1. Background
The patent ductus arteriosus (PDA) is the cause of more than 10% of congenital heart defects and it is more common among female infants than males (1, 2). The clinical symptoms depend on the volume of shunted blood from aorta to pulmonary artery bed, which is related to a diameter of duct and pulmonary vascular resistance.
As we know, untreated PDA can lead to an obstructive pulmonary disease, pulmonary hypertension, heart failure, and even increased risk of necrotizing enterocolis in premature infants (3). In premature infants, medical treatment is usually the first option and surgery is only considered when drug treatment is proved ineffective (4). Although the PDA ligation procedure is simple, three complications related to ligation including procedure-induced bleeding, unintended ligation of aortic, left pulmonary artery or its branches may occur (1). As a result, recently attempts have been made to find techniques that minimize these side effects.
One of these techniques is VATS. The present study aimed at evaluating patients with PDA who underwent VATS surgery during 2003 - 2016.
2. Methods
This is a retrospective descriptive study in which the medical records of 129 infants who underwent PDA ligation during 2003 - 2016 in Ghaem Hospital, Mashhad, Iran were assessed. All operations were performed by the same surgeon and in all cases the necessity of the surgery for PDA ligation was confirmed by a pediatric cardiologist.
Information on 30-day mortality, lengths of intensive care unit (ICU) stay and total hospital stay, comorbidities and complications, including pulmonary complications, residual shunt and need for chest tube insertion was extracted from medical records and subjected to descriptive analysis.
All candidates for the VATS closure were referred to pediatric cardiologists. After arrival in operating room and standard monitoring, anesthesia was induced by sevoflurane or ketamine, fentanyl and atracurium. For maintenance, propofol infusion and fentanyl were used. Tracheal intubation was performed with an uncuffed endotracheal tube. An esophageal stethoscope was inserted after intubation.
All patients were positioned in right lateral decubitus. Three 5-mm incisions were created: anterior to scapula, posterior to scapula and tip of scapula. After dissection of PDA from aorta and pulmonary artery, and exposing of PDA, two clips were used for closure. Vanishing of PDA murmur was checked with an esophageal stethoscope.
The patients were extubated in the operating room or early in ICU.
We excluded all PDAs sized larger than 1 cm and patients that needed other operation(s) besides PDA closure.
3. Results
In this study, 129 patients underwent surgery during 2003 - 2016. Forty-six patients were males with the mean age of 35.44 months (age range, 2 to 144 months). More than 51% of the patients were under the age of 24 months. The average weight of the patients was 12.5 ± 6.89 kg (range, 4 to 40 kg). Six patients (4.65%) had a Down syndrome and 13 patients (10.07%) had other abnormalities like ventricular septal defect (VSD), patent foramen ovale (PFO), and floppy mitral valve. In 12 patients (9.3%), thoracotomy was performed following VATS. It was due to technical problems like bleeding, and distorted anatomy. The average operation time was 0.52 hours. In 6 patients (4.65%), a drain was inserted. Two subjects (1.55%) had pulmonary complications and one showed residual shunt and was reoperated. The average length of stay in ICU and hospital was 2.89 hours and 1.78 days, respectively. There was no mortality in this period. The observed complications were as follows: there was one recurrent laryngeal nerve injury (with hoarseness); we also had two cases of chylothorax one of which is managed surgically. The 30-day mortality was zero.
The characteristics of the patients in the VATS group and the group that was eventually converted (thoracotomy) are shown in Table 1.
| Characteristics | Frequency | |
|---|---|---|
| VATS | Convert | |
| Recurrent laryngeal nerve injury | 1 (0.77) | 0 |
| Chylothorax | 2 (1.55) | 0 |
| Down Syndrome | 6 (4.65) | 0 |
| Other associated anomalies | 13 (10.07) | 0 |
| Chest tube | 6 (4.65) | 12 (100) |
| Residual shunt | 1 (0.77) | 0 |
Abbreviation: VATS, Video-Assisted Thoracoscopic Surgery.
aValue are expressed as N. (%).
