1. Background
Psychological disorders, as the most common group of mental disorders, involves high levels of anxiety, depression, and somatic symptoms (1). These disorders are extremely common and debilitating, resulting in significant cost and social burden on individuals, as they affect their personal, professional, and social performance (2). According to statistics, they affect a large proportion of the population in different societies (3). Generally, exposure to adverse life events is associated with life-long psychological trauma (4). A wide range of mental disorders, including cognitive, behavioral, emotional, and social problems, affect children and adolescents and continue into adulthood, causing various comorbidities in these individuals (3). These disorders can disrupt the lives of young people and their families and have significant impacts during adulthood.
The triple vulnerability theory for anxiety and depression claims that biological vulnerabilities, general psychological vulnerabilities, and specific psychological vulnerabilities play a role in creating and maintaining emotional disorders (5). Experience of emotional problems results in the person’s engagement in impulsive behaviors to boost his/her mood. Impulsivity, as maladaptive behaviors, are significantly associated with or caused by emotional disorders (6). The importance of impulsivity has been recognized in everyday life, given its effects on the decision-making process and many psychiatric conditions. Moreover, it is recognized as a diagnostic criterion for several personality disorders, such as borderline and antisocial personality disorders, eating disorders, attention-deficit/hyperactivity disorder, and substance or alcohol abuse (7).
Childhood abuse is a traumatic experience, associated with various types of abuse and neglect (physical, sexual, and emotional) (8). It leads to altered physiological responses to stressful stimuli, adversely affecting the future socialization of children (9). Childhood maltreatment experiences seem to be associated with impulsive behaviors, such as inappropriate affect, negativity, and reduced emotional adjustment. Evidence suggests that childhood abuse is a major threat to the person’s impulsive control system and leads to the development of antisocial behaviors (10). In other words, childhood abuse may be an environmental risk factor for the development of impulsivity in depressed adults (11).
Considering the clinical problems associated with high impulsivity, besides the relationship between Psychological disorders and childhood maltreatment, it is important to understand the mechanisms involved in the development of impulsivity and explore the relationship between these phenomena.
2. Objectives
This study aimed to determine the relationship between childhood maltreatment and emotional disorders, with impulsive behavior as a mediator, and to examine their causes and consequences.
3. Methods
The statistical population consisted of all second-semester students of Azarbaijan Shahid Madani University, Tabriz, Iran, in the academic year 2018-2019. According to the number of cases in Morgan table, a total of 316 students were selected via multistage cluster sampling. For this purpose, some classes were selected randomly from random university faculties. The questionnaires were distributed among the students after obtaining informed consent. The inclusion criterion were willingness to participate in the study and as age > 18 years and < 30 years, whereas the exclusion criterion were unwillingness to participate and incomplete questionnaires. In this study, the students were asked to complete the inventory of depression and anxiety symptoms (IDAS), the short form of Urgency-Premeditation-Perseverance-Sensation Seeking-Positive Urgency (UPPS-P) scale, and Childhood Trauma Questionnaire (CTQ).
3.1. Inventory of Depression and Anxiety Symptoms (IDAS)
IDAS was first designed to evaluate the specific symptom dimensions of major depression and anxiety disorders. It was developed by conducting principal factor analysis among three large samples (college students, psychiatric patients, and community adults). It contains ten specific symptom scales: suicidality, lassitude, insomnia, appetite loss, appetite gain, ill temper, well-being, panic, social anxiety, and traumatic intrusions. The scales are all rated on a five-point Likert scale (ranging from 1 = “never” to 5 = “too much”). Also, the scales are internally consistent and define a single underlying factor. Abdi et al. evaluated the factor structure and the psychometric properties of this scale in an Iranian population. They showed strong short-term stability, in addition to good convergent and discriminant validity with other measures of depression and anxiety (Cronbach’s α = 0.79-0.93) (12).
3.2. Urgency-Premeditation-Perseverance-Sensation Seeking-Positive Urgency (UPPS-P)
This scale was first developed by Whiteside and Lynam in 2001 by performing a factor analysis of self-report scales, measuring different aspects of impulsive personality, that is, perseverance, premeditation, negative urgency, and sensation seeking (lack of perseverance and premeditation). Later, a fifth dimension, called positive urgency, was added, based on a study by Cyder et al. (13). According to their study, although immediate action is marked by severe negative emotions in the model, there are also immediate actions under intense positive emotions that are not well thought out or measured. Therefore, they developed a positive urgency scale, which was incorporated in the impulsive behavior scale (UPPS-P). The items of this scale are all rated on a four-point Likert scale (ranging from 1 = “strongly agree” to 4 = “strongly disagree”). Jebraeili et al. evaluated the psychometric properties of this scale in an Iranian population in Tehran, Iran and reported an internal consistency reliability of 0.52-0.75 (14).
