1. Context
Low back pain (LBP) is one of the most usual causes for which people follow medical treatments. It is estimated that one in two people will experience LBP throughout their lifetime, and at least 10% of LBP sufferers experience chronic low back pain (CLBP) (1). In 2015, the worldwide prevalence of disability due to LBP was 7.3%, which means that 540 million people are affected by LBP. In fact, LBP is the most prominent cause of disability worldwide (2). The majority of LBP sufferers are between 40 and 80 years old (3). Moreover, CLBP is associated with disability, depression, cognitive dysfunctional, loss of sleep and appetite, and social isolation (4). In addition to human suffering, high economic costs of health-care and indirect costs of job loss or productivity decrease can be counted as other crises of chronic pain (5-9).
In the treatment of CLBP, ordinary treatments such as pharmacological, medical, surgical, are not solely effectual in the elimination of pain or improving emotional and physical functioning (10). International guidelines about CLBP care have focused on treatments that emphasize the active role of patients, including exercise, relaxation, and behavioral changes due to psychological treatments (11). Among psychological treatments, CBT has more evidence in chronic pain research literature. As chronic pain has a complex nature, CBT, like medical treatments, cannot be influential in eliminating and controlling pain (12).
Unlike other treatments, which focus on diminishing and controlling the intensity of the pain, mindfulness-based interventions (MBIs) helps patients without requiring to change pain intensity (13). MBIs taken from ancient Buddha have attracted much attention in contemporary psychotherapy. Mindfulness with the attitude of non-judgmental acceptance is a phenomenon that requires one’s full consciousness. That awareness is accompanied by a careful observation of perceptions, cognitions, emotions, or feelings without good or bad evaluation, right or wrong, healthy or ill, important, or unimportant (14). Two concepts have been identified in mindfulness: self-regulation of attention and orientating to the present moment with curiosity, openness, and acceptance (15). Humans usually are not aware of their moment-by-moment experiences; they seem to be in an auto-pilot mode. Moment-by-moment awareness of experiences can enrich the sense of life in which each experience can be an alive and active mental partnership rather than a subconscious response (16).
The question is whether MBIs with a focus on improving function and active role of the patient can reduce the pain intensity in patients with CLBP. The effectiveness of MBIs in pain intensity in patients with chronic pain is investigated in a review article by Reiner et al. (13). This study reviews 16 articles, 10 of which showed a meaningful reduction in pain intensity of the MBIs groups.
2. Objectives
In this systematic review, we aimed to investigate whether MBIs have been able to reduce short term and long term pain intensity in people with CLBP. Besides, since there is not any review article which investigates Persian articles on this topic, we will also have a Persian search which can enhance the quality of this review.
3. Data Sources
3.1. Search Strategy
We searched six databases, including MEDLINE/PubMed, Cochrane Library, PsycINFO, GoogleScholar, Scopus, and ProQuest in English and Irandoc, Google Scholar, and SID databases in Persian from 2014 to June 2020. The following terms were searched in English databases: MBSR [Title/Abstract] OR MBCT [Title/Abstract] OR Mindfulness [Title/Abstract] OR Meditation [Title/Abstract] AND Low Back Pain [Title/Abstract] OR Lower Back Pain [Title/Abstract] OR Lumbago [Title/Abstract] OR Low Backache [Title/Abstract] OR Low Back Ache [Title/Abstract] OR Mechanical Low Back Pain [Title/Abstract] OR Postural Low Back Pain [Title/Abstract] OR Recurrent Low Back Pain [Title/Abstract]. We also searched the following terms in Persian databases: Mindfulness [Title/Abstract] OR MBSR [Title/Abstract] OR MBCT [Title/Abstract] AND chronic low back pain [Title/Abstract]. The reference lists of identified original articles or reviews were also examined manually for additional eligible studies.
4. Study Selection
Studies were included if they were: (1) RCT; (2) had patients with CLBP of any reason, duration, or intensity; (3) made a comparison between MBIs and a passive comparator (usual care) or an active comparator (such as cognitive-behavioral therapy (CBT) or health education); (4) examined pain intensity.