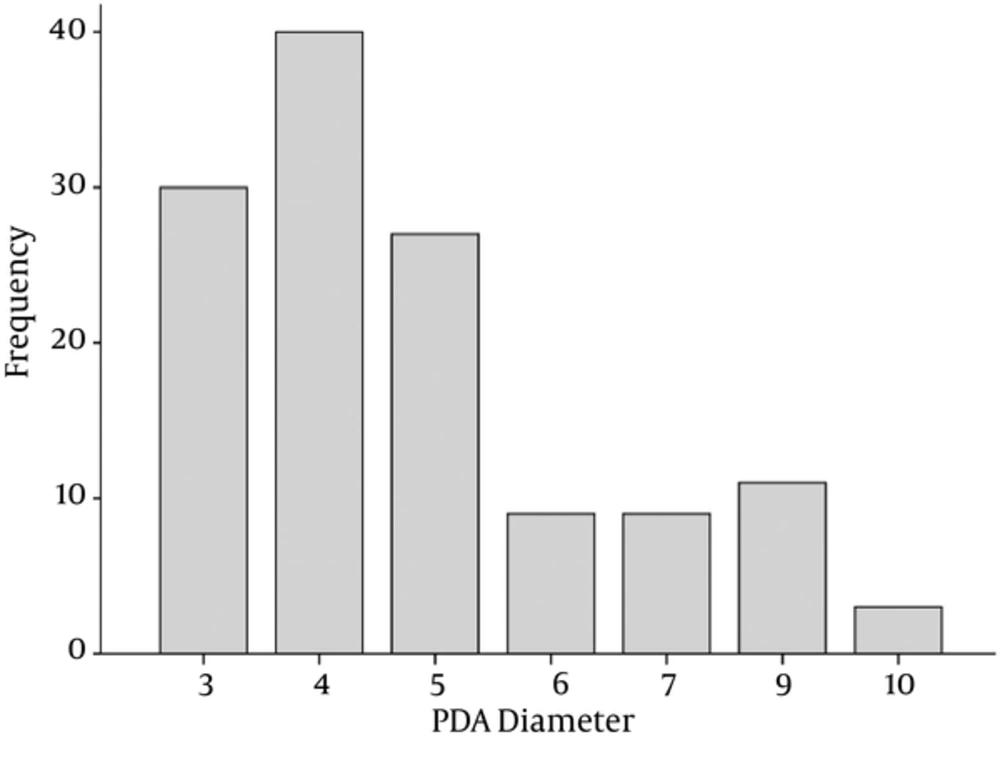
Some patients had disease other than PDA including 3 cases (2.32%) of VSD, 3 cases (2.32%) of PFO, 2 cases (1.55%) of dilation AO, 2 cases (1.55%) of dilation LA and LV and one case (0.77%) of Floppy mitral. The PDA diameter is reported in Figure 1.
4. Discussion
As we know, the PDA is one of the most common heart diseases in infants. Recently, there has been a tendency to perform this surgery by the VATS. Many studies have been conducted to examine the mortality rate of this method. For example, Satoko et al. (2016) reported a mortality rate of 9.9% and neurological disorder prevalence of 21.1% in this method (5), which depicts a declining trend compared to the previous studies (13% and 44%, respectively) (6). In our study, the 30-day mortality rate of patients was zero, though investigation with a larger sample size is required to confirm the results.
A meta-analysis by Weiz et al. in 2014 showed that the VATS surgery reduced mortality in patients, but it increased the prevalence of neurological disorders, respiratory problems and eye complications (7). The current study, however, did not report any of the complications observed in the mentioned study.
There were two important advantages in this method: first, cosmetic benefit for children that may be very important especially in psychological problems, and the second advantage, avoiding chest tube insertion in more than 95% of the patients that allowed us to discharge them earlier from the hospital. It is important that the surgery was performed in early ages. Alipour et al. study has addressed it (8).
The limitations of this study included its retrospective and single-center nature. However, the results suggest that the VATS surgery can be performed more conveniently with fewer side effects.
4.1. Conclusion
Results of this study showed that the PDA surgery by the VATS method can reduce the mortality rate, complications and side effects.