1. Background
In 1948 the World Health Organization (WHO) defined health as “A state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity” (1). Although some authors do not agree on the inclusion of social well-being in health definition (2), according to the WHO definition, health is a complex term with a wide range of diverse conditions (3). Over the past two decades, much attention has been paid to the measurement of health, its improvement, and following-up on the outcomes of diseases (4). The index of quality of life (QOL) has been widely used as a measure of health outcomes (5). It could measure health outcomes beyond morbidity and biological dysfunction (2). WHO defines QOL as “The perception that an individual has of his or her place in life, within the context of the culture and system values in which he or she lives, and in relation to the objectives, expectations, standards, and concerns of this individual” (6, 7). QOL can include subjective or objective or both conditions affecting individuals’ existence; therefore, it is a broad concept (8). The term health-related quality of life (HRQOL); however, it focuses on the health domain of QOL with no incorporation of non-health factors of QOL, such as economic status or political circumstances (2). WHO defines HRQOL as “An integrative measure of physical and emotional well-being, level of independence, social relationships, and their relationship to salient features of their environment” (9, 10).
Although there is no single gold standard for health measurement (4), several generic HRQOL measurement tools have been used for this purpose, the Duke health profile (DHP) being one of them. Those tools can be used to determine the burden of disease and evaluate the outcomes of treatment in chronic diseases for the measurement of healthcare services and policy development (9). Since the generation of HRQOL measurement tools is a complex and time-consuming challenge in different social and cultural settings (11), translation, cross-cultural modification, and validation (5) of existing tools appear to be more reasonable.
Duke health profile (DHP) is a 17-item questionnaire that can either be self-reported or filled by interviewers (9). It also includes six health scales (physical, mental, social, general, perceptual, and self-confidence) and four dysfunction scales of anxiety, depression, pain, and disability (4). Items 8, 9, 10, 11, and 12 are assigned to physical health, items 1, 4, 5, 13, and 14 to mental health, and items 2, 6, 7, 15, and 16 to social health. The average of those three subscales is used as a determinant of general health. Item 3 is used to assess perceived health, and items 1, 2, 4, 6, and 7 are used to score self-esteem. Items 2, 5, 7, 10, 12, and 14 are used to determine the anxiety score. Items 4, 5, 10, 12, and 13 measure depression, item 11 measures pain, and item 17 determines the degree of disability. The DHP scores a range of 0 - 100 with higher scores, indicating better health conditions. Conversely, 100 is the worst, and zero is the best in case of dysfunction (9). Each item is answered by three Likert scales, including “yes, describes me exactly”, “somewhat describes me”, and “no, does not describe me at all”. In some items, the answers are presented as: “none”, “some”, and “a lot”. The last item’s answer is prepared as: “none”, “1 - 4 days”, and “5 - 7 days” (5). The score obtained from this questionnaire can be used as a health predictor. The questionnaire examines the health status of a person over the past week, and in older subjects, it is more suitable than the 36-Item Short-Form Health survey (SF-36 questionnaire) (9, 12). Up to 2011, the questionnaire had been translated into 17 different languages, including French, German, Italian, Afrikaans, Chinese, Dutch, Belgian, English, Portuguese, Spanish, Korean, Norwegian, Polish, Swedish, Taiwanese, and Vietnamese (9).
2. Objectives
There are approximately 110 million Persian speakers worldwide, justifying the need for a Persian-translated version of DHP. We, hereby, are reporting the process of translation of DHP into Persian language and its validation.
3. Methods
3.1. Translation of DHP
A forward and backward procedure was used to translate DHP from its English version to Persian. First, two bilingual experts with the instruction to focus on concepts rather than literal aspects of the text and that the audience would be the normal population, translated the questionnaire to Persian, separately. Then, the two translated questionnaires were merged by one of the authors, and an English to Persian translated questionnaire was obtained. In the next step, two other English professional translators who had not seen the original English questionnaire translated the Persian version again into English. Then, a panel of experts with educational background of psychiatry, clinical psychology, general practitioner, and health education, who were all bilingual, compared the original questionnaire with the Persian to English translated questionnaire, and eventually, after some linguistic and cultural adaptation, a basic Persian version was finalized. This version was tested in twenty people aged over 18 with different socioeconomic statuses in face-to-face interviews performed by the first author. After minor revision, the final version of the questionnaire was adopted.