Studies were excluded if they were: (1) non-randomized trials or observational studies; (2) interventions included individual therapy sessions; (3) had not been published as a full-text; (4) used interventions that had no formal meditation (for example, acceptance and commitment therapy or dialectic behavioral therapy); (5) interventions included other meditations such as yoga, tai chi, qigong, or meditation techniques without referring to the mindfulness. Two reviewers (F.A. and M.H.) independently reviewed all of the recovered articles in full to determine their eligibility for inclusion. Discrepancies between the reviewers were resolved by consensus of the third reviewer (H.H.).
5. Data Extraction
Two reviewers independently extracted data from the eligible articles. We studied full texts of the final articles and extracted some information about article characteristics (including trial design and randomization), sample characteristics (including sample size, age, sex, and diagnosis), intervention and comparison group characteristics (including type, program length, and frequency and duration of sessions), pain intensity characteristics (type of measuring tool, short and long-term outcomes), and information about follow-up length and outcome. Discrepancies between the reviewers were resolved by consensus of the third reviewer (H.H.).
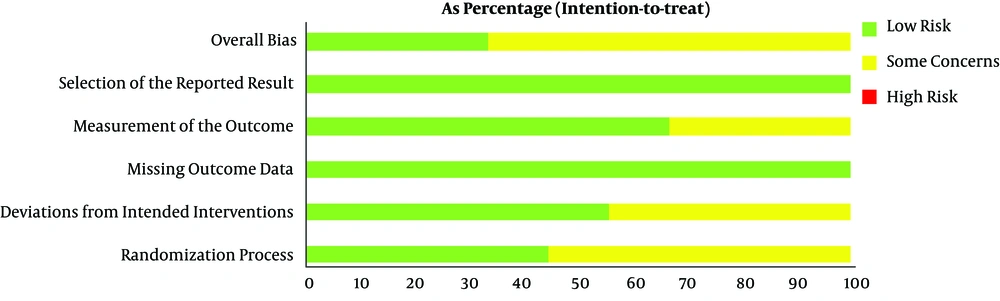
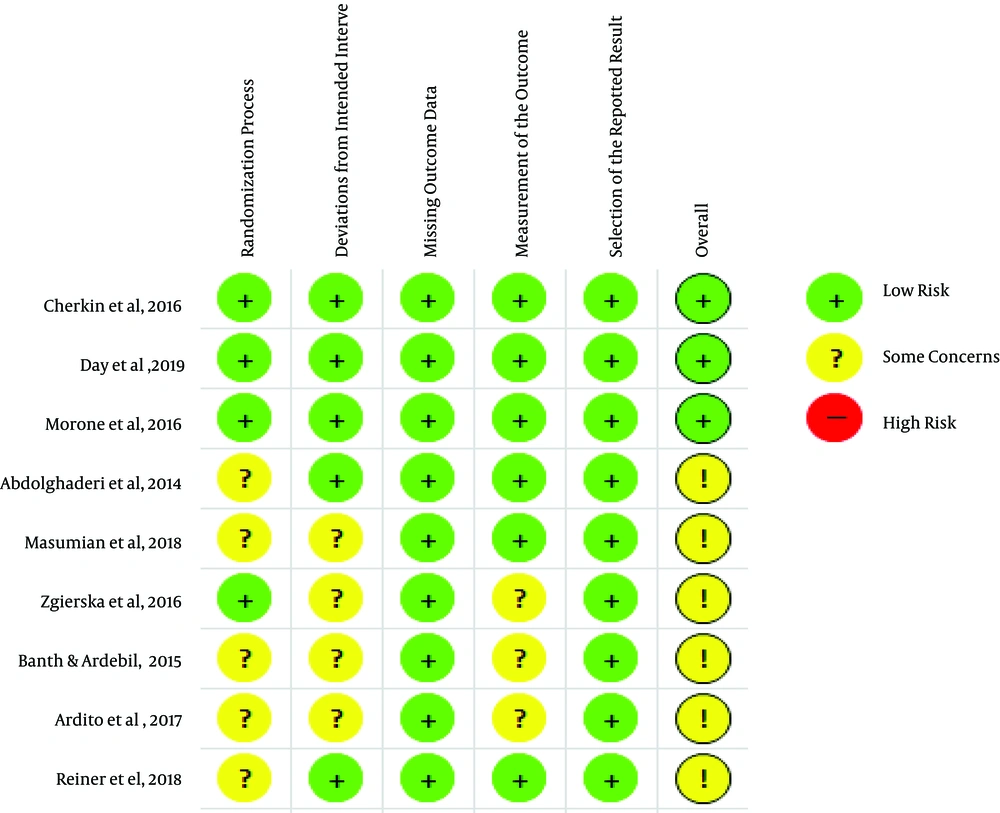
5.1. Assessment of the Risk of Bias
Two reviewers independently evaluated the risk of bias based on the Cochrane risk-of-bias tool for randomized trials (RoB 2) in terms of the randomization process, deviations from the intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result. Discrepancies between the reviewers were resolved by consensus of the third reviewer (H.H.).
