1. Background
Pediatric Intensive Care Unit (PICU) is defined as “a hospital unit which provides treatment to children with a wide variety of illnesses of life-threatening nature including children with highly unstable conditions and those requiring sophisticated medical and surgical treatment (1). Pediatric intensive care has substantially improved the health and survival of children that are critically ill. The survival rate of children admitted to Pediatric Intensive Care Units (PICUs) has gradually increased (2-5), primarily owing to PICU resources, such as child-tailored equipment and specialized medical personnel. Therefore, many countries are making efforts to create PICUs.
In the United States, the number of PICU beds has increased beyond what would be expected based on population growth; there was a noticeable growth in the number of PICUs and PICU beds, most of these PICUs had a pediatric intensivist on staff (6). Though it is diverse in structure, there is a high presence of pediatric intensivists and specialized PICU nurses in most European PICUs (7). This way, pediatric intensive care facilities have emphasized the importance of supporting the medical needs of children at risk of imminent death, resulting from acute illness or injury. However, the number of PICUs and total PICU beds remains insufficient in many other countries (8, 9).
In these countries, many critically ill children are treated in Intensive Care Units (ICUs) other than PICUs, which may adversely affect outcomes owing to a shortage of PICU beds. However, there is limited research to compare the mortality rate of children who received pediatric critical care in PICU and those that received it in other ICUs.
2. Objectives
We hypothesized the mortality rate would be lower in children treated in PICUs than in other ICUs.
3. Methods
3.1. Study Population and Data Collection
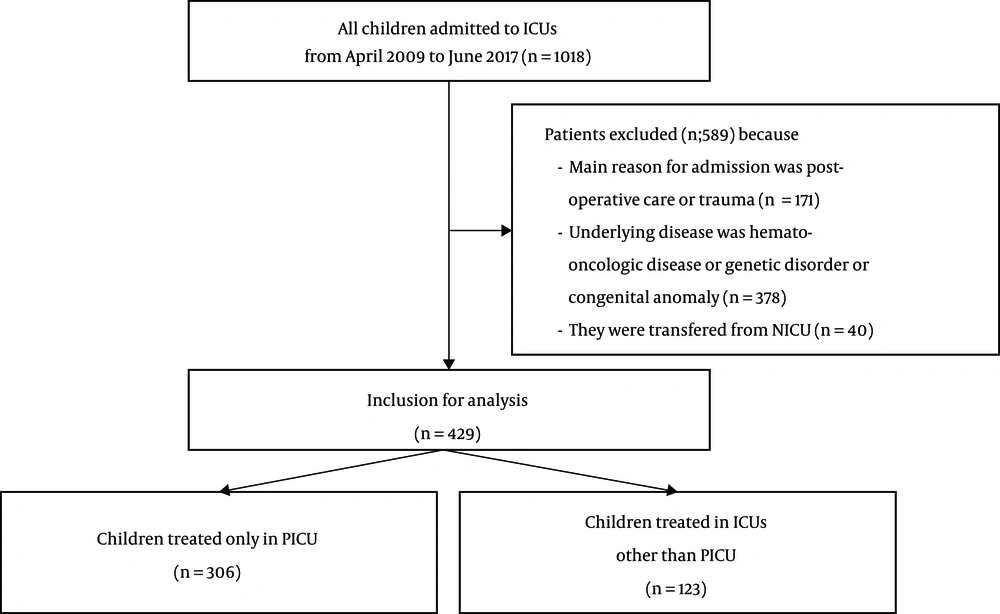
We retrospectively reviewed the medical records of 1018 patients aged < 18 years who were admitted to an ICU in the pediatric department of the Tertiary General Hospital from April 2009 to June 2017. There are six different ICUs in the hospital: medical, cardiac, neurologic, surgical, bone marrow transplant, and pediatric ICU equipped with 20, 18, 19, 22, 5, and 5 beds, respectively. All the six ICUs are “open” ICU where the intensivists have roles of consulting. All the beds of six ICUs have patient’s monitors and ventilator equipment applicable in case of necessity. One pediatric intensivist and ten specialized PICU nurses work in the PICU. In case of shortage of beds in PICU or for coordination with other departments, pediatric patients were also treated in adult ICUs on the responsibility of pediatric intensivists.