3.2. Validation of the Questionnaire
Validation of the questionnaire was performed according to a cross-sectional study protocol. The study was carried out in Tehran, Iran, from August to September 2017. Participants in this study were volunteer individuals aged 18 and higher from two college students dormitories and visitors to three public parks who were recruited by convenience sampling. Based on previous studies (13, 14), the sample size was decided to be at least 10 times the questionnaire items. We, therefore, targeted a sample size of 240. Four trained interviewers initially introduced the objective of the study. In the case of subjects’ agreement to participate in the study, written informed consent was obtained, and finally, the questionnaire was completed in the presence of interviewers. Completing each questionnaire took up to 10 minutes. A total of 239 participants answered the questionnaire. The data were analyzed using SPSS and Lisrel.
3.3. Reliability
In order to determine the reliability of the questionnaire by test-retest, 35 college students were invited to complete the questionnaires in a two-week interval. Cronbach’s alpha coefficient was used to assess the internal consistency of the questionnaire. The alpha coefficient was separately measured for each subscale of the questionnaire, and values higher than 0.7 were considered satisfactory. To assess the questionnaire’s stability, the test-retest reliability was examined using the intraclass correlation coefficient (ICC) with ICCs of 0.4 and over were considered acceptable (15, 16).
3.4. Content Validity
A panel of nine experts evaluated the content validity of the questionnaire. Professions of the panelists included psychiatry, health education and promotion, psychology, and medical doctor with experience in public health and social medicine. The panel evaluated and scored the items of translated DHP for relevance, specificity, clarity, and simplicity on a Likert scale. The resultant content validity index (CVI) of 0.80 and over was considered acceptable (17). Furthermore, content validity ratio (CVR) was determined by the panel expressing their opinion about the necessity of each item on a three-point Likert scale with CVR of 0.78 and over was considered acceptable (18).
3.5. Face Validity
Twenty subjects from the general population with different ages and levels of education in both sexes were selected to assess the face validity of the items of the questionnaire. Each item was read for each member of the group. Their views on the ambiguity of the question and the problem in its perception and its relation to the purpose of the questionnaire were noted. This resulted in final amendments in the wordings of the questionnaire.
3.6. Construct Validity
A confirmatory factor analysis method was used to determine the construct validity. In this method, the χ2/df ratio was calculated. A ratio between 2:1 and 5:1 was re-quired for an acceptable fit (19). Also, the goodness of fit index (GFI), comparative fit index (CFI), Non-normed fit index (NNFI), normed fit index (NFI), root mean square error of approximation (RMSEA), and standardized root mean square residual (SRMR) were calculated. While CFI, GFI, NNFI, and NFI values may be between zero and one, a model valued 0.8 or higher was considered acceptable (15, 19). In fit models of RMSEA and SRMR, values less than 0.08 were considered acceptable (20).
4. Results
The descriptive characteristics of participants are shown in Table 1.
| Indicator | Values |
|---|---|
| Age, y | |
| 18 - 28 | 140 (58.6) |
| 29 - 38 | 62 (26) |
| 39 - 48 | 25 (10.4) |
| > 48 | 12 (5) |
| Sex | |
| Male | 137 (57.3) |
| Female | 102 (42.7) |
| Job Status | |
| Jobless | 84 (35.1) |
| Part-time | 75 (31.4) |
| Full-time | 79 (33.1) |
| Retired | 1 (0.4) |
| Education | |
| Not graduated from high school | 43 (18) |
| High school graduated | 56 (23.4) |
| Academic degree | 140 (58.6) |
| Marital status | |
| Married | 85 (35.6) |
| Single | 141 (59) |
| Divorced | 10 (4.2) |
| Widow(er) | 3 (1.3) |
| Physical illness | |
| Yes | 54 (22.6) |
| No | 185 (77.4) |
aValues are expressed as No. (%).
The overall Cronbach’s alpha index for the internal reliability of the questionnaire was 0.77 and between 0.47 and 0.69 for its subscales. The questionnaire subscales ICC was between 0.64 and 0.88. The questionnaire’s internal consistency and ICC are indicated in Table 2.