6. Results
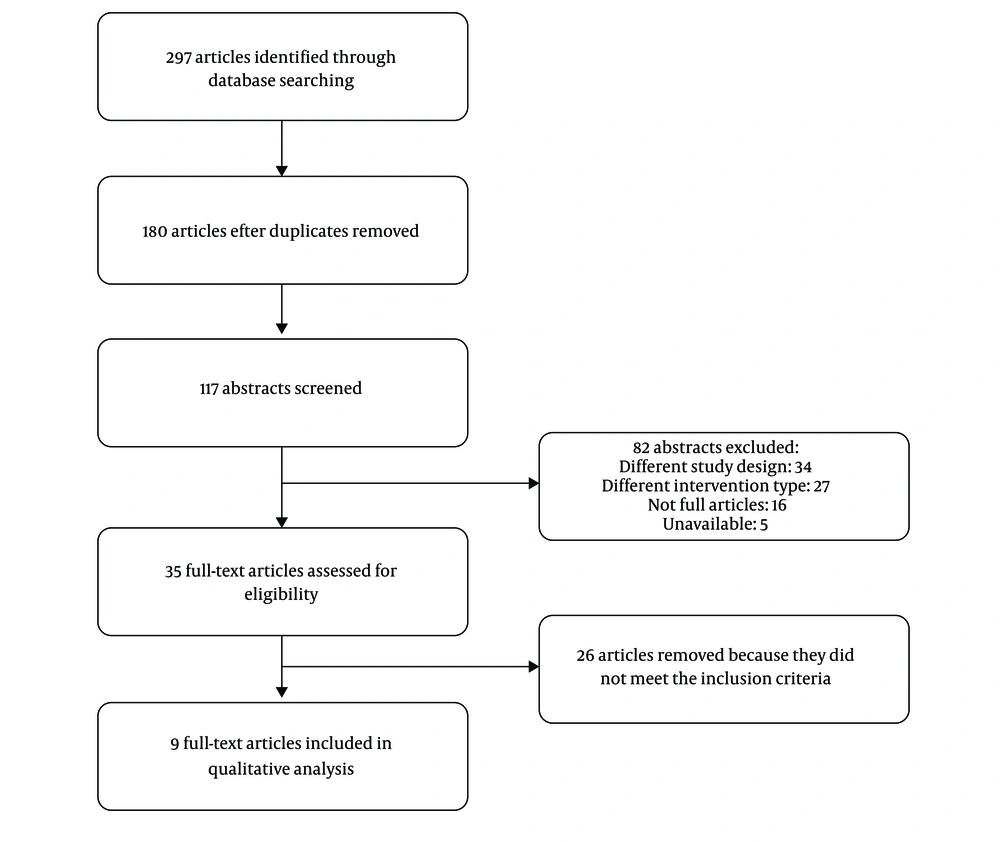
A total of 297 relevant articles were retrieved by the initial search, among which 262 duplicate and irrelevant articles were deleted after reviewing their titles and abstracts. After full-text evaluation, 26 studies were excluded due to the lack of inclusion criteria mentioned in the methodology. Eventually, nine articles with a total of 959 patients were included in this systematic review (Figure 1).
