1. Background
Local anesthetics are used to provide effective analgesia for many dental, surgical, and dermatologic procedures. Local anesthetics constitute the most commonly used drug group in dentistry (1). According to their chemical structure, local anesthetics are divided into two groups as amide and ester groups (2). Physicians prefer amide group anesthetics because they provide faster and deeper anesthesia and are generally well tolerated. Allergic reactions due to local anesthetics are seen more in the ester group, but since amide group drugs are used more in clinical practice, the reaction with this group has been reported more (3, 4). Type I hypersensitivity reactions with mepivacaine, lidocaine, bupivacaine, articaine, levobupivacaine, and ropivacaine were the most frequently described (4). Ester group local anesthetics consists of cocaine, procaine, chlorprocaine, tetracaine, benzocaine, and amide group local anesthetics includes lidocaine, mepivacaine, prilocaine, bupivacaine, etidocaine (2). The risk is greater in patients with a history of drug allergy and a history of local anesthetic allergy (5). The frequency of actual local anesthetic allergy is unknown. In some publications, it was reported that the rate is below 1% (5, 6). It is common in non-IgE mediated reactions such as vasovagal syncope and psychomotor reactions due to local anesthetics (5, 7, 8). Type I and Type IV reactions have been defined with local anesthetics. Rarely, it has been reported that immune complex reactions may also occur (3). In Type I reactions, itching, urticaria, angioedema in non-adjacent tissues, bronchospasm, and anaphylaxis may occur (9, 10).
2. Objectives
In clinical practice, history of drug allergy, asthma or atopy in the patients or in their families demand the attention of dentists and allergy specialists for patients who will undergo interventions including local anesthesia procedures. The aim of this study was to evaluate the results of skin tests with local anesthetics and to investigate the factors associated with these results in patients in the Faculty of Dentistry who were referred to allergy specialists due to a history of allergy. In this study, we aimed to determine the relationship between local anesthetic sensitivity in children with a history of atopy or in children with a family history of atopy.
3. Methods
The results of prick and intradermal (ID) tests with local anesthetics of patients in whom surgery could not be performed due to their or their relatives’ allergic disease who were sent to allergy outpatient clinic for testing with the local anesthetics planned to be used in the Faculty of Dentistry between December 2017 and December 2018 were analyzed. Atopic disease, urticaria, asthma, food allergy, atopic dermatitis, and history of drug allergy were questioned and recorded for the patients. The history of urticaria-angioedema due to previous drug use six hours after the rash, hypotension, respiratory distress, and history of anaphylaxis were questioned and recorded. Patients with ongoing food allergy, chronic urticaria, active atopic dermatitis, and patients who had been followed up and treated (inhaler steroid) due to asthma, patients with a history of drug allergy, and patients who had previously described allergic reactions to local anesthetics were included in the study. Patients with a history of drug allergy in the family, patients with food allergy in the family, patients without asthma symptoms, and patients with atopic dermatitis that had improved were not required to undergo testing and were not included in the study. Only one patient with a history of severe anaphylactic reaction due to penicillin in his mother was included in the study.
The patients who underwent prick and intradermal test with local anesthetic were included in the study. Data were collected by examining computer records and test result records. Full dose prick test was performed with one of the amide group non-vasoconstrictor local anesthetic agents (articaine, mepivacaine, lidocaine). NaCl (0.9%) was used as a negative control, and 10 mg/mL histamine served as a positive control. Prick test before each patient. In patients with a negative prick test with local anesthetics, the ID test was performed at 1:1000, 1:100 and 1:10 dilutions, respectively. If ID test was negative, next dilution was started. The ID test was not performed with non-diluted local anesthetics because the false-positive rate is high. When evaluating the tests, if the negative control was 0 mm, induration greater than 3 mm and erythema greater than 5 mm, it was considered positive. Each concentration was assessed by evaluating diameters of erythema and induration formed in the 15th minute and histamine response and negative control. Intravenous fluid, adrenaline, and antihistamines were given and patients were monitored for 24 hours in case of development of systemic reactions. All patients were checked after 24 - 48 hours for delayed reactions. All patients with positive local anesthesia test were tested with another alternative local anesthesia of amide group and no reaction was observed. The second test in patients who were tested for a second time was not included in the study.