| Questionnaire Subscales | Cronbach's Alpha (95% CI) (N = 239) | ICC (95% CI) (N = 35) |
|---|---|---|
| Physical health | 0.69 | 0.88 (0.78 - 0.94) |
| Mental health | 0.59 | 0.75 (0.55 - 0.86) |
| Social health | 0.53 | 0.77 (0.60 - 0.88) |
| Perceived health | - | 0.68 (0.46 - 0.82) |
| Self-esteem | 0.47 | 0.87 (0.76 - 0.93) |
| Anxiety | 0.62 | 0.77 (0.59 - 0.87) |
| Depression | 0.62 | 0.82 (0.68 - 0.90) |
| Pain | - | 0.75 (0.56 - 0.86) |
| Disability | - | 0.64 (0.40 - 0.80) |
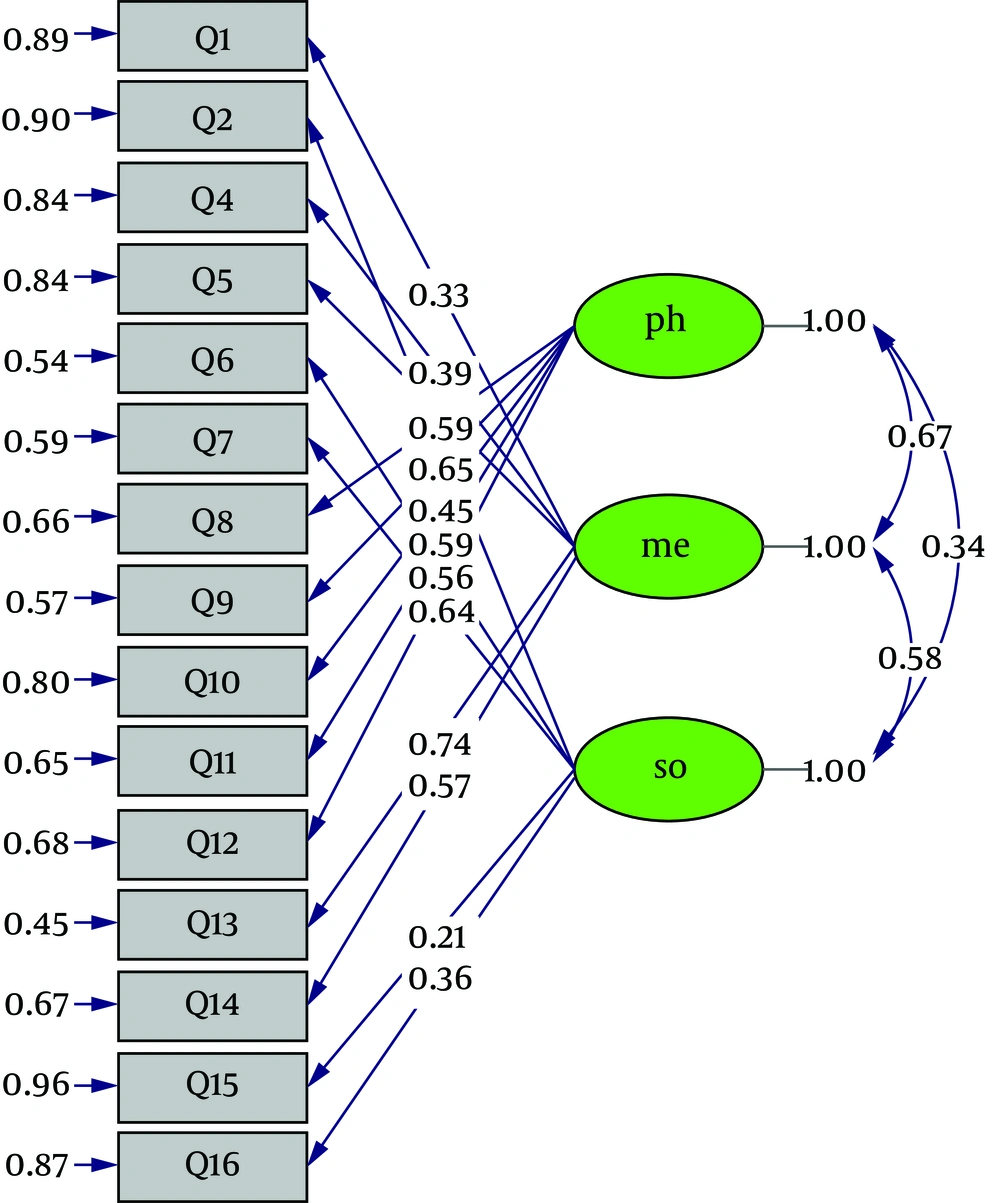
For each item, CVR was between 0.78 and 1, relevance CVI was between 88 and 100%, and S-CVI was estimated at 96%. Furthermore, clarity CVI for each item was between 88 and 100, and the clarity of S-CVI was 94%. Content validity indexes and qualitative face validity results were taken as proof that all items were valid. Construct validity was measured using confirmatory factor analysis (Figure 1). The original questionnaire covered six indicators of physical health (items 8, 9, 10, 11, and 12), mental health (items 1, 4, 5, 13, and 14), social health (items 2,6 ,7 , 15, and 16), self-esteem (items 1, 2, 4, 6, and 7), anxiety (items 2, 5, 7, 10, 12, and 14), and depression (items 4, 5, 10, 12, and 13). To determine fitness indexes, three subscales of physical health, mental health, and social health, as general health index, and subscales of self-esteem, anxiety, and depression were separately analyzed by first confirmatory factor analysis using Lisrel software (see Table 3). The fitness indexes, including χ2/df, RMSEA, SRMR, GFI, NNFI, NFI, and CFI were within good or acceptable range.