Patients were excluded from the study if their reason for admission was postoperative or trauma care; a hemato-oncologic disease, genetic disorder, congenital anomaly, or a transfer from a Neonatal Intensive Care Unit. Among the remaining 429 patients, 306 were treated in the PICU, and 123 were treated in other ICUs (Figure 1).
3.2. Outcome Parameters
The parameters retrospectively analyzed in the 429 critically ill study children were sex, age, source of ICU admission, underlying disease, reason for admission, pediatric index of mortality (PIM)-3 score, length of stay (LOS) in an ICU and the hospital, post-ICU admission respiratory and neurologic complications, ICU mortality, and pathogen infection. The source of ICU admission was divided into two categories: patients were admitted to one of our ICUs owing to symptom aggravation at our hospital, and patients were admitted owing to symptom aggravation outside our hospital. The underlying disease was divided into nine categories: respiratory, neuromuscular, cardiovascular, acute infection, endocrine, gastrointestinal, nephrological, prematurity, and others. The reason for admission was divided into eight categories: respiratory, neurological, cardiovascular, endocrine, nephrological, shock, close monitoring, and others. The PIM-3, which represents disease severity, was evaluated within 1 hour after ICU admission (10). Post-ICU admission respiratory complications, defined as respiratory abnormalities not present before ICU admission, were identified via chest radiography or chest computed tomography. In cases of post-ICU admission neurologic complications, no neurological disease was observed by the medical staff at ICU admission. Pathogen infection included any pathogen in catheter tips, venous blood, central blood, wounds, the nasal cavity, sputum, spot urine, or stool.
3.3. Statistical Analysis
Statistical analysis was performed using IBM SPSS Statistics ver 22.0 (IBM Co., Armonk, NY, USA). The results were expressed as median values [interquartile (IQR) ranges] after the normal distribution was determined using the Kolmogorov-Smirnov method. The chi-square test was used to compare categorical variables between patients treated in the PICU vs other ICUs. A multivariate logistic regression model was used to identify independent risk factors for ICU mortality and was adjusted for the source of the ICU admission and type of ICU. P values < 0.05 were considered statistically significant.
This study (protocol number: KC18RESI0092) was approved by the institutional review board of the Seoul Saint Mary’s Hospital, the Catholic University of Korea.
4. Results
Of the total 429 patients, 306 (71%) were treated only in the PICU, and 123 (29%) were treated in other ICUs. Table 1 shows characteristics of the patients. The PICU group vs the other ICU group differed significantly in terms of admission from our hospital (27% vs 37%; P = 0.043), but not in terms of age (18 months [IQR = 3 - 85 months] vs 26 months [IQR = 4 - 114 months]), P = 0.104), male sex (57% vs 54%, P = 0.587), or mechanical ventilation within 1 hour of ICU admission (15% vs 21%; P = 0.126).
| Variable | Only PICU (N = 306) | Other ICUs (N = 123) | P |
|---|---|---|---|
| Age, mo | 18 (3 - 85) | 26 (4 - 114) | 0.104 |
| Male | 173 (57) | 66 (54) | 0.587 |
| Source of ICU admission | |||
| In the same hospital | 84 (27) | 46 (37) | 0.043 |
| Outside the hospital | 222 (73) | 77 (63) | |
| Mechanical ventilation | |||
| On admission or in first hour | 46 (15) | 26 (21) | 0.126 |
| Underlying diseaseb | |||
| Respiratory disease | 165 (54) | 65 (53) | 0.84 |
| Neuro-muscular disease | 144 (47) | 69 (56) | 0.09 |
| Cardiovascular disease | 42 (14) | 25 (20) | 0.089 |
| Acute infection | 64 (21) | 24 (20) | 0.745 |
| Endocrine disorder | 12 (4) | 6 (5) | 0.655 |
| Gastrointestinal tract disease | 28 (9) | 5 (4) | 0.074 |
| Nephrological or urologic disease | 6 (2) | 3 (2) | 0.755 |
| Prematurity | 38 (12) | 12 (10) | 0.437 |
| Others | 8 (3) | 3 (2) | 0.917 |
| Main reason for admission | |||
| Respiratory disease | 127 (42) | 44 (36) | 0.273 |
| Neurological disease | 89 (29) | 41 (33) | 0.387 |
| Cardiovascular disease | 29 (9) | 18 (15) | 0.122 |
| Endocrine disorder | 8 (3) | 3 (2) | 0.917 |
| Nephrological disease | 2 (1) | 0 | 0.369 |
| Shock | 15 (5) | 6 (5) | 0.992 |
| Close monitoring | 28 (9) | 9 (7) | 0.541 |
| Others | 8 (3) | 2 (2) | 0.54 |
| Pediatric index of mortality-3 scorec | -4.3 (-4.9 - 3.8) | -4.1 (-5.4 - 3.4) | 0.128 |
Abbreviations: ICUs: Intensive Care Units; PICU, Pediatric Intensive Care Unit.
