1. Background
In the diagnostic and statistical manual of mental disorders (DSM-5), the fifth edition, obsessive-compulsive disorder (OCD), and similar related disorders are sorted in a spectrum and classified as a separate subtype (1). In this spectrum, OCD is the most problematic disorder, which can disrupt the interpersonal, occupational, and personal life of the patients imposing substantial economic and social costs on the individual and society (2).
The behavioral approach to OCD emphasizes on compulsive behaviors that persist through negative reinforcement (3). This theory recommends behavioral therapies for OCD, including exposure/response prevention (ERP). However, one of the most critical limitations of ERP is that almost half of the patients do not respond to these treatments, do not complete their treatment, or are resistant to it (4, 5). In other words, half of the patients with OCD show signs of recovery after receiving one course ERP (6). In detail, 75% to 80% of these patients report symptom reduction, and only 40% to 52% are cured (7-9). Besides, almost 25% of the patients fully complete the treatment (10).
Given the above problems, the question that arises is how to help OCD patients in whom ERP has not had a significant effect, even in combination with medication (11). Although eye movement desensitization and reprocessing (EMDR) has already been supported empirically for the treatment of post-traumatic stress disorder (PTSD), its impact as an alternative treatment on OCD has also been examined in recent studies. Several uncontrolled case studies and two randomized controlled trials have reported the success of using EMDR to reduce OCD symptoms (11-14).
Preliminary studies have suggested that EMDR can be an appropriate alternative treatment for ERP in OCD (15). To have desirable progress in the treatment of OCD, in-vivo desensitization (exposure), and work on OCD-related events using EMDR therapy should be considered. Because of focusing on practical exercises in standard treatment, patients learn to leave compulsive behaviors and resist doing obsessive behaviors in real-life situations. With the help of EMDR therapy, they could better integrate the emotional aspects of problems and transfer their emotional learning to daily life and tolerate emotional distress. Therefore, the combination of EMDR with OCD standard treatment has been introduced (15-17). Results of studies have shown that the combination of both methods can reduce OCD symptoms in the long term. Compared to ERP alone, the combination of EMDR and ERP reduces the dropout rate and creates higher motivation in patients (15). Like many psychiatric disorders, OCD is also affected by stressful life events both at the beginning and during the disease. Studies have shown preliminary evidence about the relationship between stress and OCD (18). Stressful life events in general and traumas, in particular, have a contribution to the development of OCD symptoms both in the non-clinical and clinical population through the creation of intrusive thoughts and potential obsessive impulses (19). Studies have shown that OCD, like PTSD, can be initiated after facing a traumatic experience or stressful event (20), and the risk of OCD development in people with PTSD is 10 times more than those without problems related to trauma (21). Therefore, people with traumatic and stressful experiences are more likely to be diagnosed with OCD (22, 23).
In addition, obsessions/checking and symmetry/ordering are specifically associated with traumatic life events. Based on the model of adaptive information processing (AIP) in EMDR therapy, psychiatric disorders are often the result of unprocessed traumatic events (24). Although the presentations of OCD are different from that of PTSD, but there are some similarities, like repeated intrusive images and thoughts recalling anxiety and extreme avoidance. Many case studies have also shown qualitative/metaphorical relationships among the contents of obsessive intrusions. Emerging studies and hypotheses suggest that EMDR may be a useful treatment option for OCD (25). Since its introduction, EMDR has been utilized successfully for the treatment of psychological consequences related to many traumatic events (26); however, regarding the application of this method in treating OCD, little research is available supporting its impact.
Although the use of EMDR for OCD treatment was predicted by Shapiro and Forrest (24), few studies have used this method combined with other interventions that are effective in treating OCD (14). EMDR has also been shown to inhibit serotonin reuptake (27); hence, this method can be useful in the treatment of obsessions. Considering the specifications of OCD, the development of the EMDR method and its combination with standard therapies to help these patients are the main objectives of this study. Concerning a few studies on this topic, the results of small case series cannot be generalized due to the lack of rigorous design and susceptibility to biases. So far, only the experimental studies conducted by Nazari et al. (13) and Marsden et al. (11) have empirically supported the use of EMDR in the OCD treatment. However, in none of these studies, the presence of stressful life events has not been considered in OCD patients under treatment. Furthermore, in the aforementioned studies, EMDR was not used in combination with ERP.
2. Objectives
Considering all the mentioned points, in this randomized controlled trial, we attempted to examine the effects of a combined serial protocol of ERP plus EMDR and its comparison with standard ERP therapy in patients with OCD who have had stressful life experiences.
