1. Background
Hypospadias reconstruction is a common surgical procedure carried out by pediatric urologists and surgeons. The procedure is performed early in life, but the aesthetic and functional aspects acquire greater significance with age. The results of reconstruction have a noticeable impact on self-esteem and sexual behavior in adolescence. The reconstruction requires to address the hypoplasia of the tissues forming the ventral aspect (ventral radius) of the penis (1). The ventral skin is certainly affected in variable degree in this process also.
Once the penile curvature release is completed, a U shaped bare area of skin, variable in size is exposed on the ventrum. The margins of the available skin are usually thin. The routine procedure is midline closure of skin from proximal to distal and pulling and rotating down the distal skin dorsolaterally to the ventrum, and creating the Byars’ or sliding flaps and continuing the midline closure. However, some surgeons prefer to reconstruct the foreskin, but still more surgeons favor circumcision (1, 2). Clearly when the skin deficiency is severe, this procedure may shorten the penile ventrum, create ventral tilting and tethering of the glans. Finally the result is tightened and over-stretched cylindrical thin skin around the distal penile shaft (3). In order to compensate this deficiency, we covered this bare area by quilting the preputial skin island flap. This paper presents the results of this prospective study.
2. Methods
2.1. Patients
Two hundred fifty six hypospadias patients were admitted to the Bahrami Children’s Hospital for repairing surgery, from March 2009 to January 2016. Two of the authors (Mansour Molaeian and Farid Eskandari) performed the procedures in the same manner. The study inclusion criteria were: (1) midshaft to distal hypospadias, including coronal and sub-coronal cases along with penile curvature varying 10 to 25 degrees; (2) presence of severe skin deficiency after release of curvature in which two edges of available skin were located in mid coronal line while the penis was in straight state. 32 patients with proximal or posterior type of hypospadias were excluded from the study. 192 patients were initially operated at our hospital, while 32 had the experience of initial procedure elsewhere. These latter cases had additional scar tissue due to an insufficient procedure on ventral surface in the past but still had an intact and usable dorsal prepuce. The mean age of the patients was 28 months (8 months to 10 years). 182 of the patients had distal type and 42 others had midshaft type. Tubularized incised plate (TIP) repair was performed in 120 patients. Urethral mobilization and advancement with distal triangular urethral plate flap procedure (4) was performed in 32 distal cases, due to narrow and poor urethral plate. The advancement procedure like the MAGPI and the Arap was performed in 30 of the distal cases (coronal and sub-coronal). All of 42 midshaft cases underwent TIP repair. Totally, 162 of patients had urethral suture line. The well vascularized dartus layer of the flap was used as a barrier layer to prevent urethrocutaneous fistula in 147 cases. The right processus vaginalis flap was applied in 15 cases (3 distal and 12 midshaft), due to inadequacy of the available dartus. The patients were followed for 8 months to 7 years.
2.2. Surgical Technique
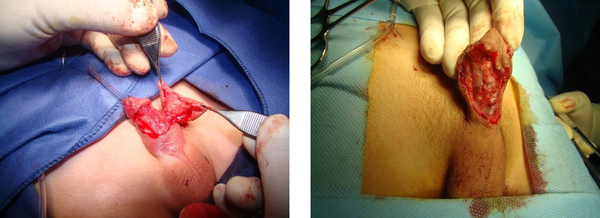
Penile curvature correction was started by skin degloving superficial to Buck’s fascia. This dissection was continued to the penoscrotal junction; more in ventral and less in dorsal portion. We carefully paid attention to avoid damaging the penile skin and preputial vasculature. The penile skin and the prepuce become sufficiently mobile after this dissection. The large bare area was exposed in this stage in ventral surface of the penile shaft varying in length and width. The edges of normal skin were seen to be located in the mid coronal line when the penis was assessed in straight position. We highlight the shortness of ventral skin height in comparison with dorsal penile skin height also. The penile curvature was corrected with penile skin degloving only in 188 patients, but the dorsal plication was needed to complete the correction in 36 patients (Figure 1).
