1. Introduction
Gaucher disease (GD), the most common lysosomal storage disease, is an inborn error of metabolism caused by the deficiency of lysosomal enzyme glucocerebrosidase. GD is classified into three types: type 1 (non-neuronopathic), type 2 (acute neuronopathic), and type 3 (subacute neuronopathic). Children with type 2 GD may appear normal at birth but manifest systemic and neurological signs by 2 years of age and deteriorate rapidly. Management of type 2 GD can be challenging. Although enzyme replacement therapy (ERT) is generally used for only type 1 and 3 GD patients (1), it is generally accepted that ERT for type 2 GD patients should be discussed with families presenting both its potential merits and the limitations. Here, we present a case of a 3-month-old Japanese girl with failure to thrive and inspiratory stridor. She possessed a compound heterozygous mutation including RecNciI and a novel missense mutation. ERT was started as early as she was 5 months old. We describe the effectiveness and the limitation of early ERT observed in this patient.
2. Case Presentation
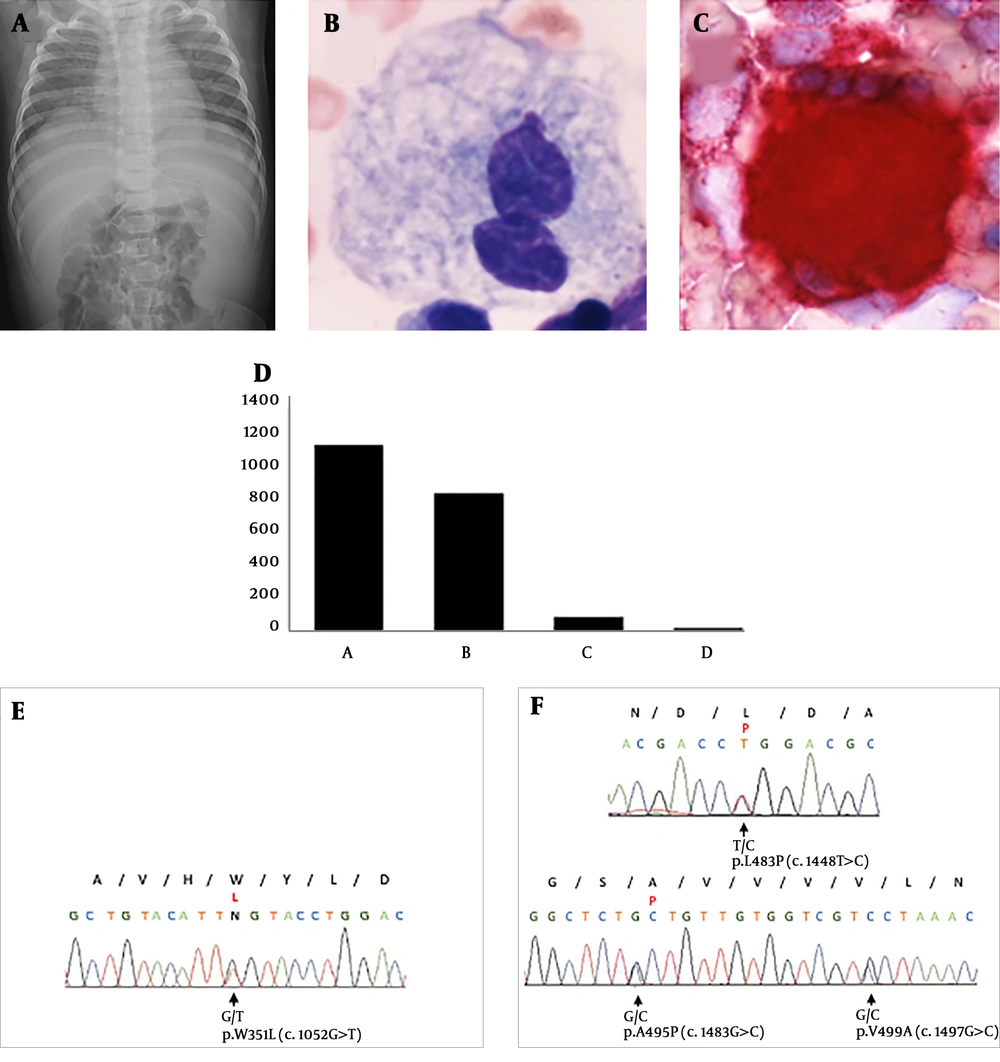
A 3-month-old Japanese girl with failure to thrive and inspiratory stridor presented to our outpatient clinic. She was an appropriate for gestational age baby, who was born at 38 weeks via spontaneous vaginal delivery. She was the second child of non-consanguineous healthy Japanese parents, and she has a healthy older brother. Physical examination and abdominal X-ray revealed marked splenomegaly (Figure 1A). She was diagnosed with neuronopathic GD with elevated angiotensin-converting enzyme and acid phosphatase levels (Table 1), Gaucher cells in the bone marrow (Figure 1B and C), and decreased glucosylceramidase activity in cultured fibroblasts (Figure 1D). Genetic analysis by direct sequencing of amplified PCR products of all 12 exons and flanking regions of GBA (NM-000157.3) was performed after obtaining informed consent from her parents (Figure 1E). It revealed two heterozygous mutations: a recombinant mutation RecNciI in the GBA pseudogene and the novel missense mutation c.1052G > T (p.W351L). After discussing the treatment plan with her family, we administered velaglucerase alfa (VPRIV®, Shire US Inc) at 60 unit/kg once in two weeks at 5 months of age. Clinical response was mainly observed regarding the neurological involvement, splenomegaly, and ichthyosis. We observed gradual improvement in inspiratory stridor, failure to thrive, and hypertonicity. In addition, the patient was able to smile and roll over, which satisfied her family. Splenomegaly improved after a few months. The patient developed ichthyosis as a complication of GD, which exhibited a transient but clear response to ERT. Unfortunately, the patient exhibited sudden neurological deterioration at 8 months of age, triggered by an episode of septic shock caused by methicillin-resistant Staphylococcus aureus. The patient underwent tracheostomy and gastrostomy. At 2 years of age, the patient remains bed-ridden and suffers from frequent systemic dystonic postures and seizures.