3. Methods
3.1. Design
The current randomized controlled trial (RCT) was carried out using the parallel method, and with a pre-test, post-test, and follow-up design among OCD patients referred to the outpatient clinic of 22 Bahman Hospital in Qazvin after a psychiatrist’s diagnosis between April 2018 to May 2019. This study complies with the guidelines of the Helsinki Declaration.
3.2. Sampling
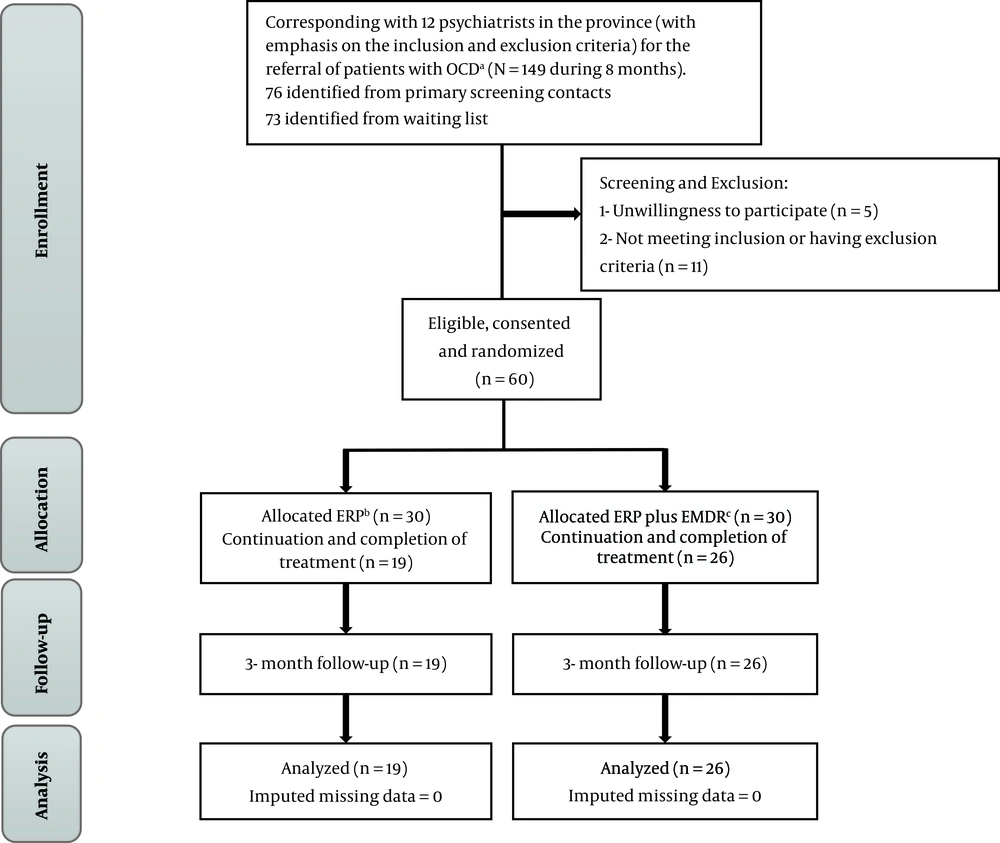
Using Cohen’s table, the sample size was calculated as 50 (25 for each group). According to this table, if the effect size is 0.50 at a significance level of 0.05, selecting 25 samples for each group can achieve the test power of 0.96. Considering the potential dropout, 30 patients were randomly assigned to each group after informed consent forms were obtained from them, and according to the inclusion/exclusion criteria. In the end, 26 patients in the ERP plus EMDR group and 19 in the ERP group completed their treatment. The flow diagram of participants in each randomized trial stage is presented in Figure 1.
The inclusion criteria were preliminary diagnosis of OCD by structured clinical interview related to DSM-5 (SCID-5) (28), Y-BOCS score ≥ 16, having 18 - 60 years of age, having at least secondary education, lack of a comorbid disorder (any kind of psychological or medical disorder) now or in the past except for secondary depression, having subclinical characteristics following OCD, not having substance and alcohol abuse, not having attended any other types of psychotherapies over the past six months, willingness to participate in the study (by completing a written consent form), and having experienced a minimum of one stressful life event (before the onset of OCD) according to the scores of Traumatic Experiences questionnaire (TEC).
