1. Background
Overactive bladder syndrome (OAB) is a condition in which the patient needs to urinate more frequently. This condition occurs along with frequency and nocturia, with or without urgency, or urge urinary incontinence (UUI) (1, 2). Various dimensions of a patient’s life are affected by its symptoms; therefore, this disorder is considered to be a large socioeconomic burden worldwide (3) that affects the quality of life and living costs (3). The prevalence of OAB has been measured in several regions, including Canada (12.8%), Europe (16.6%), the USA (16.9%), and Korea (12.2%) (4). The syndrome has a considerable effect on the patient's lives, which may result in an increased risk of falls, diminished quality of life, social isolation, sexual dysfunction, and depression (5, 6). There are many hypotheses for the etiology of OAB, including myogenic, peripheral autonomous, or neurogenic sources of detrusor hyperactivity as the prevalent consequences of urodynamic evaluation (7, 8). Although there are possible mechanistic etiologies such as benign prostate hyperplasia (BPH) in men and menopause, or pregnancy in women, its exact etiology is unknown yet (9-11).
Psychological causes of OAB have shown some conflicting findings in this field (12). Various investigations performed in patients with OAB and urinary incontinence have revealed that there is a significant relationship between depression and idiopathic UUI (13). Investigating psychiatric disorders and psychological features with OAB are beneficial for future investigation in detecting the mechanisms of OAB and its treatment (9). Hsiao et al. demonstrated that female patients with OAB suffer from psychological distress, neurotic disorders, and introversion more than normal female cases, and anti-muscarinic medications can help them to improve their psychological distress (9).
In another study in 2016, Ahn showed that female patients demonstrated more obsessive traits on the Korean version of the Maudsley Obsessional-compulsive Inventory total score (P = 0.006) and on the checking subscale (P = 0.001) (14). Obsessive-compulsive disorder (OCD) is characterized by intrusive, troubling thoughts (obsessions), and repetitive, ritualistic behaviors (compulsions), which are time-consuming, significantly impair functioning, and/or cause distress (15, 16).
2. Objectives
The aim of this study was to evaluate the relationship between OCD and OAB in Iranian patients.
3. Methods
This study was a case-control study, which was conducted in a population over 18 years who were referred to the urodynamic clinic of Shohada-e-Tajrish center from June 2013 to February 2018 in Tehran, Iran. The diagnosis of OAB was confirmed for each patient by a single urologist with urodynamic study (UDS) and questionnaire. OAB is characterized as a “symptom syndrome”, marked by urgency, with/without urgency incontinence, and occasionally with frequency and nocturia. All cases had detrusor overactivity (DO) in UDS. The OAB-validated 8-questionnaire screen test (OAB-V8) was conducted too. The diagnosis of OCD was confirmed for each patient by a single psychiatrist according to DSM-5 criteria, and the Yale-Brown questionnaire (17) was completed for each patient to determine the severity of OCD symptoms.
The inclusion criteria for this study were patients ≥ 18 years old, confirmation of OAB by a urologist, OAB-V8 > 8, DO in UDS. The exclusion criteria for this study were urinary infection and history of psychiatric disorders (except OCD). Subjects suffered from multiple sclerosis (MS), a history of cerebrovascular accident, spinal cord stenosis, and a history of pelvic organ radiation, and participants with an incomplete questionnaire and reluctance to enroll in the study were excluded. The control group subjects were patients older than 18 years from the same community who were visited by the same urologist and did not have any symptoms of OAB in their evaluations during the period of the study. None of the control participants had to DO in UDS and urgency in their history. They were referred to UDS clinics for evaluation of true and stress incontinence or lower urinary tract symptoms. There were 580 participants in each group finally. The patient medical history was taken at the initial presentation. Afterward, physical examination, ultrasound imaging of the bladder and kidneys were performed to diagnose bladder stone, diverticula, and mass.
To rate the severity of variables, we used an OAB-V8 questionnaire and the Persian version of Yale-Brown Obsessive-compulsive Scale (Y-BOCS) for our samples (17). OAB-V8 questionnaire, which was validated by test-retest evaluation, consists of 8 questions about lower urinary tract symptoms, according to Ahn et al. study (14). Each question has a 6-point value between 0 (“not at all”) to 5 (“very great”) (18). The validity of OAB-V8 was evaluated by concurrent related validity. The reliability of OAB-V8 was also assessed by internal consistency and reproducibility. Cronbach α was calculated to assess the internal consistency. The calculated optimal levels of internal consistency scores for Q1 (frequency) was 0.77, for Q2 (nocturia) was 0.74, for Q3 (urgency) was 0.76, and for Q4 (urgency incontinence) was 0.78. The correlation coefficient for Q1 (frequency) was 0.83, for Q2 (nocturia) was 0.84, for Q3 (urgency) was 0.79, and for Q4 (urgency incontinence) was 0.71. test re-test method was used to determine the reproducibility. The questionnaire was completed two times during the 10 days by 30 individuals. Test re-test reliability (95% CI) for Q1 (frequency) was 0.78, for Q2 (nocturia) was 0.81, for Q3 (urgency) was 0.70, and for Q4 (urgency incontinence) was 0.73 (18).
