Dear Editor,
Coronavirus disease 2019 (COVID-19), referred to as 2019-nCoV and SARS-CoV2, has attracted global attention after appearing in Wuhan, China, in the late December 2019, followed by being introduced as a pandemic by the WHO (1). In recent months, measures taken to identify the destructive effects of this epidemic on public mental health have failed despite concentrations on epidemiology, clinical features, transmission patterns, and management of COVID-19 (2). Previous studies have suggested that pandemics impose a broad spectrum of psychological impacts. At the individual level, these adverse effects can cause new psychiatric symptoms, intensify the pre-existing mental illnesses, and induce distress in caregivers of infected patients. Accordingly, in such a condition, society members may undergo some negative experiences, such as fear and anxiety about falling sick or dying and helplessness, which can potentially cause mental breakdown (3). Likewise, it is believed that the COVID-19 pandemic can significantly affect public mental health and well-being in addition to physical health (4). From a psychopathological viewpoint, the current pandemic can be assumed as a relatively new form of stressor or trauma for several reasons. First, unlike natural disasters, the COVID-19 pandemic is not a temporary emergency limited to a specific region. In other words, this threat can exist in every region and be transmitted from person to person (2). Second, social isolation programs such as quarantine, physical distancing, and self-isolation may cause different psychological problems due to limiting normal adaptive coping strategies, namely social interactions, exercises, and leisure time. On the other hand, isolated infected patients cannot see their close ones, which intensifies their suffering (5). Third, some specific characteristics in COVID-19, such as uncertain incubation period of the virus, possibly asymptomatic transmission, a rapidly increasing number of confirmed cases and deaths, and lack of specific treatment or vaccine against the novel coronavirus, have escalated the fear and anxiety among the general population (1, 5). The final negative effect is the stigma of disease imposed on suspected cases, confirmed patients, and their families (even after being recovered) by society (1, 6). Therefore, the psychosocial consequences of the COVID-19 pandemic seem to be more severe for several groups of people and may put them in need of immediate follow-ups. These groups include (1) confirmed patients, (2) suspected cases, (3) susceptible persons, particularly those who are vulnerable to biopsychosocial stressors, (4) people who are directly or indirectly in contact with the virus, (5) patients who refuse to seek care, and (6) health professionals and healthcare workers (4).
According to the recent experiences, on January 26th, 2020, the National Health Commission of China released a statement about reducing the negative effects of COVID-19 pandemic on public mental health. The statement clearly emphasizes the importance of psychological crisis interventions as part of the public health response to the current pandemic (5). However, one of the drawbacks of this statement is disregarding the mobilization and coordination of different groups and the undeniable role of the government and society members in providing public mental health and well-being.
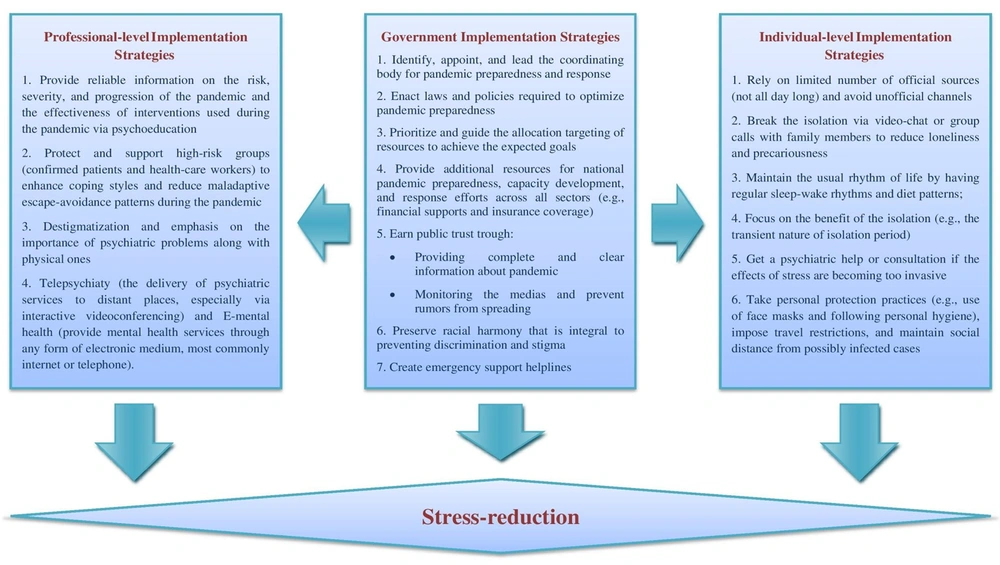
Accordingly, the proposed model of this paper classifies stress-reduction programs into three subcategories, including individual-level, government-level, and professional-level implementation strategies, and addresses the essential roles of these groups in the reduction of long-term psychological consequences of COVID-19 pandemic (Figure 1) (4-8). Based on this model, in the present condition, individual and professional unity, care-based and egalitarian policies, and the welfare provision role of governments constitute the only emergent and effective approach to overcoming the COVID-19 pandemic. Moreover, the evidence has suggested that the government has a major role in creating public trust and monitoring the proper execution of the strategies defined in the two other subcategories (7).