The exclusion criteria included having active suicidal ideation and absence in more than one treatment session. Based on these criteria, 60 samples were selected and assigned to the two groups of ERP plus EMDR (n = 30) and ERP (n = 30) by the simple random sampling method. During the initial sessions, 15 samples left the study due to unwillingness to complete the treatment process (4 in the ERP plus EMDR group and 11 in the ERP group). The participants in both groups had a history of using the standard medications for OCD treatment for more than six months without receiving adequate treatment response. At the time of the study, with the prescription of a psychiatrist, they were also using selective serotonin reuptake inhibitors (SSRIs). The ERP plus EMDR group received 12 sessions of EMDR combined with ERP, while the ERP group received only ERP therapy; each session lasted for 75 - 90 min held by an experienced cognitive-behavioral therapist (PhD candidate in Clinical Psychology) with 23 years’ experience in EMDR and ERP (the first author). There was also one follow-up session three months after the end of treatment.
The combination of in-vivo desensitization with EMDR is done in different ways. The standard method is using the alternating technique (25). ERP and EMDR treatments are not combined in one session (15) and can be provided in alternating sessions (17).
3.3. Ethical Considerations
The current study was extracted from a PhD dissertation on Clinical Psychology. The study was approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences (with the ethics code of IR.USWR.REC.1396.301).
3.4. Measures
3.4.1. Demographic Characteristics Checklist
The checklist was developed by the researchers and used for the examination of the participants’ demographic characteristics, including education, marital status, gender, age, job, the onset of the disorder, and history of obsessive-compulsive disorder in the family.
3.4.2. Structured Clinical Interview Related to DSM-5 (SCID-5-CV)
The SCID-5-CV scale functions as a comprehensive standardized tool to examine psychiatric disorders according to the DSM-5 definitions and criteria developed for clinical investigation and research. Numerous studies in various countries have confirmed the reliability and validity of the instrument (28).
3.4.3. Traumatic Experience Checklist (TEC)
This reliable and valid self-report instrument addresses potentially traumatic events and can be used for the purposes of clinical practice and research. Satisfactory indices belonging to the scale internal consistency and test-retest reliability confirmed the TEC reliability. Cronbach’s alpha coefficients were 0.86 and 0.90 for the first TEC administration and the TEC retest, respectively (29). In a study in Iran, Cronbach’s alpha was calculated to be 0.62 (30).
3.4.4. The Yale-Brown Obsessive-Compulsive Scale (YBOCS)
Goodman et al. developed the YBOCS as a scale with 10 items for measuring OCD symptoms. It is scored between 0 (no symptom) and 4 (severe symptoms), with a total score ranging between 0 and 40. Its internal consistency is 0.89 (11). In this study, we used the self-rated Y-BOCS designed by Baer et al., whose cut-off score is ≥ 16. This scale is commonly used to diagnose moderate to severe symptoms of OCD (31). Marsden et al. (11) reported a Cronbach’s alpha of 0.89 for the Y-BOCS. In the Iranian version, its Cronbach’s alpha is reported to be 0.97 (32). In this study, it was obtained as 0.76.
3.4.5. The Beck Anxiety Inventory (BAI)
Beck et al. (33) developed the BAI with 21 items. Each item reflects one of the common symptoms of anxiety and measures its severity in the past week. The items are scored based on a Likert-type scale between 0 and 3, with the total score ranging between 0 and 63; scores between 0 and 21 are indicative of low anxiety, between 22 and 35 are indicative of moderate anxiety, and equal to and above 36 represent high anxiety, which requires follow up and treatment. The BAI has high internal consistency, and the correlation between its items falls within the range of 0.30 - 0.71 (mean = 0.60). The Persian version of BDI has high internal consistency (α = 0.92) and acceptable validity and reliability (34). In the present study, a Cronbach’s alpha coefficient of 0.89 was obtained for BAI.
3.5. Interventions
3.5.1. EMDR with ERP
The EMDR is an eight-phase protocol: (1) Taking history and formulation of the case; (2) preparation to ensure that the clients have the necessary resources for processing the management of disturbing information to achieve an adaptive solution; (3) addressing visual, cognitive (desired positive and negative cognition), sensory and emotional elements of recalls/the target memories are detected, and the level of disturbances and clients’ beliefs in cognition with positive status; (4) recalling the disturbing thought or memory (objective), and simultaneously, performing a set of eye movements (this procedure continues until the subjective units of disturbance (SUD), and validity of cognition (VOC) scales scores reach zero); (5) using further bilateral stimulation to elevate transition into a validated positive cognition; (6) this step is completed when the patient can bring the target memory and cognition with positive status to mind with no physical tension; (7) closing the session after reduction of the patient’s tension; and 8-reassessment, which is repeated at the start of the next session.