A, Chest and abdominal X-ray obtained at admission shows markedly enlarged spleen; B, Gaucher cells in bone marrow with Wright-Giemsa stain. Large histiocytic cells with striated, fibrillar pale-blue to gray cytoplasm; C, Gaucher cells are positively stained with acid phosphatase stain; D, glucosylceramidase activity in cultured fibroblast (nmol/h/mg); A and B, healthy control; C, another patient with Gaucher disease (86.7); D, patient in this report (11.1); E, genetic analysis of maternal; and F, paternal GBA; E, the patient’s parents are the carriers of GBA mutation in exon9 p.W351L (c.1052G > T); and F, exon11 RecNci I (p.L483P, p.A495P, p.V499V). The compound heterozygous mutations of GBA were identified in the patient. The sequences are presented according to the NCBI reference sequence, NM-000157.3.
| Variable | On Admission | 3 Months After Treatment |
|---|---|---|
| Hematocrit, % | 35.4 | 39.3 |
| Hemoglobin, g/dL | 12.0 | 13.4 |
| White-cell count, ×103/µL | 9.3 | 10.6 |
| Differential count, % | ||
| Neutrophils | 30.2 | 38.5 |
| Lymphocytes | 56.3 | 49.8 |
| Others | 13.5 | 11.7 |
| Platelet count, ×104/µL | 21.2 | 28.5 |
| AST, IU/L | 93 | 54 |
| ALT, IU/L | 45 | 33 |
| LDH, IU/L | 344 | 277 |
| Creatine kinase, IU/L | 60 | 99 |
| ACE, IU/L | 63.7 | 39.0 |
| ACP, IU/L | 94.1 | - |
Abbreviations: ACE, angiotensin converting enzyme (normal range: 7.7 - 29.4); ACP, acid phosphatase (normal range: 5.4 - 14.3); ALT, alanine aminotransferase; AST, aspartate transaminase; LDH, lactate dehydrogenase.
3. Discussion
Among all GD subtypes, type 2 shows the poorest prognosis owing to its rapidly progressive neurological symptoms. Affected children may appear normal at birth but manifest systemic and neurological signs by 2 years of age and deteriorate rapidly (2). GD type 2 accounts for 24% of all GD subtypes in Japan (3), while less than 1% of all patients with GD are classified as type 2 based on international registry (4). The genotype-phenotype relationship in GD has not been fully elucidated, except in case of a few mutations, such as N409S, in type 1 (non-neuronopathic) GD. Differences in prevalence of GBA mutations in Japanese patients may explain the high incidence of type 2 GD in Japan compared with other regions. International data suggests that N409S accounts for approximately 53% of mutations, but in Japan, L483P (41%) and F252I (14%) are the two most common mutations in neuronopathic GD (5, 6).
We identified a compound heterozygous mutation including RecNciI and c.1052G > T (p.W351L) in GBA in this patient. RecNciI is a well-known recombinant allele in type 2 GD (7). In contrast, c.1052G > T is a novel missense mutation that has not been reported previously. We consider this mutation to be pathogenic because both SIFT and PolyPhen2 predicted that this mutation was disease-causing. In addition, the c.1052G > T mutation causes a substitution of an evolutionarily conserved amino acid in eukaryotes, and other substitutions of W351R and W351C have been reported in GD (8, 9). Furthermore, genetic analysis of parental GBA revealed the segregation of RecNciI and c.1052G > T in both parents.
The presentations of type 2 GD include failure to thrive, feeding difficulties, laryngeal spasm, seizure, opisthotonus, splenomegaly, interstitial pneumonia, anemia, and thrombocytopenia (10). There is no evidence that ERT improves neurological involvement because the recombinant enzyme does not cross the blood-brain barrier. Thus, it has been debated if ERT, which is a very costly treatment, in patients with type 2 GD is justified. To our knowledge, it is generally accepted that ERT should be discussed with families presenting both its potential merits and the limitations. As previously reported, ERT is effective on visceromegaly and hematologic abnormalities in patients with type 2 GD (11). Our patient showed improvement in splenomegaly and ichthyosis, and transient response to neurological involvement. The treatment may have been partially effective immediately after introduction because the patient gained motor development and became free of opisthotonus. However, her neurological symptoms rapidly worsened after an episode of septic shock, and ERT did not decelerate her neurological deterioration.
Our case supports the current evidence that ERT for type 2 GD does not alter the fatal neurological outcome or delay the neurological progression as a consequence. Further investigation and new treatment options, such as gene therapy, pharmacological chaperones, and histone deacetylase inhibitors (12), for type 2 GD are required.