To evaluate the severity of obsessive-compulsive symptoms, we used the Persian version of the Y-BOCS. The severity was calculated by considering the higher sub-scale Y-BOCS scores, which is a standard and routine metric for researchers/clinicians. The Y-BOCS is a questionnaire, which assesses the presence and severity of obsessive-compulsive symptoms. It has two parts, including a symptom checklist and a severity scale. The symptom checklist includes 54 items that evaluate present and past obsessions and compulsions. The severity scale contains 10 items that show the effect of obsessions and compulsions. These 10 items are 5-point scales, including the time spent on compulsions (item 1), interference from obsessions (item 2), distress associated with obsessions (item 3), resistance to obsessions (item 4), patients control over obsessions (item 5), and the same items for compulsions (items 6 - 10) (17, 19). The maximum score for Y-BOCS is 40 and various therapeutic studies needed a twenty-score for coverage, which is related to cut-off points for Y-BOCS; 8 - 15 = Mild OCD; 16 - 23 = Moderate OCD; 24 - 31 = Severe OCD; 32 - 40 = Extreme OCD. The Persian validated Y-BOCS has shown good psychometric properties and sensitivity. The calculated optimal levels of internal consistency scores for the symptom checklist was 0.97, and for severity, the scale was 0.95. Split-half reliability for symptom checklist was 0.93, and for severity, the scale was 0.89, and test-retest reliability was 0.99 (17).
For this purpose, participants who reported obsessions or compulsions in the last 12 months before the interview were asked to report the number of weeks in which they experienced obsessions or compulsions more often in the last 12 months and the average number of hours/days involved with obsessions/compulsions. Numeric characteristics were compared in two groups by Student t-test if the distribution was normal or with nonparametric assays in cases of non-normal distribution. The chi-square (χ2) test used to detect the OAB-V8 score was related to the Y-BOCS score in two groups. The P-value of less than 0.05 was considered statistically significant. The association between the OAB and OCD variables was assessed by logistic regression analysis. We measured the odds ratios for the probability of OCD features in case of the existence of OAB. All statistical tests were performed with SPSS version 21 software. After describing the aim of the study and its process, all participants who agreed to enter the study signed the informed consent form. This study was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences with ethical code IR.SBMU.RETECH.REC.1399.863.
4. Results
Of 1,160 cases enrolled, 580 of them were in control, and 580 subjects were in the case groups. The average age of the participants was 47.32 ± 11.47 (18 - 75), and most of them were female (297 in the case and 275 in the control group, respectively). Data about the OAB score and Y-BOCS scores are summarized in Table 1 and compared between the two groups.
