference was observed between the two techniques. All treated teeth showed clinical success, whereas radiographic failure was observed in 6.4% and 17.1% of teeth treated with P/GI/SSC and P/SSC, respectively.
Different techniques and materials are available for pulpotomy (17-23). Despite concerns, formocresol is the gold standard (5, 8, 16, 20, 24, 25). Hence, we used formocresol. Further, we used the hard-setting ZOE, which is the most common dressing. Studies have demonstrated the desired outcomes of formocresol pulpotomy (5, 26). In the studies, the success rate was 55% to 100% (8, 27). Although the age range of the subjects and the follow-up period in those studies were different from ours, different results may be influenced by some factors, such as the type of tooth (i.e. maxillary or mandibular; first or second molar); study design; the operator; and child’s cooperation. However, the clinical success of P/SSC was 100%, which was consistent with other studies (1, 4, 5, 18, 19). The radiographic success was higher than 80%, which was also relatively similar to some other studies (5, 27).
In pulpotomy, the likelihood of failure, such as internal root resorption, PDL widening, loss of lamina dura, and furcation involvement, is higher than periapical lesions (8, 27). Accordingly, our study showed the common signs of failure, with no case of periapical lesion or PCO. In previous studies, factors including eugenol, reversible fixative effects, irritative pH of formocresol, inadequate isolation, incomplete and traumatic removal of the coronal pulp, and most likely, undiagnosed chronic inflammation of the radicular pulp, have been reported as the reasons of formocresol pulpotomy failure (18, 23, 25).
In our study, researchers selected the teeth based on the pulpotomy indications and further direct pulp evaluation. However, it should be emphasized that there is no exact conformity between the examination findings and histological condition of the pulp (13). In fact, the accurate diagnosis of a non-inflammatory status of the pulp is a key to predict the healing capacity and prognosis of vital pulp treatment. For this reason, the healing potential of the pulp decreases in cases of undiagnosed chronic inflammation, and the repair capacity of the already inflamed pulp may be further exacerbated through coronal leakage over time (13).
In addition to the medicament, many other factors affect the success of pulpotomy. Contamination of pulp stumps over time has a greater influence than factors such as pulp dressing material (7, 28). Hence, finding the most suitable restoration, which could resist against bacterial leakage over time, has been concerned by researchers. We attempted to compare methods of restoration of GI-SSC and SSC to prevent pulp contamination within a 6-month period.
It is well-known that bacteria should pass through the barrier of materials used beneath restoration before reaching the pulp (13, 15). ZOE has bactericidal effects, which reduce the probability of survival of the microorganisms that reach the pulp stumps as a result of leakage (13, 15). However, the application of ZOE followed by the placement of SSC shows a high microleakage (11, 15) The bacteria toxins, penetrating via the margin of poorly sealed restoration, can pass through the hard-setting ZOE under the restoration and affect the radicular pulp (15). Despite the application of this material under the prefabricated SSC, which doesn’t have a maximum adaptation with the tooth structure, the complicated healing potential of the pulp owing to an undiagnosed inflammation is twice weakened by an ongoing bacterial leakage (13). Therefore, using more definitive material, such as GI, which is capped by SSC, is recommended.
A high success of 80% has been reported for SSCs (14, 15). Many studies emphasized the superiority of SSC to other restorations (13, 14, 29, 30). Despite strong bias towards SSCs, some studies observed no significant difference in the success of pulpotomy after restoration with SSC or amalgam (15, 16, 31).
Despite adequacy of SSC in protecting the crown from fracture, considering the prefabricated entity, the authors believe that SSCs can’t be adapted perfectly and don’t protect the pulp from long time bacterial invasion. Especially as a routine in pulpotomy after dressing the pulp, the remaining part of the cavity is filled with hard-setting ZOE. SSC is then cemented without any definitive restoration beneath it. In addition, the GI luting, applied to cement the SSC, can’t establish a sufficient seal (14). Owing to this inherent drawback of SSCs especially in cases of lower age, pulpotomy failure or restoration loss before natural exfoliation time will be likely.