3.3. Childhood Trauma Questionnaire (CTQ)
This questionnaire, as a self-report tool for evaluating childhood abuse, was designed by Bernstein in 1994. In 1995, a second 53-item version of this questionnaire was developed, and its short form with 28 items (25 clinical questions and three validation questions) was finalized in 2003. Each item of the questionnaire is categorized into five levels (“never”, “rarely”, “sometimes”, “often”, and “always”) and is scored on a five-point Likert scale. This questionnaire assesses the extremity of emotional abuse, physical abuse, emotional neglect, physical neglect, and sexual abuse. It has been used in samples of psychiatric patients and substance users for psychological evaluation (15). The validity and reliability of this questionnaire are relatively high. In Iran, Garrusi and Nakhaee measured the reliability of various scales of this questionnaire in Iranian drug addicts, psychiatric patients, and college students and reported Cronbach’s alpha coefficients of 78-93% (16).
3.4. Data Analysis
All statistical analyses were performed in SPSS version 22 and LISREL version 8.80. Descriptive statistics, Pearson’s correlation coefficient, and structural equation modeling were used for data analysis.
4. Results
The study population consisted of university students, including 178 females and 138 males. The participants’ mean age was 23.4 years, with a standard deviation of 2.5 (range: 18 - 30 years). The means and standard deviations of the variables under study are presented in Table 1. The correlation matrix was calculated and examined for all variables, which are presented in Table 2.
| Index | Girls (178) | Boys (138) | Total (316) |
|---|---|---|---|
| Variables | Mean ± SD | Mean ± SD | Mean ± SD |
| Negative urgency | 2.952 ± 0.722 | 2.503 ± 0.902 | 2.576 ± 0.834 |
| Positive urgency | 3.252 ± 0.605 | 2.822 ± 0.786 | 3.064 ± 0.721 |
| Lack pf perseverance | 2.264 ± 0.718 | 2.588 ± 0.814 | 2.405 ± 0.777 |
| Lack of premeditation | 1.963 ± 0.818 | 2.458 ± 0.876 | 2.179 ± 0.878 |
| Sensation seeking | 3.199 ± 0.612 | 2.663 ± 0.810 | 2.965 ± 0.753 |
| Emotional abuse | 1.576 ± 0.749 | 2.137 ± 1.045 | 1.821 ± 0.932 |
| Physical abuse | 1.224 ± 0.415 | 1.730 ± 0.799 | 1.445 ± 0.662 |
| Sexual abuse | 1.328 ± 0.627 | 1.149 ± 0.351 | 1.250 ± 0.531 |
| Emotional neglect | 3.434 ± 1.035 | 2.843 ± 0.956 | 3.176 ± 1.043 |
| Physical neglect | 2.533 ± 0.363 | 2.589 ± 0.360 | 2.558 ± 0.362 |
| Lassitude | 1.879 ± 0.729 | 2.432 ± 0.963 | 2.120 ± 0.882 |
| Suicidality | 1.679 ± 0.772 | 1.948 ± 0.803 | 1.769 ± 0.796 |
| Insomnia | 1.438 ± 0.651 | 1.751 ± 0.792 | 1.574 ± 0.732 |
| Appetite loss | 1.646 ± 0.729 | 2.072 ± 0.985 | 1.832 ± 0.875 |
| Appetite gain | 1.642 ± 0.867 | 1.797 ± 0.876 | 1.709 ± 0.873 |