| Variables | OAB Group (n = 580) | Control Group (n = 580) | P-Value |
|---|---|---|---|
| Age (y) | 46.87 ± 12.21 | 47.63 ± 13.72 | 0.781 |
| Age group | ≥ 0.5 | ||
| < 20 | 48 (8.28) | 39 (6.7) | |
| 20 - 29 | 106 (18.3) | 96 (16.7) | |
| 30 - 39 | 126 (21.8) | 116 (20) | |
| 40 - 49 | 97 (16.8) | 116 (20) | |
| 50 - 59 | 77 (13.2) | 87 (15) | |
| 60 - 69 | 87 (15) | 78 (13.4) | |
| ≥ 70 | 39 (6.8) | 48 (8.2) | |
| Female | 297 (51.2) | 275 (47.4) | ≥ 0.5 |
| Marital status | |||
| Unmarried | 175 (30.1) | 173 (29.8) | ≥ 0.5 |
| Married | 382 (65.8) | 389 (67) | |
| Divorced | 23 (3.9) | 18 (3.1) | |
| Education | |||
| Primary school | 163 (28.1) | 120 (20.6) | ≥ 0.5 |
| Higher education | 264 (45.5) | 279 (48.1) | |
| University education | 153 (26.3) | 181 (31.2) | |
| Occupation | |||
| Student | 27 (4.6) | 33 (5.6) | ≥ 0.5 |
| Military service | 30 (5.1) | 52 (8.9) | |
| Self-employed | 140 (24.1) | 145 (25) | |
| Homemaker | 204 (35.1) | 186 (32) | |
| Retired | 112 (19.3) | 98 (16.8) | |
| Unemployed | 56 (9.6) | 52 (8.9) | |
| Other | 11 (1.8) | 14 (2.4) | |
| OAB-V8 score | 18.79 ± 13.46 | 1.79 ± 1.68 | < 0.0001 |
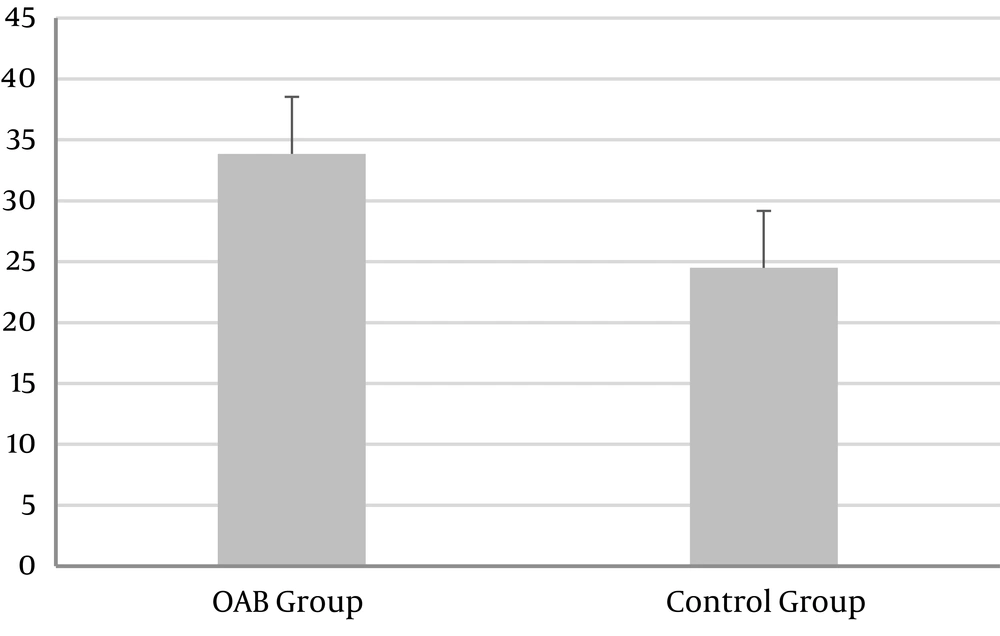
| Y-BOCS score | 33.85 ± 8.07 | 24.49 ± 7.59 | < 0.001 |
| Mild OCD | 78 (13.4) | 309 (53.3) | < 0.01 |
| Moderate OCD | 271 (46.7) | 193 (33.3) | |
| Severe OCD | 231 (39.9) | 78 (13.4) |
Abbreviations: OAB, overactive bladder syndrome; OAB-V8, OAB-validated 8-questionnaire; OCD, obsessive-compulsive disorder; SD, standard deviation; Y-BOCS, Yale–Brown Obsessive Compulsive Scale.
a Values are expressed as No. (%) unless otherwise indicated.
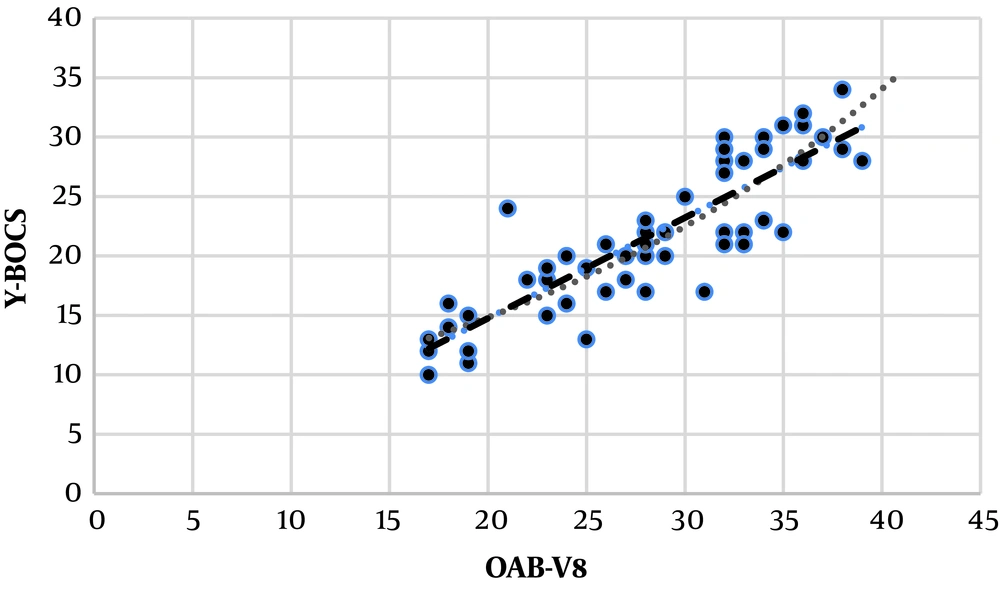
Age was not significantly different in the two groups (P-value < 0.001). Our study population with OAB was more likely to have OCD than non-OAB control group subjects in age classified groups. Frequency (76%) was the most commonly reported symptom among those with an OAB, followed by nocturia (44%) and urge incontinence (29%). The average score of OAB-V8 was 18.79 ± 13.46 in the OAB group. The mean Y-BOCS score ± SD in the OAB group was 33.85 ± 8.07 (Table 1). OCD scores were significantly higher in the OAB group compared to the control group (P < 0.001). As shown in Figure 1, there was no significant correlation between the OAB-V8 score and the Y-BOCS score (r = 0.09, P = 0.219) in the OAB group. However, the patients in the OAB group had a significant relationship in the OAB-V8 score and Y-BOCS score (r = 0.418, P = 0.001) by age adjusting. Logistic regression analysis showed that our study population with OAB was more likely to have OCD than non-OAB control group subjects in age classified groups (OR: 6.23; P < 0.001) (Table 2).