aValues are expressed as No. (%) or median (IQR).
bCategories do not add up to 100% because some patients had multiple underlying diseases.
cPediatric index of mortality-3 was measured at the time of PICU admission.
Most of the patients had one or more underlying diseases before entering an ICU. Gastrointestinal tract disease was more common in the PICU group than in the other ICU group, whereas neuromuscular and cardiovascular diseases were less common. However, these differences, as well as those for the other diseases, were not significant. Respiratory, neurological, and cardiovascular diseases were the major reasons for ICU admission in both groups. The reasons for admission did not differ significantly between the two groups, nor did the PIM-3 score (-4.3 and -4.1 in the PICU group and the other ICU group, respectively; P = 0.128).
Table 2 shows the unadjusted outcomes of critically ill children admitted to an ICU. The LOS in ICU was similar in the PICU group and the other ICU group (5 days [IQR = 3 - 10 days] vs 5 days [IQR = 3 - 15 days]; P = 0.357). Neurologic complications occurred at a similar rate in the PICU vs the other ICU group (4% vs. 2%, P = 0.282), whereas respiratory complications were significantly less frequent in the PICU group (5% vs 11%, P = 0.021). Neurologic complications included convulsion, and respiratory complications included pneumonia, pulmonary hemorrhage, pneumothorax, and pneumomediastinum. The ICU mortality rate (4% vs 11%, P = 0.008) and pathogen infection rate (34% vs 57%, P < 0.001) were significantly lower in the PICU vs the other ICU group.
| Variable | Only PICU (N = 306) | Other ICUs (N = 123) | P |
|---|---|---|---|
| Length of stay | |||
| ICU | 5 (3 - 10) | 5 (3 - 15) | 0.357 |
| Hospital | 11 (6 - 20) | 11 (6 - 25) | 0.317 |
| Complications | |||
| Respiratory | 14 (5) | 13 (11) | 0.021 |
| Neurologic | 11 (4) | 2 (2) | 0.282 |
| ICU mortality | 12 (4) | 13 (11) | 0.008 |
| Pathogen detection rate | 104 (34) | 70 (57) | < 0.001 |
Abbreviations: ICUs: Intensive Care Units; PICU, Pediatric Intensive Care Unit.
aValues are expressed as No. (%) or median (IQR).
In a univariate logistic analysis, the risk of ICU mortality was significantly lower in the PICU vs the other ICU group (odds ratio [OR] = 0.36; 95% confidence interval [CI] = 0.15 - 0.78). It remained significantly lower after adjusting for the source of ICU admission and type of ICU (OR = 0.39; 95% CI = 0.17 - 0.90) (Table 3).
| Variable | OR (95% CI) | P | Adjusted OR (95% CI) | P |
|---|---|---|---|---|
| Other ICUs | 1 | |||
| Only PICU | 0.36 (0.15 - 0.78) | 0.008 | 0.39 (0.17 - 0.90) | 0.027 |
Abbreviations: ICUs: Intensive Care Units; PICU, Pediatric Intensive Care Unit.
aVariables considered for the regression analysis included the following: source of ICU admission; type of ICU.
5. Discussion
Many critically ill children throughout the world, including Korea, receive pediatric critical care (PCC) in adult ICUs owing to the lack of PICUs. We thought that children would benefit more if they received PCC in the PICU than in other ICUs. The study presented here shows that this is indeed the case: compared with critically ill children treated in other ICUs, those treated in the PICU had fewer respiratory complications, pathogen infections, and a lower ICU mortality rate. The ICU mortality rate was significantly lower in the PICU group even after it was adjusted for ICU admission source and ICU type, both of which differed significantly between the PICU and the other ICU group.