The inner mucosal layer of prepuce was removed without apparently damaging the dartus layer underneath. The penile skin and prepuce were illuminated by front and back lighting using the cold light source to identify the anatomy of vasculature. The presence of one or two predominant arteries with or without communicating branches was confirmed. We incised the skin transversally, at the level of transition of the prepuce into the penile skin. Separation of penile skin from dartus was attempted and continued proximally in favor of preserving of the dartus vessels and leaving the penile skin well vascularized. This separation should be sufficient in length for transferring the flap to the ventral surface of the penis for preventing the future torsion. Proper dissection must be performed to avoid the impairment of predominant arteries.
The flap was rotated around the left side of penile shaft and was fashioned to properly quilt on the ventral bare area as a patch. This flap could cover and align the ventral surface from penoscrotal junction to the sub-coronal cuff and both sides of the shaft. The flap borders with inadequate circulation were excised if needed. Also the thin and poor penile skin around the bare area was excised. The edges of remaining good penile skin were sutured to flap by 6 - 0 vicryl (Figure 2).
Illumination of the prepuce in 28 patients demonstrated no predominant artery (net-like category), therefore, they were excluded from the study. In this type of cases, the Bayar’s flap was created and used only for skin reconstruction.
The penile shaft was wrapped with multiple layers of surgical sponge for dressing including the innermost vaselinated layer during the 5 postoperative days. This dressing was fixed to skin at four points with adhesive strips. This type of compressive dressing immobilizes the penis, prevents skin edema and allows easy observation and evaluation.
The parents were informed about the surgical technique and signed the informed consent form.
In addition to close visits on a weekly basis during 3 weeks postoperatively for wound management, we followed up the patients every 3 months for 9 months and then annually.
In these visits we evaluate the appearance of the penis and its curvature and also the quality of penile skin as a cylindrical long and loose cover around the shaft by examination. It is desired that the penile skin seem as a homogenous plicated coverage around the shaft from the penoscrotal junction up to sub-coronal cuff.
3. Results
All of our patients were discharged the day after surgery and followed up as outpatients. The ischemic changes of the flap as blue discoloration were seen in 7 (3.125 %) patients when the dressing was removed, all finally resulted in flap loss. In these cases we waited for spontaneous recovery for several months and finally reconstructed the ventral shaft skin using local flaps.
Ischemic discoloration at the margins of the flap was another problem which was seen in 12 (5.3%) patients, all of these recovered spontaneously. In this group of the cohort, there were no long-term compromises in the integrity of the flap. The urethrocutaneous fistula was developed in 7 (4 mid and 3 distal TIP) of 162 (4.3%) urethroplasty group. Although, the technique of the creation of the flap and denudation of a portion of it was the same as in others, it probably was inadequate to support the suture line appropriately. In 15 of 162 urethroplasty (3 of distal and 12 of midshaft) we applied the processus vaginalis flap (13 right and 2 left) for this purpose. No urethrocutaneous fistula was developed in cases in which the processus vaginalis flap was used as a barrier layer. Meatal stenosis also occurred in 4 (2.4%) cases of urethroplasty group. The duration of the follow up ranged from 10 months to 7 years (mean 33.92 ± 6.61 months).
On follow up, the persistence of the flap as a hypertrophied area on the ventrum of the penis was encountered in 5 (2.23%) patients, all of which were tailored surgically 9 to 12 months after primary repair.
In the long-term follow up, the appearance of these penises were desirable in regard to size and skin covering (Figure 3).
There was no tilting of the glans downward and no tightened cylindrical and over-stretched skin on the distal penile shaft. The shaft skin looked like a normal and loose penile skin.
4. Discussion
Hypospadias can be defined as a hypoplasia of the tissues forming the ventral aspect of the penis beyond the division of the corpus spongiosum (ventral radius). It is characterized by a ventral triangular defect with its summit being the division of the corpus spongiosum, its sides represented by two pillars of atretic spongiosum and its base the glans. This hypoplasia also influences the ventral penile skin in variable severity (1). The dysplastic process in hypospadias involves the tip to the base of the ventral aspect of the penis (5). The skin is thin, short and adherent to underlying structures. In other words, a V-shaped atretic ventral skin outlines the division of the atretic corpus spongiosum (6). The division of the corpus spongiosum is very often clearly outlined on the mid-ventral thin skin by a small cutaneous ridge (5). The curvature itself is the direct consequence of this abnormal proximal division of corpus spongiosum and the hypoplasia of the tissues sitting in this triangular defect. The skin is tethered on to the underlying structures in most cases. The penile skin in both sides of the defect is also thin, variable in severity (7, 8). Psychological reviews have pointed that parents are concerned about the appearance and adequacy of the penis, and it is now known that reconstruction can provide an almost normal appearance. The result of reconstruction potentially has a significant impact on self-esteem and sexual behavior in adolescence. It has been reported that most patients experience a normal sexual life but they have a more negative genital appreciation (9, 10). Patients with repaired hypospadias perceive a difference in penile appearance and adequacy more frequently than controls. Surveys on adults who have undergone hypospadias repair at childhood reveal that the most important issue regarding satisfaction from various perspectives is penile size (11, 12). Finally, the quality of life of these children might be affected by negative penile self-perception, which can lead to poor school performance and feeling of shame or tantalizing remarks from their counterparts (13, 14).