The characteristics of the nine studies are shown in Tables 1 and 2. In this study, patients with CLBP ranged between 20 and 70 years of age, but one RCT enrolled patients older than 65 years (17), and another enrolled 20 - 80 years old (18). In RCTs, the duration of pain was reported from three months or more (17-22), six months or more (23), and in two RCT is not mentioned (24, 25). They were referred either through physicians in rehabilitation centers, adult pain clinics, and physiotherapy centers (18, 20, 21, 23, 25), or they have introduced themselves after having been informed through a variety of media such as newspaper ads, direct mail (such as letters, brochures, Emails), or phone calls (17, 19, 20, 22).
| Authors/Year | Participants (Groups) | Mean (SD) Age, y | Inclusion Criteria | Mindfulness Intervention | Treatment Group (Intervention Length, Frequency, Duration) |
|---|---|---|---|---|---|
| Banth and Ardebil, 2015 (23) | 88 (2) | Overall: 40.3 (8.2) | Age 30 - 45 years, being under medical treatments, history of non-specific low back pain persisting pain for ≥ 6 months, language-Persian, gender-female, educated at least up to high school. | MBSR | MBSR, an 8-week program, one session per week for 90min; Homework: 30 - 45 min daily |
| Cherkin et al., 2016 (19) | 342 (3) | UC: 48.9 (12.5); MBSR: 50.0 (11.9); CBT: 49.1 (12.6) | 20 to 70 years of age, with non-specific low back pain that persisted for ≥ 3 months, rated pain bothersomeness ≥ 4 on 0- to 10-point scales, pain interference with activities ≥ 3 on 0- to 10-point scales | MBSR | MBSR, an 8-week program, once weekly for 2 hours plus optional 6 hours retreat. homework: frequency and duration not mentioned |
| Zgierska et al., 2016 (22) | 35 (2) | Overall: 51.8 (9.7) | Age ≥ 21 years, fluent in English, daily CLBP for ≥ 3 months, daily opioid therapy (at least 30 mg/day of MED), and ability to feel thermal sensations in both hands | Mindfulness meditation-CBT intervention | Meditation-CBT intervention, 2 hours per week for 8 weeks; homework: at least 6 days per week for at least 30 minutes per day |
| Morone et al., 2016 (17) | 282 (2) | MBSR: 75 (7.2); GC: 74 (6.0) | Age ≥ 65 years, spoke English, Mini-Mental State Examination score ≥ 24, RMDQ ≥ 11, CLBP (with moderate intensity for ≥ 3 months, occurring daily or almost every day) | MBSR | MBSR, an 8-week program, one session per week for 90 min, after intervention monthly 60-minute booster sessions, homework: daily meditation (six of seven days/week) lasting 50 minutes (45 minutes of meditation, 5 minutes to complete a log) |
| Ardito et al., 2017 (21) | 28 (2) | Overall: 48.14 (11.09) | 20 to 65 years of age, CLBP for ≥ 3 months, etiology of the pain: lumbago, sciatica due to displacement of the intervertebral disc, neuralgia, neuritis, radiculitis due to displacement or rupture of the lumbar intervertebral disc, lumbosacral spondylosis without myelopathy or fibromyalgia | MBSR | MBSR, 8 weekly sessions of 2 hours and during the second-to-last weekend a 7-hour session; homework: 40 min a day |
| Masumian et al., 2018 (24) | 18 (2) | MBSR: 44.33 (10.22); CG: 51 (3.42) | 18 to 60 years of age | MBSR | MBSR, one day a week during 2 - 2.5 hours in 8 sessions; homework: frequency and duration not mentioned |
| Day et al., 2019 (20) | 69 (3) | MM: 48.09 (16.13); MBCT: 49.87 (11.89); CT: 54.26 (14.87) | Age ≥ 18 years, a primary problem of CLBP (pain lasting for ≥ 3 months, experienced on ≥ 50% of days), average pain intensity of ≥ 4 for most days of the previous three months, analgesic or psychotropic medications have been stabilized for four or more weeks before study enrollment, fluent in English, able to attend a weekly two-hour therapy. | MM, MBCT | MM, MBCT intervention, 8 weekly 2-hour sessions, Homework: 45 minutes, six days per week. |
| Abdolghadery et al., 2014 (25) | 30 (3) | CLBP was diagnosed by a specialist physician, ages 18 to 60 years, upper secondary education, and No substance abuse. | MBCT | MBCT, each week for a 90-minute session for 8 weeks; homework: frequency and duration not mentioned | |
| Reiner et al., 2018 (18) | 67 (2) | CLBP for ≥ 3 months, pain level score of ≥ 5 | MBI | Inspired by MBSR and MBCT, each week for a 90-minute session for 8 weeks; homework: practice daily for at least 20 min |