Oral and written informed consents were taken from the patients’ parents because all patients were aged under 18 years. Informed consent was obtained from patients between the ages of 12 - 18. The study was approved by the ethics committee of our hospital (Decision number: 2019/01/19). The statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) version 18.0 statistics program. In descriptive statistics, continuous variables are expressed as mean ± standard deviation, median, minimum-maximum and non-continuous variables are expressed as numbers and percentages. In comparisons, Pearson’s chi-square, the Mann-Whitney U and Fisher’s exact test were used. Relationship between test results was evaluated with Fisher’s exact test. P value < 0.05 was considered statistically significant.
4. Results
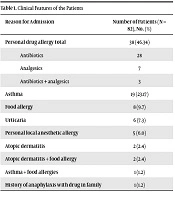
Of the 82 patients, 47 (57.3%) were male and 35 (42.7%) were female. The mean age was 8.43 ± 3.34 (min: 2.9, max: 16.1) years. Table 1 shows the reasons for referral for the test with local anesthetics.
| Reason for Admission | Number of Patients (N = 82), No. (%) |
|---|---|
| Personal drug allergy total | 38 (46.34) |
| Antibiotics | 28 |
| Analgesics | 7 |
| Antibiotics + analgesics | 3 |
| Asthma | 19 (23.17) |
| Food allergy | 8 (9.7) |
| Urticaria | 6 (7.3) |
| Personal local anesthetic allergy | 5 (6.0) |
| Atopic dermatitis | 2 (2.4) |
| Atopic dermatitis + food allergy | 2 (2.4) |
| Asthma + food allergies | 1 (1.2) |
| History of anaphylaxis with drug in family | 1 (1.2) |
Eighty-two patients were tested with local anesthetics. In 71 (86. 5%) of these patients, no allergy was detected as a result of prick test and subsequent ID test. In the study group, prick test was positive in 1 patient (ID test was also found positive in this patient), and the ID test was found positive with a 1:100 concentration in 11 patients (13.4%). There was no difference between patients with positive and negative results in terms of age and sex (P = 0.40 and P = 0.55, respectively).
In 4 of 38 patients with drug allergy, the ID test was positive. There was no difference between patients with and without drug allergy in terms of ID test results (P = 0.32). In 3 of 19 patients with asthma, the ID test was positive. Test positivity with local anesthetics was found to be statistically significant in asthma patients (P = 0.02). The ID test was positive in 1 of 6 patients with urticaria, in 2 of 8 patients with ongoing food allergy, and in 2 of 2 patients with atopic dermatitis. The comparison of the patient groups with positive and negative ID test results with local anesthetics is given in Table 2.
| Patients with Positive ID Test (N = 11) | Patients with Negative ID Test (N = 71) | P Valuea | |
|---|---|---|---|
| Sex (M/F) | 5/6 | 30/41 | 0.55 |
| Antibiotic allergy | 3 | 25 | 0.32 |
| Asthma | 3 | 16 | 0.02 |
| Analgesic allergy | 0 | 7 | 0.66 |
| Food allergy | 2 | 6 | 0.17 |
| Chronic urticaria | 0 | 6 | 0.17 |
| History of allergy with LA | 0 | 5 | 0.48 |
| AD | 2 | 0 | 0.02 |
| AD + food allergy | 0 | 2 | 0.17 |
| Antibiotic + analgesic allergies | 1 | 2 | 0.66 |
| Asthma + food allergy | 0 | 1 | 0.14 |
| History of anaphylaxis with drug in family | 0 | 1 | 0.66 |
Abbreviations: AD, atopic dermatitis; F, female, ID, intradermal test, LA, local anesthetics M, male.
aFisher’s exact test
The ID test was positive in 3 of 28 patients with antibiotic allergy and in none of 7 patients with analgesic allergy.