| Index | χ2/df | RMSEA | SRMR | GFI | NNFI | NFI | CFI |
|---|---|---|---|---|---|---|---|
| General health | 2.36 | 0.076 | 0.073 | 0.90 | 0.87 | 0.82 | 0.89 |
| self-esteem | 1.65 | 0.052 | 0.043 | 0.96 | 0.92 | 0.91 | 0.96 |
| Depression | 1.43 | 0.043 | 0.033 | 0.99 | 0.97 | 0.96 | 0.99 |
| Anxiety | 1.52 | 0.047 | 0.041 | 0.98 | 0.95 | 0.93 | 0.97 |
5. Discussion
The present study reports the process of translation of DHP to Persian language and further exploration of psychometric properties of the translated version. The original English version was translated into Persian, and adapted to this language by confirmatory factor analysis. Although a Persian version of WHOQOL and SF-36 are already available, DHP appears to be more convenient for the assessment of the quality of life.
Our study was able to demonstrate that all of the six subscales of the original version, i.e., physical health, mental health, social health, self-esteem, anxiety, and depression, were statistically valid and reliable in the Persian translation. Moreover, I-CVI and S-CVI indexes for relevance and clarity of items, as well as for the whole questionnaire, exceeded 88%, indicating good relevance and clarity of the items. Furthermore, the CVR index was between 0.78 and 1 for each item, which, according to Lawshe (21), indicating an acceptable content validity. The translated DHP Cronbach’s alpha index in this study was 0.77, and for specific subscales ranged from 0.47 to 0.69, indicating moderate reliability. The self-esteem subscale had the lowest value. The reliability index in the original study, however, was between 0.55 and 0.78 (4). This index has been reported to be less than or equal to 0.7 in other studies (9, 22, 23); nevertheless, in one study, it was equal to or higher than 0.87 for different subscales (5). Low alpha value can be a result of a small number of questions, low internal consistency, and weak structural heterogeneity. The more the items of a test are relevant, the higher the alpha coefficient. However, a high alpha coefficient does not always mean a high internal consistency of the tool because this coefficient is influenced by the length of the test. If the test is short, the alpha value reduces (24).
The ICC values in this study were between 64% and 88%, which were quite promising in terms of stability and reproducibility of the questionnaire. The ICC values in the present study, however, were higher than in other studies (5, 25, 26) and even values acquired in the original Duke version’s review (4).
For the assessment of the construct validity of Persian translated DHP, we tested CFA for four subscales. Fit index values, including χ2/df, RMSEA, SRMR, CFI, GFI, NNFI, and NFI, were all within the acceptable range. Physical health, mental health, and social health subscales were shown to be able to determine the general health index. Also, self-esteem and common psychiatric disorders such as anxiety and depression items were shown to be reliably measured. The convergent and discriminant validity of DHP by score correlations between DHP and sickness impact profile, Tennessee Self-Concept scale, and Zung Self-Rating Depression scale (4), or by assessment of the scores differences between substance user and non-user individuals and between single parent and non-single parent conditions of participants (5) has been measured previously. We, however, used confirmatory factor analysis for the assessment of the construct validity of the instrument.
5.1. Conclusions
The Persian translated version of DHP was able to qualify psychometric properties required for a questionnaire, including reliability, content validity, face validity, and construct validity.
5.2. Limitations
Regarding sampling, a selection bias could happen in convenience sampling. More than 70% of our sample was educated at the high school level or higher. This rate is somewhat higher than the general population literacy rate. Furthermore, our study does not prove that the Persian version of DHP will have the same results in cases with very lower education.