1. Background
Congenital heart diseases (CHD) include a variety of malformations defined by Mitchell et al. (1) as the structural abnormalities of the heart and great vessels which exist at birth and have functional response at some point of life. CHD is among congenital anomalies that impose remarkable burden on families and health care system. It includes about 28% of all congenital anomalies worldwide (2). The annual global prevalence of CHD is estimated to be 1.35 million in 150 million live births (3). CHD is more common in Asia, with prevalence of 9.3 per 1,000 live births, mostly due to high consanguinity, especially among Iranians (4).
Patients with congenital heart disease are susceptible to mild malnutrition up to failure to thrive (5). Malnutrition has its highest rate and severity in developing countries (6, 7); although it has a significant prevalence even in developed countries (8). Several factors have been identified to contribute to the occurrence of malnutrition, such as increased mean total daily energy expenditure, decreased energy intake, increased oxygen consumption, disturbed absorption due to bowel congestion, inability of the tissues to use the nutrients and disturbed cellular metabolism due to under oxygenation (9). Children with complex heart lesions need beyond 120% of the common energy intake to have acceptable growth pattern (10, 11). This situation is more critical for children, because besides the increased energy demand caused by CHD, they require more nutrient and energy for growth and neurodevelopment. Children affected by malnutrition are at a higher risk of infection and mortality even after surgery (10). Nutritional challenges often appear at birth or soon after birth and growth impairment is more pronounced during neonatal period, especially for those with hemodynamic-significant defects. Malnutrition causes both short-term complications, including longer hospital and Intensive care unit (ICU) stay, postoperative infection, long-term complications such as impaired neurodevelopment and mortality (11-13). Nutritional assessment and management in these children could result in remarkable improvement, including better results and less complications of the surgery, better growth and neurodevelopment and less imposed burden on the affected families and health care system; however, the first step in this regard, is to identify and evaluate the prevalence and severity of malnutrition and growth impairment on these patients.
2. Objectives
This study aimed to assess the prevalence and severity of malnutrition among patients with CHD prior to the surgical corrective or palliative repair.
3. Methods
3.1. Study Design
This study was performed as a retrospective study, evaluating the medical records of children with cyanotic congenital heart diseases who had undergone palliative or corrective surgery between March 2011 and March 2017 at Children’s Medical Center of Excellence, Tehran, Iran. All patients with cyanotic congenital heart disease, diagnosed by echocardiography had moderate/high risk cardiac defects (Box 1). Children with complex gastrointestinal anomalies affecting the nutritional state, syndromic patients and children with birth weight below 1300 grams were excluded from the study. This study is approved by our institutional board review.
| Cardiac Defects |
|---|
| 1. low nutrition risk |
| Coarctation of aorta |
| Patent ductus arteriosus (if early surgery) |
| Atrial septal defect (minor lesion) |
| Cor triatriatum |
| Transposition of great arteries |
| Total anomalous pulmonary venous drainage |
| VSD (small lesion) |
| Pulmonary stenosis |
| 2. Medium nutrition risk |
| Pulmonary atresia |
| Tetralogy of fallot |
| Atrial septal defect (severe lesion) |
| 3. High nutrition risk |
| Ventricular septal defect (moderate to large) |
| Arterioventricular septal defect |
| Hypoplas11c left heart syndrome |
| Truncus arteriosus |
| Aortopulmonary window |
| Patent ductus arteriosus (if large or delayed surgery) |
| Tricuspid atresia |
| Ebstein anomaly |
| Partial anomalous pulmonary venous drainage |
3.2. Data Collection and Statistical Analysis
All inpatient medical records and cardiac surgery databases were reviewed. patients’ and height at the time of surgery, birth weight, duration of intensive care unit (ICU) stay and 30-day mortality were extracted and weight for age z score (WAZ), weight for length z score (WLZ) and length for age z score (LAZ) were calculated using World Health Organization (WHO) Anthro (version 3.2.2 January 2011) software. Z scores above -1 were considered as normal, between -1 and -2 as mild, between -2 and -3 as moderate and below -3 as severe malnutrition (14). WAZ represents immediate, WLZ acute and LAZ chronic malnutrition. BMI z scores were also categorized in the same way as severely thin, moderately thin, mildly thin and normal (15). The amount and severity (normal, mild, moderate and severe) of malnutrition were compared between males and females. All data were analyzed by SPSS version 22. Qualitative variables are expressed by number (percent) and qualitative variables by mean ± standard deviation. P value less than 0.05 was considered significant.
4. Results
4.1. Study Population
Totally 639 patients were recruited. 359 (56.2%) were male and 280 (43.8%) female without any significant difference (P value = 0.415). The average age, weight and height were 16.688 ± 24.859 months, 7.509 ± 5.629 kilograms and 73.759 ± 95.869 centimeters, respectively. The average length of ICU stay was 8.36 ± 6.254 days. The 30-day mortality was 5.7% (36 cases). The mean birth weight of the subjects was 2986.462 + 443.57 grams.