EMDR can be an appropriate choice for OCD treatment. This study used the EMDR protocol proposed by Marr, which included the processing of the current motivating factors (obsessions and compulsions of OCD considered as traumatic or current disturbing events), installing a picture of the future (imagining successful actions in the future), and then processing disturbing events occurred in the past (17).
3.5.2. ERP
Exposure/Response Prevention: During the treatment, patients are exposed to some stimuli, including situations, feelings, and thoughts, enabling them to recall obsessive thoughts or painful feelings with no obsessive rituals for distress reduction (response prevention). Exposure was initially provided by imagination (imaginational exposure), and after a significant reduction in symptoms, the patient had real contact (in vivo) with stimuli in the form of behavioral exercises. These methods were systematic and based on the hierarchy of exposure assignments, which gradually become more difficult. With repeated exercises, the SUD scale associated with stimuli and the tendency to obsessive behaviors was used. The ERP treatment was conducted in 5 steps: (1) Evaluation and OCD education; (2) conceptualization of the case and directing therapeutic methods; (3) collaborative development to determine the hierarchy of exposure; (4) performing ERP in sessions and between sessions as homework; and (5) using the ERP program to deal with future potential barriers.
3.6. Data Analysis
For statistical analysis of the collected data, descriptive statistics, repeated-measures ANOVA, Kolmogorov-Smirnov (K-S) test for checking the normality of data distribution, linear correlation test between pre-test and post-test scores, Levene’s test to calculate the homogeneity of variances, ANCOVA, Bonferroni post hoc test and measurement of effect size were used. The analysis was performed using SPSS version 22.
4. Results
Table 1 presents demographic information. According to the results of the analysis, no significant difference was observed between the two groups in terms of gender (P = 0.068), marital status (P = 0.550), age (P = 0.711), and education (P = 0.176), and the dropout rate was significantly higher in the ERP group (P < 0.05).
| Group | ERP | ERP plus EMDR | Test-Statistic |
|---|---|---|---|
| Gender | χ2 = 3.3111; P value = 0.068 | ||
| Male | 11 (57.9) | 8 (30.8) | |
| Female | 8 (42.1) | 18 (62.2) | |
| Marital status | χ2 = 0.357; P value = 0.550 | ||
| Single | 9 (47.4) | 10 (38.5) | |
| Married | 10 (52.6) | 16 (61.5) | |
| Age | χ2 = 0.6812; P value = 0.711 | ||
| < 25 | 8 (42.1) | 8 (30.8) | |
| 25 - 40 | 9 (47.4) | 14 (53.8) | |
| > 40 | 2 (10.5) | 4 (15.4) | |
| Education | χ2 = 0.0362; P value = 0.819 | ||
| Diploma and lower | 9 (47.4) | 11 (42.3) | |
| Associate’s degree | 1 (5.3) | 7 (26.9) | |
| Bachelor’s degree | 9 (47.4) | 6 (23.1) | |
| Master’s or Doctorate | 0 (00.0) | 2 (7.7) | |
| Completion status | χ2 = 4.355; P value = 0.036 | ||
| Completed | 19 (22.50) | 26 (22.50) | |
| Dropped out | 11 (7.50) | 4 (7.50) |
Demographic Characteristics and Dropout in the Two Groupsa
Table 2 presents the descriptive information of the research variables. The mean scores of the research variables in the posttest and follow-up in the ERP plus EMDR group decreased more than those in the ERP group.