Hypospadias reconstruction is a common surgical procedure performed by pediatric urologists and surgeons. The systematic process of hypospadias repair includes correcting the penile curvature, urethroplasty, creating the meatus at the tip of the glans, and finally resurfacing of the penis. Traditionally the goals of the repair in children with hypospadias has been focused on urethroplasty and avoiding the fistula and recurrence of curvature. Although surgical techniques have been improved in this field, the parents insist that body image and aesthetics are the patients’ priority.
When the penile curvature is released and urethroplasty, glanoplasty and meatoplasty are completed, a bare area of skin variable in length and width is exposed in ventral surface. The dimension of this area depends on the severity of hypoplasia in ventral radius (1). The margins of remaining skin are usually thin and good quality available skin may be located in the mid coronal line and even beyond. The height of the ventral skin is shorter than the dorsal. In addition to mid hypospadias cases this condition may be found in distal cases. Penile ventral skin coverage by pulling and midline approximation of available skin may leave some disfiguration on the ventrum which impact on the future penile appearance (15). 30 cases in our study group were in this latter category.
Midline closure of the defect and using local flaps are currently practiced. Snodgrass and Bush, have recommended an alternative to Byars’ flaps (8). Removal of preputial outer skin and applying its transposed inner layer and midline closure also has been reported (16). Firlit in 1987, described a dorsal chevron incision to create bilateral “darts” for ventral midline approximation (8). Snodgrass supported this midline approximation of collar mucosal using sub-epithelial and interrupted stiches (16). Also another modification in Byars’ flaps has been reported on this issue (17). The use of the transverse outer preputial (TOP) island flap, and midline approximation of bilateral sub-coronal mucosal “darts” alone, has also been reported (18, 19). The current procedure using ventral mucosal collar approximation provides more satisfaction with age.
The dorsal prepuce in the hypospadias, as a well vascularized tissue, is ideal for reconstruction of the urethra and penile body skin (20). It seems that there may be a communication between superficial preputial and the penis circulation (21). Four main types of vasculature have been recognized in this tissue using trans-illumination and other techniques (22, 23):
Type A: single artery predominant
Type B: two arteries predominant
Type C: H-type arch artery
Type D: no predominant artery but net-like system with fewer distal branches
Similar explorations have been tried on normal prepuce (24). The presence of comparable types of vasculature has been found as well. Different incidences of all four types of vasculature have also been reported in normal and two series of hypospadiac prepuce. The authors accordingly assert the using of only the first three types of prepuce as a flap in urethral and penile skin reconstruction (22, 23). Creation of these flaps requires an in-depth knowledge of the cutaneous arteries and skilled dissection technique, so that they provide greater dimension and reliability in return.
The vascular anatomy of dorsal prepuce harvests from 65 patients with hypospadias has been studied by Perovic and Radojicic (22). They found that 70% of them are well vascularized because of being in type A, B, and C categories. In another study, Yucel et al. reported a rate of 53% for well vascularized group (23). In addition they studied the harvests of 48 normal prepuces. The normal samples were removed from circumcision of normal boys, and reported a rate of 80% well vascularity. All poor vascularized samples in these studies were in type D category (net-like system with fewer distal branching).