4.2. Malnutrition Status
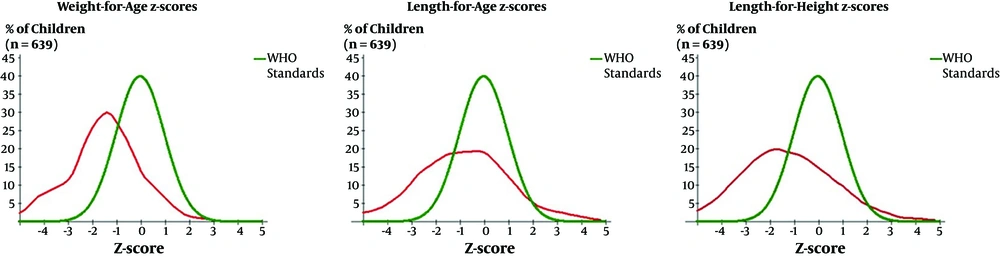
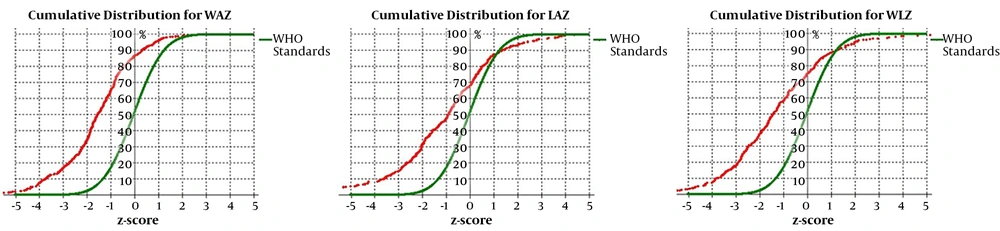
The average WAZ, LAZ, WLZ, and BMI Z was -1.5 ± 1.69, -0.9 ± 2.38, -1.2 ± 3.97, and -1.4 ± 2.11, respectively. Regarding WAZ, LAZ, WLZ and BMI Z, 62.2%, 46.1%, 72.3%, and 70.9% of patients had mild to severe forms of malnutrition, as the rate of malnutrition based on WAZ (P = 0.001), LAZ (P < 0.0001), WLZ (P < 0.0001) and BMI Z (P = 0.007), was significantly higher than normal subjects. (Table 1 and Figures 1 and 2). The severity of malnutrition did not differ between males and females, based on WAZ (P = 0.130), LAZ (P = 0.661), and WLZ (P = 0.125). The mortality rate was not associated with lower WAZ (P = 0.866), LAZ (P = 0.907), and BMI Z (P = 0.357); but was associated with lower WLZ (P = 0.023), birth weight (P = 0.014), weight (P = 0.038), and height (P = 0.026). There was no significant association between length of the ICU stay and severity of malnutrition, based on WAZ (P = 0.203), LAZ (P = 0.295), WLZ (P = 0.734), and BMI Z (P = 0.777). Lower birth weight was associated with more severe malnutrition based on all growth indices (P value < 0.0001).
| Normal (> -1) | Mild (-2 to > -1) | Moderate (-3 to > -2) | Severe (< -3) | |
|---|---|---|---|---|
| WAZ | 238 (37.8) | 188 (29.9) | 105 (16.7) | 98 (15.6) |
| LAZ | 241 (53.9) | 80 (17.9) | 64 (14.3) | 62 (13.9) |
| WLZ | 174 (27.7) | 303 (48.2) | 78 (12.4) | 74 (11.8) |
| BMI-Z | 183 (29.1) | 279 (44.4) | 83 (13.2) | 84 (13.4) |
aValues are expressed as No. (%).
5. Discussion
Malnutrition is a common problem for CHD patients, regardless of the presence of cyanosis and type of cardiac anomaly. In USA, 33% of children with CHD have acute and 64% have chronic malnutrition (11). Determination of the growth disturbance for cyanotic and acyanotic defects has been changed considerably over the past 25 years due to surgical interventions in early childhood, especially for patients with cyanotic lesions. Several factors are associated with the type and severity of the malnutrition, including presence of cyanosis, congestive heart failure, and pulmonary hypertension. Villasis-Keever et al. (16) found that presence of cyanosis, lack of nutritional supplementation and great number of family numbers are among the risk factors of malnutrition. Delayed surgical repair put patients with CHD in greater risk for developing malnutrition (17). In developing countries, the surgical corrections are often delayed, due to high demands for the surgery in a tertiary center, on the other hand, some procedures are preferred to be performed later until adequate weight gain; although this point of view is reconsidered recently (18). Okoromah et al. (9) indicated that the predictors of malnutrition among patients with CHD includes type of CHD, presence of CHF, duration of the symptoms, less than 5 years of age, anemia, lower oxygen saturation and poor dietary condition. All patients in the current study had cyanotic CHD, which causes low oxygen saturation and had a mean age of 16.88 months. As most of cyanotic CHD lesions need to be operated as soon as possible due to becoming symptomatic, 16.8-month duration of having symptoms could cause considerable impact on growth pattern. Cyanotic defects lead to disturbed height and weight growth patterns (19). Linde et al. (20) have indicated that acute and chronic malnutrition is more common among cyanotic patients than acyanotic ones. In the current study, 72.3% and 46.1% of cyanotic patients had acute and chronic malnutrition.