| Variables | Pre-Treatment | Post-Treatment | Follow-Up |
|---|---|---|---|
| ERP plus EMDR Group | |||
| BAI | 28.42 ± 10.35 | 8.70 ± 2.43 | 8.46 ± 2.46 |
| Y-BOCS | 24.26 ± 5.00 | 5/50 ± 1.96 | 4.96 ± 1.63 |
| ERP Group | |||
| BAI | 21.15 ± 9.12 | 12.00 ± 2.00 | 14.73 ± 1.79 |
| Y-BOCS | 21.26 ± 3.70 | 7.42 ± 1.07 | 9.47 ± 1.21 |
Means and Standard Deviations of the Studied Variables in Pre-Test, Post-Test and Follow-Upa
While complying with all the assumptions ANCOVA, results for anxiety and OCD symptoms severity are presented in Table 3, which show that the effect of group is significant (Sig. = 0.001), and the EMDR plus ERP protocol significantly decreased the mean post-test scores of anxiety and OCD symptoms severity, even lower than what was achieved by the ERP protocol. Repeated measures ANOVA results of anxiety in the ERP plus EMDR group (Table 4) showed that the effect of treatment was significant (F = 111.031, P < 0.001), hence, there was a significant reduction in post-test and follow-up mean scores of anxiety compared to the pre-test scores. The results for symptoms severity in this group (Table 5) also indicated the significant effect of treatment (F = 332.825, P < 0.001) and a significant reduction in post-test and follow-up mean scores of symptoms severity compared to the pre-test scores. The repeated measures ANOVA results for the variable of obsession severity in the ERP group are presented in Table 5. These results indicate the significant effect of ERP treatment in reducing post-test and follow-up mean scores of obsession intensity (F = 257.527, P < 0.001) compared to the pre-test scores. Bonferroni post hoc test results for the pairwise comparison of the three treatment stages (i.e., pre-test, post-test, and follow-up) for anxiety variables in the ERP group showed a significant difference between pre-test and post-test, pre-test and follow-up, and between post-test and follow-up (P < 0.001). Also, Bonferroni post hoc test results for obsession intensity variable in the ERP group indicated that the significance of repeated measure ANOVA is due to the significant difference between pre-test and post-test, pre-test and follow-up, and post-test and follow-up (P < 0.001).
| Sum of Squares | df | Mean of Square | F | P Value | Eta Squared (η2) | |
|---|---|---|---|---|---|---|
| BAI | 0.625 | |||||
| Constant | 257.614 | 1 | 257.614 | 77.210 | 0.001 | |
| Pre-test | 79.712 | 1 | 79.712 | 23.891 | 0.001 | |
| Group | 233.989 | 1 | 233.989 | 70.130 | 0.001 | |
| Error | 140.134 | 42 | 3.337 | |||
| Y-BOCS | 0.296 | |||||
| Constant | 33.517 | 1 | 33.517 | 12.687 | 0.001 | |
| Pre-test | 6.172 | 1 | 6.172 | 2.336 | 0.134 | |
| Group | 46.582 | 1 | 46.582 | 17.632 | 0.001 | |
| Error | 110.960 | 42 | 2.642 |
ANCOVA Test Results of Anxiety and Obsession Severity for Comparing ERP Plus EMDR and ERP Protocol Treatments
| Intervention | Sum of Squares | df | Mean of Square | F | P Value | Eta Squared (η2) |
|---|---|---|---|---|---|---|
| ERP plus EMDR | 111.031 | 0.001 | 0.816 | |||
| Treatment | 7042.333 | 2 | 3521.167 | |||
| Error | 1585.667 | 50 | 31.713 | |||
| Total | 8628.000 | 52 | ||||
| ERP | 18.793 | 0.001 | 0.511 | |||
| Treatment | 839.719 | 2 | 419.860 | |||
| Error | 804.281 | 36 | 22.341 | |||
| Total | 1644.000 | 38 |
Repeated Measures ANOVA Results of Anxiety Separated by the Intervention Groups
| Intervention | Sum of Squares | df | Mean of Square | F | P Value | Eta Squared (η2) |
|---|---|---|---|---|---|---|
| ERP plus EMDR | 332.825 | 0.001 | 0.930 | |||
| Treatment | 6286.462 | 2 | 3143.231 | |||
| Error | 472.205 | 50 | 9.444 | |||
| Total | 6758.667 | 52 | ||||
| ERP | 257.527 | 0.001 | 0.935 | |||
| Treatment | 2120.456 | 2 | 1060.228 | |||
| Error | 148.211 | 36 | 4.117 | |||
| Total | 2268.667 | 38 |
Repeated Measures ANOVA Results of Obsession Severity Separated by Study Groups
5. Discussion
This randomized controlled trial is the first experimental study using the ERP plus EMDR method for OCD treatment and compared its results with ERP alone as a standard and evidence-based treatment. Rates of attendance and treatment completion were different in the two groups; in the ERP plus EMDR group, 86.66%, and in the ERP group, 63.33% of the samples completed the treatment process. In other words, the dropout rate in the ERP group was twice as high as the ERP plus EMDR group.