| Characteristics | Wald Chi-Square | P-Value | OR (95% CI) |
|---|---|---|---|
| OAB | 8.98 | < 0.001 | 6.23 (1.29 - 17.45) |
Abbreviations: OAB, over-active bladder; OCD, obsessive-compulsive disorder; OR, odds ratio.
5. Discussion
There are limited data in the field of the correlation between OAB and OCD. Some studies have shown a relationship between OAB and psychiatric disorders such as anxiety disorders (20, 21), and another study have shown a relationship between OAB and psychological stress (22). In a study, it was found that the anxiety score was significantly higher in the subjects with OAB than controls (20).
We revealed that the Y-BOCS score was higher in OAB patients compared with the control group, and OCD was 6.23 times more frequent in OAB patients (Figure 2). In line with our study, Hsiao et al. (9) used the Brief Psychiatric Rating Scale to assess interpersonal sensitivity, somatic, symptoms, obsessive-compulsive symptoms (OCS), depressive symptoms, anxiety, hostility, phobic anxiety, and paranoid traits and found that there are more somatic problems and OCS in females with OAB (9). Their results do not concern OCS and give a wide range of psychological disturbance in OAB patients. However, similar to us, Ahn et al. (14) showed that OCS features are the dominant view of the psychiatric characteristics of OAB patients. They showed that the Korean version of the Maudsley Obsessional-Compulsive Inventory (MOCI-K) scores were higher in the patient group, and female OAB subjects were more probable to gain obsessive-compulsive symptoms than the non-OAB control group. They also showed that in patients with OCD, the OAB-V8 scales were related closely to the MOCI-K scales (14). Similar to this study, we used a standard diagnostic means of OCD, i.e., Y-BOCS, which is an international scale for the severity of OCD and is specific for it. To get more generalizability of the findings, we selected a larger sample size compared to these studies. We diagnosed OAB with both clinical and screening questionnaires (OAB-V8). The diagnosis of OCD was confirmed for each patient by a single psychiatrist with DSM-5 criteria.
There is an important question in this setting and field, either OCD is the cause of OAB, or there is a relationship or co-existence. There is little data in this field, and it is suspected that this linkage can be multifactorial. Our results and previous studies in OCD and OAB relationship (14) demonstrated that this link could be causally related because this linkage is solid with a high odds ratio compared with the control group. In mechanistic relevance, we can mention the serotonergic pathway that is involved in OCD patients, In this regard, there are neuro-imaging results that express lower 5-HT transporter accessibility in addition to higher 5-HTT availability. There is an incidental clue that the 5-HT2A receptor might be of a special contribution to OCD (23). A decline in serotonin levels in the central nervous system is related to urinary frequency and bladder contractions, while stimulation of the central serotonergic system with a 5-HT reuptake inhibitor reduces reflex bladder contractions and elevates the urine volume brink in animal studies (18, 24). Therefore, there might be a linkage between OAB or incontinency via the serotonergic cycle and OCD. Although the mechanisms are biologically reasonable, the proof is primary and is not in a clinical setting; thus, it is necessary to investigate the potential mechanisms.
Despite the well-designed study for lowering the limitations of previous studies, our study had some limitations: We did not collect the demographic and underlying possible risk factors like smoking or dietary, which may affect the results. Moreover, our study did not include men.
We showed that OAB patients reported higher scores in Y-BOCS compared to the controls. There is an independent correlation between OCD and OAB. However, the linkage between OCD and OAB justifies the need for more research. Conducting extensive studies in a cohort design is recommended to follow patients for possible causality pathways and performing mechanistic investigations like neuroimaging beside other standard questionnaires.