| Temper ill | 1.966 ± 0.872 | 2.521 ± 1.021 | 2.208 ± 0.978 |
| panic | 1.849 ± 0.801 | 2.420 ± 1.101 | 2.098 ± 0.984 |
| Social anxiety | 1.599 ± 0.746 | 1.844 ± 0.702 | 1.706 ± 0.736 |
| Traumatic intrusions | 1.865 ± 0.841 | 1.962 ± 0.697 | 1.907 ± 0.781 |
| Well-being | 1.769 ± 0.918 | 2.177 ± 1.032 | 1.947 ± 0.989 |
aValues are expressed as mean ± standard deviation (SD)
| variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total. impulsive behavior | 1 | |||||||||||
| Total. Childhood maltreatment | 0.449** | 1 | ||||||||||
| Lassitude | 0.45** | 0.564** | 1 | |||||||||
| Suicidality | 0.478** | 0.604** | 0.814** | 1 | ||||||||
| Insomnia | 0.373** | 0.517** | 0.757** | 0.79** | 1 | |||||||
| Appetite loss | 0.258** | 0.353** | 0.57** | 0.653** | 0.654** | 1 | ||||||
| Appetite gain | 0.291** | 0.308** | 0.498** | 0.447** | 0.367** | 0.158** | 1 | |||||
| Temper ill | 0.458** | 0.544** | 0.853** | 0.85** | 0.737** | 0.585** | 0.468** | 1 | ||||
| panic | 0.413** | 0.544** | 0.795** | 0.829** | 0.791** | 0.647** | 0.392** | 0.817** | 1 | |||
| Social anxiety | 0.261** | 0.416** | 0.669** | 0.658** | 0.718** | 0.622** | 0.351** | 0.647** | 0.752** | 1 | ||
| Traumatic intrusions | 0.442** | 0.606** | 0.825** | 0.819** | 0.747** | 0.618** | 0.436** | 0.651** | 0.816** | 0.668** | 1 | |
| Well-being | -.0334** | -.0423** | -.0729** | -0.678** | -.0622** | -.0461** | -.0.416** | -.0706** | -0.648** | -.0568** | -.679** | 1 |
a *P < 0.05; **P < 0.01
The impulsive participants reported higher levels of emotional disorder, including suicidality (r = 0.47, P < 0.01) and lassitude (r = 0.45, P < 0.01). They also reported higher levels of childhood maltreatment (r = 44, P < 0.01). Besides, there was a significant relationship between childhood maltreatment and emotional disorders, including traumatic intrusions and suicidality (r = 0.60, P < 0.01). For maximum likelihood estimation, descriptive statistics and Pearson’s correlation coefficient were calculated for all variables. Structural equation modeling was used to evaluate the hypothesized relationships between the variables. Also, the model fit was determined by measuring the root mean square error of approximation (RMSEA), comparative fit index (CFI), ratio of Chi-square to the degree of freedom (χ2/df), adjusted goodness-of-fit index (AGFI), goodness-of-fit index (GFI), and root mean square residual (RMR).
4.1. Structural Equation Modeling
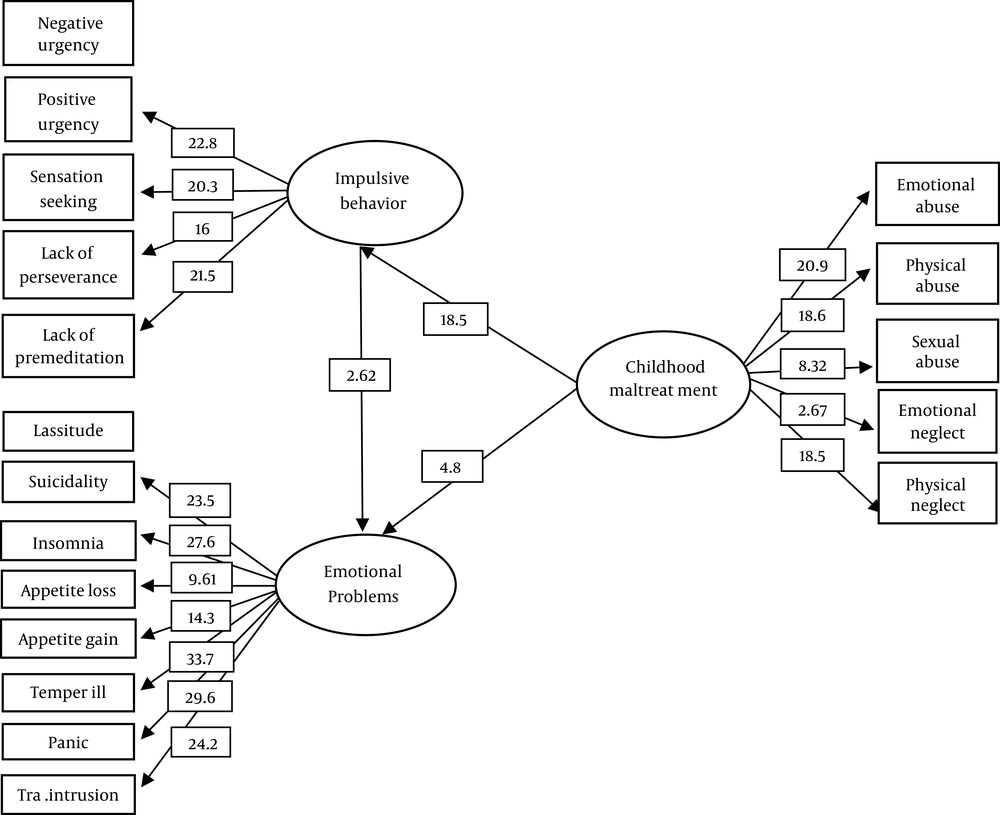
The structural model exhibited a generally good fit to the data (χ2 = 333.18, CFI = 0.99, GFI = 0.9, AGFI = 0.86, and RMSEA = 0.07) (Table 3). The results indicated that impulsive behavior mediated childhood maltreatment and emotional disorder dimensions (Figure 1).