None of the 5 patients with a history of local anesthetic allergy had a positive ID test (4 with a history of urticaria and 1 anaphylaxis) (P = 0.48). Test positivity with local anesthetics was not significant in patients with history of drug allergy, and history of allergy with local anesthetics. There was only one patient who had a history of anaphylaxis due to drug in their family. The patient’s mother reported severe anaphylaxis due to penicillin; prick and ID tests with local anesthetics were negative in this patient (P = 0.66).
According to the type of previous drug reaction, urticaria was observed in 35 patients, late drug reaction in 1, and anaphylaxis in 2 patients. The ID test was positive in 3 of 35 patients with urticaria (P = 0.17) (Table 3).
| Reaction Type | Urticaria | Late Drug Reactions | Anaphylaxis |
|---|---|---|---|
| Number of patients | 35 | 1 | 2 |
| Intradermal test positivity | 3 | 0 | 1 |
Anaphylaxis findings were found in 2 of 11 patients with ID test positivity to local anesthetics. Two (2.4%) of 82 patients were followed up with a diagnosis of anaphylaxis after performing diagnostic tests for local anesthetics. These patients developed systemic urticarial rash, hypotension, tachycardia, and vomiting 15 minutes after the ID test. Intravenous adrenalin was administered to these patients and they were monitored for 24 hours. One of these patients had antibiotic and analgesic allergies and the other one was tested with local anesthetics due to atopic dermatitis.
Patients with a positive ID test with local anesthetics were tested with another local anesthetic from the amide group (articaine, mepivacaine, lidocaine), which does not contain an additive or vasoconstrictor (adrenaline). The ID tests were found negative with these local anesthetics and as a result, alternative local anesthetics were found for all patients. The second test in patients who were tested for a second time was not included in the study. Six of 11 patients with ID test positivity to local anesthetics were tested with articaine and 5 with lidocaine.
The patient with atopic dermatitis who developed anaphylaxis was tested with lidocaine and the patient with antibiotic and analgesic allergies was tested with articaine. These 2 patients were then tested with mepivacaine and were found negative; it was learnt that they had undergone dental treatment with mepivacaine without any reaction.
5. Discussion
Although local anesthetics are generally well tolerated, reactions due to local anesthetics can be observed. Vasovagal syncope, psychomotor reactions, dose-dependent toxic responses in normal subjects, and allergic reactions in sensitive subjects may occur (7, 8). Although allergic reactions due to local anesthetics are more frequent in the ester group, its use in dentistry is reduced. As a result, complications due to local anesthetics are rare (11, 12). In our study, 86.5% patients did not have any allergies according to prick test and subsequent intradermal test results. This shows that local anesthetics are well tolerated. In our study, a-rate of reaction with local anesthetic was found to be 13.4%, and unlike other studies, 2.4% developed anaphylaxis during test. None of the 5 patients with a history of local anesthetic allergy had a positive ID test. Similar to the literature, none of the 10 patients with a history of allergies to local anesthetics were found to be positive (12). In a retrospective study of 5018 patients treated with local anesthesia, the incidence of adverse effects was found as 0.5%. Only 2 of those 25 patients reported an allergic reaction and most were mild and quickly reversible psychogenic or vasovagal reactions (13). In one study, 168 patients were tested with local anesthetics due to having a history of drug allergy in themselves or in their families. No allergy with local anesthetics was detected in 96.4% patients, and the ID test was positive (1:10 and 1:1 concentration) in 3.6% patients (14). In another study, 30 patients who were referred to an allergy specialist due to having a history of allergy were evaluated. Six patients were not tested due to the recommendation of the consultant allergy specialist, and tests with local anesthetics were positive in only 4.1% patients (12).