Abbreviations: CBT, cognitive behavioral therapy; MBSR, mindfulness-based stress reduction; MM, mindfulness meditation; SD, standard deviation.
| Comparison Group (Intervention Length, Frequency, Duration) | Longest Follow-Up | Pain Intensity Measures | Results on Pain Intensity |
|---|---|---|---|
| Usual care only | One month | McGill Pain questionnaire | Significant differences for MBSR vs. UC in short- and long-term |
| 1) CBT techniques most commonly applied and studied for chronic low back pain, an 8-week program, once weekly for 2 hours. Homework: Frequency and duration not mentioned; 2) Usual care only | 26 and 52 weeks | Average of 3 ratings (current, worst, and average back pain in the previous month) rated on an 11-point Numerical Rating scale. | Significant differences; for MBSR vs. UC in; short- and long-term, no significant; differences for MBSR; vs. CBT |
| Usual care only | 26 weeks | Average of four-item subscale from the Brief Pain Inventory: “current” and past-week “average, worst and least” pain intensity, rated on an 11-point Numerical Rating scale. | Significant differences for meditation-CBT intervention vs. UC in short- and long-term (P = 0.045) |
| Eight weekly 90-minute health education program based on the “10 keys” to healthy aging, after intervention monthly 60-minute booster sessions; homework: frequency and duration not mentioned | Six months | present, average, and most severe during the past week by self-report with the Numeric Pain Rating scale (NRS; range, 0 - 20) | Significant differences for MBSR vs. health education program in long-term current and most severe pain intensity in the past week. |
| Usual care only | 4 - 5 months | The Numeric Rating scale (NRS), scale from 0 (“no pain at all”) to 100 (“my pain is as bad as it could possibly be”). | Significant differences were observed for MBSR vs. UC in short- and long-term |
| Usual care only | 0 | Multidimensional pain inventory (MPI) | Significant differences for MBSR vs. UC in terms of these subscales (daily activity disorder, pain intensity, and control over life) [P < 0.05], but not any difference between groups in terms of social support and emotional distress subscales [P > 0.05] |
| 1) Eight weekly 2 hours CT sessions homework: 45-minute, six days per week. 2) Eight weekly 2 hours of MM sessions; Homework: 45 minutes, six days per week. | Three months and 6 months | Average of four pain intensity items: most severe pain, least severe pain, average pain over the past week, and current pain rated on an 11-point Numerical Rating Scale. | Significant differences for post- vs. pre-treatment in MBCT, MM, CT groups in short- and long-term, with no significant differences between groups. |
| 1) Eight weekly 90 minutes CBT sessions; 2) usual care | 0 | McGill Pain questionnaire | Significant differences; for MBCT vs. UC in; short-term, No significant; differences for MBSR; vs. CBT. |
| Usual care only | Three months | Brief pain inventory, thermal sensory analyzer, warm sensation threshold and heat pain threshold, supra threshold pain | According to brief pain inventory, significant differences were observed for MBI vs. UC. |
In intervention groups, the type of MBIs is not the same in different studies; among them, mindfulness-based stress reduction (MBSR) (17, 19, 21, 23, 24), combined Mindfulness-Based Stress Reduction and CBT (MBSR/CBT) (22), Mindfulness-Based cognitive Therapy (MBCT) (20, 25), Mindfulness Meditation (20), and combined MBIs (MBSR/MBCT) (18) were used in intervention groups. MBIs were conducted in eight weeks and consisted of one 2-2.5-hour session per week, except for four RCTs, which held MBIs at one 90-minute session per week (17, 18, 23, 25). Almost half of each session was devoted to mindfulness meditation (body scanning, sitting meditation, and walking meditation) and the other half to training and conversation. All studies in their intervention groups required homework. In most of the studies, homework involved 30 - 45 minutes of meditation for 6 days a week (17, 20-23), except for one RCT, which involved 20 minutes of meditation for practice daily (18). In the rest of the studies, its period and frequency were not mentioned.