Surgical stress and activation of the inflammatory cascade postoperatively, lead to postoperative endocrine dysfunction, and increased energy requirement which bring about further malnutrition exacerbation (21). Infants and newborns are susceptible to hyper catabolic state postoperatively, due to lower protein and energy reserves, although postoperative hyper catabolism is not a common phenomenon in all patients with CHD (22, 23). Previous studies suggested association between poor wound healing, myocardial dysfunction, and vascular endothelial dysfunction and malnutrition prior to the surgery (24). These findings highlighten the importance of the nutritional assessment and support for these patients.
Lower WLZ, called “wasting”, represents acute malnutrition and lower LAZ, called “stunting”, represents chronic malnutrition (25), lower WAZ also indicates immediate malnutrition. The prevalence of underweight, stunting and wasting in the study of Hassan et al. (26) in 2015 in Egypt reported to be 14.3%, 61.9% and 23.8%; but the prevalence of the aforementioned variables in the study of Okoromah et al. (9) in 2011 in Nigeria were 20.5%, 28.8% and 41.1%, and the relative proportions of the underweight, stunting and wasting in the study of the Ratanachu-Ek (27) in 2011 in Thailand were 28%, 16% and 22%, respectively. Arodiwe et al. (28) found that 66% of the patients had severe malnutrition, and they also found that stunting was more common than wasting. The prevalence of underweight, stunting and wasting in the current study is 70.9%, 46.1%, and 72.3%, respectively, which is remarkably higher than those of other countries. The prevalence of the immediate malnutrition, wasting and stunting in the study of Aghaei-Moghadam et al. (29) in 2019 in Iran among acyanotic patients were 68.7%, 66.4%, and 48.6%, respectively. The prevalence of mild to severe forms of malnutrition, based on different growth indices, for both cyanotics and acyanotics are higher than those reported in the other previous studies. These findings reflect the fact that cultural, genetic and racial differences of Iranians compared to those of others, cause malnutrition to be more frequent in Iranian children diagnosed with CHD. This calls for higher requirement of nutritional support for these patients.
Previous studies have shown that malnutrition is associated with increased mortality and morbidity; it causes frequent hospitalization, poor surgical results and persistent impaired somatic growth (12). Furthermore, protracted and recurrent hospitalization worsen the nutritional status (30). Growth failure in early childhood is associated with delayed mental development, poor school performance and reduced intellectual abilities (13). This study investigated the 30-day mortality rate and length of ICU stay as the short-term postoperative complications. The 30-day mortality rate was 5.7%, which was related to the lower birth weight, weight, height and WLZ. Several studies have demonstrated that malnourished CHD patients have a longer hospital stay length (25, 31). Ross et al. (11) in 2017 found that lower WAZ and LAZ have a significant association with postoperative mortality, cardiac arrest, infection, longer mechanical ventilation and ICU stay. They also demonstrated that the nutritional support for those with growth indices below -2 results in lower mortality rate (11). In line with the previous study, Mitting et al. (25) in 2015 and Eskedal et al. (32) in 2008 found that lower WAZ is associated with higher mortality and increased duration of mechanical ventilation. The mortality rate was associated with WLZ (acute malnutrition), but it was not associated with other growth indices. The length of ICU stay in this study was 8.36 ± 6.254 days, with no association with WAZ, LAZ or WLZ.
Infants with single cardiac defect usually are born with normal weight, but the growth impairment appears thereafter (33), but the scenario is different for patients with more complex heart lesions. In a multi centric study investigating 1245 infants, known cases of univentricular CHD, in North America these patients had a lower birth weight and small for gestational age cases were more among them, compared to the normal subjects. This study concluded that the growth failure process begins during the fetal period which continues after the birth (34). The findings of the present study are in line with the previous study. Lower birth weight was associated with lower growth indices, which represents the impaired weight gain has initiated from fetal period and also that the growth and weight gain of the infants with lower birth weight need to be evaluated by a pediatric endocrinologist or dietician.