As shown in Table 1, the main clinical features of our patients were drug allergy (in 46.3%) and asthma (in 23.2%). In another study where local anesthetic sensitivity was investigated, patients with drug allergy (33. 9%), multiple drug allergy, food allergy (19.9%), atopy (36.9%) including 31 patients with asthma, familial atopy (39.8%), and a history of allergic reaction to local anesthetics (21.6%) were included in the study. Prick and ID tests resulted negative in all 236 patients. A test dose of local anesthetic was then given subcutaneously and no reaction was seen (15).
The relationship between atopic dermatitis and local anesthetics reaction is poor. In our study, 2 of 2 AD patients were found positive by ID test, which is not sufficient to draw conclusions due to the small number of patients.
In our study, intradermal test positivity was found to be statistically significant in asthmatic patients. Although allergic reactions to local anesthetics are rare in the general population, the importance of the problem in children with asthma has not yet been documented. In a study, the sensitivity of local anesthetics in children with asthma was investigated. One hundred fifty-seven children with asthma were compared with non-asthmatic children in the same age group (8 - 15 years). Prick tests, ID tests, and loading tests with lidocaine were performed in all patients. Only 3 patients had a history of reaction to local anesthetics. The tests resulted negative in these patients. As a result, local anesthetic allergy is not seen as a problem in children with asthma, but it is recommended that only those with a history of reaction should be tested and it has been suggested that these drugs can be safely used unless there is a history of emergency-type hypersensitivity reaction (16). As a result of this study, we recommend allergy consultation in patients with asthma when local anesthetic use is required.
In this study, anaphylaxis was observed during ID tests with local anesthetic in 2 patients. The test was performed in one patient because of having antibiotic and analgesic allergies and in the other patient because of having clinical findings of atopic dermatitis. The presence of antibiotic and analgesic allergies in the patient with anaphylaxis is consistent with the knowledge that multiple drug allergy increases risk. Systemic anaphylaxis within 15 minutes following local lidocaine administration was reported in a 4-year-old child (17). In the literature, atopic adult patients with a history of drug allergy were tested, and different from our study, no reaction was reported. Our study group consisted of pediatric patients, which could explain the difference between our study and that study (15).
A study investigated whether the presence of allergic diseases, asthma or atopic dermatitis in the patient or their family increased risk, and no patients with a family history of allergy had a positive result (14). In light of the literature, the test was not performed in patients with familial atopy or asthma and these patients were not included in our study. There are different opinions about the family history of drug allergy. Genetic polymorphism and familial genetic predisposition increases the risk of drug allergy (18). In individuals with penicillin allergy, the risk of allergy with other drugs increases (19). In our study, because patients with a family history of drug allergy were not tested with local anesthetics, they were not included in the study. Only one patient with a history of severe anaphylactic reaction due to penicillin in his mother was tested and resulted negative. In another study, there was no difference between patients with and without a family history of drug allergy in terms of test positivity (14).
In patients with chronic urticaria, non-steroidal anti-inflammatory drugs may exacerbate urticarial (20). In our study, the test with local anesthetic resulted negative in 6 patients with chronic urticaria.
Being atopic increases the risk of the development of severe hypersensitivity reaction. In our study, the ID test was positive in 2 of 2 patients with atopic dermatitis and anaphylaxis developed in one patient during the test. We looked for atopic diseases and found the frequency of local anesthetic allergy as 13.4% and anaphylaxis as 2.4%. These rates were considered as higher than the rates in the general population (5, 6, 13). However, the test resulted negative in all patients with a history of reaction to local anesthetics. There was no relation between test positivity to local anesthetics and, history of drug allergy, history of allergy with local anesthetics.
5.1. Conclusions
Test positivity with local anesthetics was not significant in patients with history of drug allergy, and history of allergy with local anesthetics. Intradermal test positivity was found to be statistically significant in asthma patients. Treatment should be initiated before dental intervention in atopic patients after having the necessary consultations, and treatment should be initiated with local anesthetic agents associated with fewer reactions in emergency situations in risky patients.