Different pain measurement tools have been used in different studies: McGill Pain questionnaire (23, 25), Numeric Rating scale (NRS) (17, 19-21), brief pain inventory (18, 22), and multidimensional pain inventory (MPI) (24).
In the first trial, 342 patients with CLBP in MBSR, CBT, and usual care groups were compared. Patients in the MBSR group showed a significant improvement in low back pain at 26 weeks compared to the usual care group (mean deviation (MD), -0.64 [confidence interval (CI), -1.18 to -0.11]) and this improvement was maintained at 52 weeks (MD, -0.85 [CI, -1.39 to -0.32]). In this trial, no notable differences were observed between MBSR and CBT (19). The second trial compared the effects of mindfulness meditation (MM), cognitive therapy (CT), and mindfulness-based cognitive therapy (MBCT) treatments on 69 patients who had been suffering from CLBP for an average of 14 years. Comparing post-treatment and pre-treatment for n = 43 (follow-up samples), meaningful improvements in pain intensity were illustrated in MBCT group (0.88 MD, [CI, 0.19 to 1.58]) and in MM group (MD, 0.41 [CI, -0.36 to 1.18]). This improvement was maintained at 3-month (MBCT (MD, 1.14 [CI, 0.38 to 1.89]), MM (MD, 0.48 [CI, -0.36 to 1.31])) and 6-month follow-up (MBCT (MD, 1.37 [CI, 0.67 to 2.07]), MM (MD, 0.81 [CI, 0.04 to 1.59])). No significant differences were found between the three treatment groups (20). In the third trial, the efficacy of MBSR was compared with the Health Education program in 282 patients with CLBP over the age of 65 years. The MBSR group showed a significant reduction in current and most severe pain for the past week during the 6-month follow-up. The changes in mean pain intensity were not significant (-0.1 [95% CI, -1.1 to 1.0] at 8 weeks and -1.1 [95% CI, -2.2 to -0.01] at 6 months) (17). In another trial with a small group of 28 patients with CLBP, the efficacy of MBSR on pain intensity, endocrine, and mental and physical functions were compared with the control group. The study showed moderate to high improvements in 4 - 5 months of follow-up in pain intensity and physical and psychological functioning (21). In a trial among patients with CLBP (n = 35) undergoing opioid treatment (at least 30 mg/day), the efficacy of CBT-mindfulness meditation intervention was compared with usual care. After 8 weeks of intervention (MD, 0.9 [CI 0.01 to 1.7] and 26 weeks (MD, 1.03 [CI 0.2 to 1.9]), significant differences in pain intensity between the control group and the experimental group were observed (22). In this trial, patients were categorized as either “consistent” meditators ( ≥ 150 minutes/week of formal meditation practice during at least 2/3 of the study) or “inconsistent” meditators (< 150 minutes/week of practice during at least 2/3 of the study). Compared to the control group, the consistent group showed a significant reduction in pain intensity at 26 weeks of follow-up, and the inconsistent group showed transient improvement at 8 weeks; but, these two groups (both in self-reported and in Biomarker measurements) were not significantly different between the consistent and inconsistent meditators at 8 and 26 weeks.