| Index of Fit | RMR | RMSEA | AGFI | GFI | CFI | Χ2 /df | df | Χ2 |
|---|---|---|---|---|---|---|---|---|
| Indicator values | 0.021 | 0.070 | 0.86 | 0.90 | 0.99 | 2.52 | 132 | 333.18 |
5. Discussion
The results of the present study revealed a significant relationship between childhood maltreatment and impulsive behavior. This finding is in line with the results reported by Liu et al., Estevez et al., and Mirhashem et al. (8, 17, 18). Since children and adolescents are among the most vulnerable groups in the society, the risk of aggression and neglect of their needs can have long-term detrimental effects and lead to risky behaviors in the future.
There are several possibilities as to how childhood maltreatment can lead to impulsive behavior. The first possibility is the presence of an exchange relationship between the two phenomena. In other words, childhood maltreatment increases the risk of impulsivity and behavioral problems and consequently increases the likelihood of future emotional and physical abuse, especially when the parents themselves are prone to impulsivity. Also, this possibility is increased by the hereditary nature of impulsivity in children with impulsive parents. In other words, parents who have been exposed to wrong parenting practices and maltreatment are more likely to have impulsive children (8). Generally, in exposure to childhood maltreatment and abuse, the developing part of the brain is the most affected part, that is, the hippocampus from birth until the age of two years, the amygdala in early childhood, and the prefrontal cortex during adolescence. It is argued that poor development of the frontal cortex during adolescence, compared to other periods of development, is strongly correlated with the experience of abuse and impulsivity (8, 19).
The present study also revealed a significant relationship between childhood maltreatment and emotional disorders, which is in line with studies by Nelson et al., O’Mahen et al., Heleniak et al., Wanklyn et al., and Gaher et al. (20-24). Evidence shows that different types of abuse and maltreatment in childhood are associated with poor mental health outcomes, including increased severity of depression and anxiety (25). Also, children's living environment is especially important in the early stages of their development. Due to chronic exposure to stressful events, children’s neurological development can be disrupted, and as a result, their cognitive function or coping strategies may be impaired in the future (9).
In another study, it was concluded that all types of child abuse are associated with high levels of psychological problems and emotional reactions in the future (22). It has been also reported that childhood maltreatment plays an important role in causing depression, as negative attributions for the future are associated with childhood misbehavior and interfere with the person’s enjoyment of positive events (23). Moreover, studies have shown that people with a history of childhood maltreatment are highly vulnerable to the development of emotional failure and cannot effectively deal with negative emotional stimuli (24). Also, compared to sexual and physical abuse, the experience of emotional abuse in childhood is more significantly related to severe depression. The significant positive relationship between emotional abuse and depression has been reported in the literature (20).
Moreover, the present results indicated a significant relationship between emotional disorders and impulsive behavior, which is consistent with the results reported by Bellani et al. (26). It should be noted that impulsivity is associated with a wide range of personality traits, and there is a strong positive relationship between impulsive behavior and anxiety in impulse control disorders, such as gambling, eating disorders, and behavioral disorders. In other words, the risk of impulsivity increases in patients with mood and personality disorders (26).
Finally, the most important finding of this study was that impulsive behavior had an indirect mediating effect on the relationship between childhood maltreatment and emotional disorders. This finding is in line with the results reported by Oshri et al. and Schaffer et al. (27, 28). Oshri et al. concluded that impulsivity played a mediating role in the relationship between substance use and the experience of abuse and neglect. The negative urgency dimension of impulsive behavior seems to reinforce the relationship between childhood abuse and substance use. Childhood abuse influences the cognitive function and emotional desires of individuals, resulting in impulsive decision-making and subsequent drug use (27). Conversely, Schaffer et al. found that anxiety alone did not lead to suicide, while impulsivity accelerated suicidal thoughts, eliminated intrinsic restraints, and encouraged individuals to quickly select easy mechanisms to avoid stressful situations (28).
5.1. Conclusion
The present results confirmed our theoretical and empirical hypotheses. Sufficient evidence indicated the efficacy of our model for the interaction between child abuse, psychological distress, and impulsivity. In clinical practice, by relying on such findings, necessary measures can be taken to provide effective treatments and useful strategies for reducing these symptoms and increasing people’s awareness.
This study had some limitations. It only examined the students of Azarbaijan Shahid Madani University; therefore, generalization of the results to other individuals and age groups should be done with caution. It is also suggested that future research evaluate a wider geographical scope to provide coherent and consistent findings on the variables under study. Also, further research on other age and educational groups is recommended, as it this enables comparisons. Finally, according to the present results, educational workshops can be effective in raising the parents’ awareness and promoting proper parenting to overcome anger and impulsivity in children.