In a Finnish study, the authors compared the characteristics and outcomes of the children admitted to the three PICUs with the children admitted to the 26 adult ICUs. The PICU and adult ICU mortality rates reported in the study were 1.1% and 2.1% - 2.7%, respectively. On multivariate analysis, the risk of mortality associated with admission to an adult ICU was almost four times that of admission to a PICU (11). In a study that analyzed 5 years of data in Sweden, the mortality of children admitted to the PICU and adult ICUs were 3.8% and 4.4%, respectively (12). By comparison, the mortality rate was 4% in patients treated in the PICU and 11% in patients treated in other ICUs in our study. The higher ICU mortality rates in our study, compared to previous studies, may reflect its performance at a single hospital and its smaller patient cohort; the Finnish and Swedish studies, which were national-level studies, included about 5,000 - 8,000 patients.
There were no significant differences in age, sex, PIM-3 score, underlying disease, or reason for ICU admission between the PICU and the other ICU groups in our study. Mortality data on ICU patients is usually adjusted using mortality prediction models. PIM-3 score, which was used in our study, provides an international standard based on a large dataset for the comparison of adjusted risk in mortality among children admitted to ICU (10). There are several studies to evaluate the usefulness of the PIM-3 for predicting mortality and to perform regional validations of the PIM-3 score in many countries (13-15). But the previous studies (11, 12) did not have a mortality prediction model of the patients. This prediction model estimates the risk of mortality for children that are admitted to the PICU or adult ICUs, which could vary significantly even among the children admitted in the same ICUs. The two groups, the children admitted to the PICU and adult ICUs, differed in terms of age, underlying disease, and LOS in an ICU in the Swedish study.
Differences in the admission source can also affect ICU mortality rates. Higher ICU mortality rates have been reported for patients transferred from other hospitals (16, 17). However, in our study, most admissions to the other ICUs were from other wards in our hospital, whereas most PICU admissions were from outside hospitals. This is the difference between our study and other studies. According to recent studies, readmission within 48 hours after admission, emergency admission, requirement for mechanical ventilation, and chronic comorbidities are the risk factors for ICU mortality (11, 18). In our study, there were no significant differences between the PICU vs the other ICU group in terms of the requirement for mechanical ventilation or frequency of chronic comorbidities. Readmissions and emergency admissions were not examined.
We attribute our lower ICU mortality rate in the PICU group than in the other ICU group to the proficiency of the PICU nurses and the child-specific PICU equipment. In our study, the fewer respiratory complications of critically ill patients in PICU may reflect their care by nurses who are experts in PCC because PCC is their primary duty. In contrast, nurses who work in other ICUs treat adults exclusively. Hence, nurses in PICUs can take special care of pediatric patients with sputum discharge, or those who require position changes, or other ministrations, which may reduce the risk of respiratory complications. Moreover, their skill in treating nosocomial infections and preparing contamination-free samples for pathogen detection may contribute to the lower rate of pathogen infection in the PICU vs the other ICU group in our study. Because the critical care required by adults and children differs, mainly owing to differences in their disease processes and responses (19), nurses trained in PCC can best tend to pediatric patients (20, 21). Another advantage of PICUs is the presence of equipment suitable for pediatric patients, such as appropriately sized ventilator and endotracheal tubes. Thus, PICUs are better prepared for emergencies than other ICUs.
There are two limitations to our study. First, it was a single hospital study with small sample size. However, statistically significant results were obtained, and its performance at a single site minimizes errors in data collection. Second, the pathogens detected were not classified by type or detection site, which are potential prognostic factors. Unfortunately, our data sources did not contain this information. But despite these limitations, our study is meaningful because it is the first study on the benefits of PICUs in Korea. As another strong point, our study period was 8 years, which is longer than other studies. In the future, multicenter studies should be conducted and pathogen types, as well as sites, should be included in risk factor analyses.
5.1. Conclusions
This study shows that pediatric patients treated in a PICU had a lower mortality rate than those treated in other ICUs. This finding strongly supports the need for PICUs providing PCC. The number of PICUs and dedicated medical staff members are still lower in Korea than in developed countries. We expect that this study will promote the establishment of more PICUs and the training and hiring of more PICU personnel.