Another study compared 30 patients with CLBP in CBT, MBCT, and usual care groups. Sensory, emotional, and neuropathic pain intensity in CBT and MBSR groups showed a significant improvement compared to the control group, but no significant difference was found between CBT and MBCT (25). A small group of 18 patients with CLBP was compared in two groups of MBSR and usual care. In this trial, Multidimensional Pain Inventory (MPI) questionnaire was used to assess their pain intensity, which showed that MBSR improved pain intensity, daily activity disorder, and control over life subscales compared to usual care, but there was no significant difference in social support and emotional distress subscales (24). Finally, in a study, quantitative sensory pain testing (QST) measures of the thermal and pain thresholds, pain ratings to fixed stimuli, self-report measures of the chronic pain severity, and interference with daily activities were determined at baseline after 8 weeks. The MBI group indicated a decrease in ratings, while the control group indicated an increase (18). The overall risk of bias was “low” in three studies (17, 19, 20) and “some concerns” in other studies (Figures 2 and 3).
7. Discussion
This current systematic review is the only study that investigates the effectiveness of MBIs on CLBP in both English and Persian languages. The results showed that among patients with CLBP, MBIs compared to usual care significantly reduced pain intensity both statistically and clinically. Assessments also showed that MBIs reduced pain intensity as efficiently as CBT and there was no statistically significant difference between them. These results are consistent with the findings of a systematic review by Rainer et al., which reviewing controlled and uncontrolled trials, the effect of MBIs on pain intensity in patients with chronic pain is demonstrated (13).
Mind-body treatments such as MBSR and CBT are aimed at managing pain and equipping patients with effective long-term skills (19). By reviewing follow-up periods, we concluded that the efficacy of MBIs in reducing pain intensity was also maintained in a long period. A meta-analysis and systematic review showed in the short term, MBSR effectively reduces the pain intensity in patients with CLBP but failed to maintain this efficacy in the long term (26). The result shown in this study is different from the evidence in our study, which may be due to the small number of articles reviewed by this review study.
In most of the studies reviewed in this review article, pain intensity has been investigated as the primary outcome. It should be noted that reduction in pain intensity is not the primary focus of MBIs; in fact, these interventions reduce pain intensity indirectly by teaching patients to change their perspective about pain (27). Besides, it was shown (28) that the reduction in pain intensity associated with meditation is directly related to the part of the brain where the pain is diagnosed. This article states that mindfulness skills change the mental experience of pain.
Of the 8 studies reviewed, only one study examined the effectiveness of mindfulness in people over 65 years of age (17). The results showed that MBSR did not significantly affect average pain intensity. A systematic and meta-analysis review, investigating the effectiveness of various interventions on elderly people with non-specific CLBP, showed that complementary health approach (such as acupuncture, mindfulness, yoga, etc.) was not effective for pain intensity and disability in the elderly (29). Among the articles reviewed in this review study, there is only one article that uses mindfulness to treat elderly people with non-specific CLBP, so it can be said that evidence is limited to assess the effectiveness of mindfulness on older adults, and it needs further investigation.
In search of the Persian language, only one related article was extracted between the mentioned years in which the sample size was small and did not have a follow-up period. Therefore, it is recommended that more studies with larger sample sizes and longer duration of follow-up should be performed for evaluation of the effectiveness of MBI on the pain intensity in chronic low back pain.
8. Limitations
The limitations of the reviewed articles are the low sample size, higher education level, short follow-up courses, or sometimes no follow-up courses. The limitations of the present study are the heterogeneity of age and gender of participants, the tools of measuring pain intensity, and the type of intervention in the comparative group.
9. Conclusions
The results show that among patients with CLBP, MBI reduces pain intensity in short and long periods. It is also shown that the effectiveness of MBIs for pain intensity in CLBP is similar to CBT and is not significantly different.