One of the advantages of PSIF is the use of its dartus layer as a barrier in urethroplasty cases. This flap has usually a well vascularized tissue, so the upper portion of it can be denuded of the skin and then used as a barrier layer. Sometimes this dartus doesn’t appear sufficient for prevention of fistula, Use of processus vaginalis is a reasonable alternative flap. In 15 of 162 urethroplasties (3 of distal and 12 of midshaft) we applied the processus vaginalis flap (13 right and 2 left) for this purpose
Applying the compressive wrap dressing is noteworthy on early postoperative days. This procedure certainly creates edema in penile skin because it is attempted on loose tissue. However the dressing immobilizes the shaft, provides uniform support to the repair, reduces the postoperative edema, improves hemostasis, prevents disruption, hematoma formation and infection, and eventually enhances overall aesthetic results (24).
According to Snodgrass et al.’s study most of the hypospadias repair complications occur within the first year of the operation (25). Our median follow up was about 33.92 ± 6.61 months. In addition to close visits on a weekly basis during 3 weeks postoperatively for wound management, we followed up the patients 3 months and 9 months after operation, and then annually. In these visits, we evaluate the appearance of the penis and its curvature, and also the quality of penile skin as a cylindrical long and loose cover around the shaft by physical examination. It is desired that the penile skin seem as a homogenous plicated coverage around the shaft up to sub-coronal cuff.
Fading of the flap happened in 7 (3.125%) cases due to ischemic changes of the flap post operatively. Blue discoloration was evident on the time of dressing removal on 5th postoperative day. This complication occurred in cases with fairly medium-sized flaps. All of these cases were followed for an extended period of time. Finally these cases experienced a second surgery for reconstruction. All of them were managed with rotational local flaps. None of them required the skin graft. It must be noted that sufficient vascular anatomy of the flap and saving it by gentle dissection has an important role in flap survival. The rate of ischemic changes is more in the cases with paucity of tissue, which is seen in small penis and also in severe chordee and more severe hypospadias. In Bakal et al.’s study from 10 patients who needed either Byars’ or Ombredanne methods for ventral skin coverage flap, skin necrosis occurred in 50%, although it was superficial and could be mostly treated medically (26).
Persistence of the flap as a hypertrophied tissue in the penile ventrum was encountered in prime 5 out of 224 (2.23%) patients. All of them were revised surgically and resulted in acceptable aesthetic outcome. Proper tailoring of the flap in initial operation can eliminate this obstacle.
The main message of this paper is an attempt to introduce the PISF as an appropriate tissue for cover the large exposed bare area of the ventral surface of the penis in distal and midshaft hypospadias associated with severe ventral hypoplasia. Midline closure by pulling the thin available skin and using the rotational flaps to cover the wide exposed area, may result in skin tethering and downward tilting of the glans and tightening of the skin around the distal shaft . By this alternative the lengths of ventral and dorsal penile skin become equal and all portions of penile skin seem homogenous in appearance and thickness.
Although we use no objective tool and no measurements are taken for evaluating at follow up period, it is our sense and records that these changes in appearance and adequacy are achieved in comparison with midline closure, when the bare area is extensive and there is noticeable difference between the height of dorsal and ventral penile skin. However, in cases of neo-urethral reconstruction the dartus of this flap provides an appropriate barrier layer to reduce the risk of fistula formation and facilitates avoiding the overlap of midline skin suture line over the neo-urethra. Liang et al. in their study also has used a pedicled dartos flap for urethroplasty coverage to reduce urethrocutaneous fistula (27). So this kind of flap can be used especially when there is an urethroplasty. However this technique cannot be used in preputial reconstruction (without circumcision) in hypospadias repair as for saving the blood supply its mobilization requires circumferential dissection of the penile skin (28).
The advantages of preputial skin island flap are as follow: It is a native penile tissue with normal loose dartus and normal sensation. Also it is free and transferable as a flap to the ventrum without rotating the shaft. It compensates the skin deficiency as an adequate tension-free flap in situ. It has capacity of normal stretching during full erection. It causes the penis to look larger, which is an important concern in adults with the history of hypospadias surgery. It potentially provides sufficient material to cover even the one half of the anterior penile shaft. It is available as spare material when a secondary salvage procedure is needed.
4.1. Conclusions
Applying the preputial skin island flap for covering the wide ventral bare area exposing following the correction of curvature in distal and mid-shaft hypospadias along with severe hypoplasia provides more adequate and normal appearing tissue for penile skin reconstruction. This flap provides a homogenous cylindrical skin around the penile shaft and serves as adequate space for full erection in adolescents.