Previous studies have revealed that patients with OCD often find the standard ERP treatment tedious and annoying and have little incentive to complete it. According to estimations, 15% - 40% of patients with OCD do not significantly benefit from this standard treatment (35). One reason for this dropout can be due to the strong relationship between stressful life events and OCD (36, 37). Therefore, during treatment, stressful life events should be taken into consideration to achieve integration at the emotional level. Therefore, the present study showed that the combination of ERP plus EMDR significantly increases the treatment completion rate and reduces dropout. In other words, because the EMDR focuses on emotional aspects along with the cognitive and behavioral characteristics of the patients and integrates these different aspects during the treatment process, it is more effective.
Gershuny et al. (35). also believed that EMDR in patients with OCD would improve the regulation of emotions and provide improved recovery from traumatic events by the reduction of emotional distress. In addition, the ERP plus EMDR therapy, besides targeting the obsessive thoughts, tries to treat memories of past stressful life events associated with obsessive-compulsive thoughts. Therefore, it provides the opportunity to reduce the overall emotional anxiety and disturbance more than what ERP can do by dealing with these past events. Consequently, by addressing past events, this method can reduce anxiety and emotional distress more than ERP.
Consistency exists between the results presented above and the findings of other studies that have emphasized the high dropout rate of patients with OCD treated with ERP (4, 5, 7, 9). This study showed a significant difference between the treatments in the outcomes in the post-test phase and during the three-months follow-up, such that interventions with ERP plus EMDR and ERP alone protocols reduced the scores of the anxiety and severity of OCD symptoms significantly; however, the effect of the ERP plus EMDR protocol was significantly higher. This result is consistent with the findings of Gershuny et al. (36) stating that while using EMDR, more attention is paid to the emotional aspects of patients, so their emotions are better regulated. This emotional regulation aspect of the EMDR intervention has led to a more significant reduction in anxiety, as the most critical emotion involved in OCD, thereby reducing the severity of the disorder.
Despite a considerable dropout in the number of patients in the ERP group, the present clinical trial has the potential to predict minor treatment differences, as opposed to the trial conducted by Marsden et al. (11). Our results indicated the higher effect size of the ERP plus EMDR protocol compared to the ERP protocol alone. Moreover, the effect size of the observed anxiety variable was larger than the effect size calculated for the obsession severity variable. By resolving stressful life event experiences of the patients, the ERP plus EMDR protocol reduced anxiety more than obsession symptoms and their severity.
5.1. Strengths and Limitations of This Study
Compared to the previous case series, this study examined a large number of patients randomly assigned to one of the treatment groups; thus, the necessary steps were taken to reduce the bias. The mean Y-BOCS scores of the two intervention groups before the treatment was 22.98, which was within the range of OCD symptoms (i.e., 21.8 - 28.7) reported by previous clinical trials based on this scale (11). Therefore, the study sample was comparable with those of previous studies in terms of OCD severity. Moreover, unlike a few previous clinical trials that compared the EMDR protocol only with a standard OCD treatment such as medication (13) or ERP (11), this clinical trial used the ERP plus EMDR therapy and compared it with the standard ERP therapy.
Furthermore, the present clinical trial is the first controlled study with emphasis and simultaneous intervention on OCD symptoms and stressful life events. Another distinguishing feature of this study is that the patients in both groups were randomly selected from the patients who had provided no adequate treatment responses and had no significant improvement during the past six months of receiving medications (resistant to pharmacotherapy).
The sample size was an important limitation in this study, which does not omit the probability of a slight difference among treatments. The effect size of the post-test reported in the present study can be used for calculating the sample size for future randomized clinical trials. The time and financial constraints of the present research did not allow for a more accurate evaluation of commitment to the study (including the number of sessions recorded to assess the adherence and competence of the clinician). However, like most previous OCD clinical trials (11, 38), the present study also had a short follow-up period, but it did not allow for the evaluation of sustained improvement for more than three months after treatment.
5.2. Conclusions
The results of this clinical trial confirmed that both treatments had sound therapeutic effects. However, the ERP plus EMDR protocol for treating OCD patients with stressful life events had a significantly higher effect and caused a more noticeable clinical improvement compared with the ERP protocol alone. Although some patients left the treatment and showed no improvement in OCD symptoms, and therefore, their pre-test information was removed, the results suggested that the ERP plus EMDR method was a more tolerable and acceptable treatment for these patients. Quantitative and qualitative studies in the future with an emphasis on acceptability and mechanisms of change can be very helpful in better understanding of OCD psychological treatments, and thereby, maximizing their effectiveness.