MTA is the ideal choice for coronal seal (5-8, 23, 25, 32). But it isn’t routinely used in pediatric dentistry owing to its cost, solubility, setting time, and technical sensitivity (5, 25). Hence, searching for the most ideal and practical method, which would predictively increase the success of pulpotomy, is continued.
To the best of knowledge, no study has evaluated the application of GI beneath SSC following pulpotomy in primary teeth yet, which we could use to compare findings. Hence, we mentioned the results of other studies regarding the efficacy of GI to create an intra-orifice barrier during the non-vital bleaching and seal the furcation perforation. One study compared GI with MTA in establishing coronal seal and reported no significant difference (33). In two surveys, promising findings regarding the efficacy of GI as a coronal barrier were reported (28, 34). In the aforementioned studies, as well as others, the models used to evaluate the leakage can’t simulate the actual leakage occurring in the oral cavity. Although these studies can’t be compared with ours in this regard and owing to other methodological parameters, which make the comparison difficult, it can be justified that the GI has equaled with MTA, which has shown many favorable results in several studies.
GI chemically adheres to calcium (28). Another advantage of GI is gradual release of fluoride (28, 35), which reduces coronal leakage owing to antibacterial mechanism (28). A short time was spent for its placement, which is an important consideration for pediatric dentists who routinely treat children. Another advantage of the light-cured GI compared with the conventional GI is that it sets after light curing, and the dentist can immediately perform SSC reduction. Despite the advantages, clinical sensitivity should be considered. Adequacy of GI in establishing the seal can be interpreted by the water absorption phenomena and the resultant expansion, which encounter the polymerization shrinkage of the chemical setting (28).
The authors did their best to eliminate the confounders, such as undiagnosed pulp inflammation via direct pulp observation or pulp contamination during the treatment. By random allocation of teeth into restoration methods and taking into account the uniformity of many factors affecting the success, we believe that the difference in the radiographic success can be attributed to the restoration type. Based on the significant role of coronal leakage in failure, radiographic failure may be attributed to the contamination of the pulpal chamber over time; this event may occur less in P/GI/SS. Although the 6-month superiority of P/GI/SSC was insignificant based on the radiographies, it was in association with the greater seal of GI than of the ZOE.
The treatment success has been followed up in different intervals in studies (8, 31, 36). In most cases, the interval ranged from 1 month postoperatively with 3-month intervals to 1 year. In one survey, no significant effect of increased follow-up time on the primary molar pulpotomy failure was found. They concluded that the trend for failure decreased as the duration of follow-up extended. In other words, there was a likelihood of failure soon after pulpotomy (8). In addition, the effect of definitive restoration on the success can’t be evaluated in equal to or less than 3 months, and decisions on findings that may be indicative of failure or healing potential can’t be made. Hence, we evaluated the success rate over a 6-month period. Another point is the availability of subjects for follow-ups (25). In our study, 47 of 55 subjects (85.5%), underwent follow-up, which is a high rate for follow-up studies.
The study also has some strengths. Pulpotomy and restoration were performed in single appointment, which ruled out the possibility of pulp contamination via interim restoration. All treatments were performed by the same pedodontist. Each subject served as his or her self-control, so the impact of many variables, such as age and sex, was neutralized. Teeth were randomly assigned into methods. Primary mandibular second molars were solely included. So, the effect of tooth type was omitted. The protocol was implemented using communicative management techniques. In addition, the data of a high percentage of children were accessible for follow-up.
Despite some strengths, it is early to conclude the superiority of P/GI/SSC owing to the short follow-up. Although we matched the teeth with regard to the residual tooth structure in each subject, the effect of the severity of tooth destruction on the outcome wasn’t evaluated. For this reason, our findings can’t be generalized. Although P/GI/SSC findings are promising, longer follow-ups and consideration of the effect of residual tooth structure seem necessary to determine the superiority of this method to P/SSC.
5.1. Conclusions
1. Both techniques presented an excellent clinical success.
2. Although the radiographic success rate was higher in the P/GI/SSC than in the P/SSC, no significant difference was detected between them.