1. Background
Those working in health care settings are most likely to experience disruptive behaviors (DBs) due to stressful situations (1). One of the threatening factors to the organization’s ability to provide proper care is DB (2). DB is defined as any inappropriate behavior, conflict, confrontation, ranging from verbal abuse, like berating, yelling, intimidation, disrespectful, condescending, to physical or even sexual harassment that can adversely affect professional communication, working relationships, and data transmission at the end the process of patient care (3). DBs occur for a variety of reasons. A significant relationship has been reported between the physician’s and nurse’s DB and worrisome psychological and behavioral traits that lead to impaired working relationships, frustration, distraction, impaired communication, and a decrease in information transfer that adversely affect patient outcomes (4). According to Nakhaee and Nasiri (5), other factors influencing the physician-nurse relationship are unequal distribution of power, a negative public attitude toward them, ethical shortcomings, and wrong mentalities of the members of each profession.
DB is of great importance in health care centers due to its major complications. These behaviors in health care centers have a close relationship with a variety of errors due to miscommunication. In the most severe form, unprofessional behavior can destabilize patient’s care and affect the staff and workplace environment needs and as a common stressor leads to staff burnout and turnover (4, 6, 7). Rosenstein, in a study, pointed out a strong relationship between the physician’s DBs and the nurses’ dissatisfaction, low level of adherence to ethical principles, and an increase in turnover (3). Other significant negative effects of DBs include compromised patient safety or quality of care, dissatisfaction, major errors, such as patients’ unanticipated death or permanent disability (8). Due to the importance of the issue, there is a growing number of studies done on the causes, prevalence, and effects of DBs. Rosenstein et al. reported in their studies that such behaviors are repeatedly done by many professionals in maternity and emergency wards, leading to a shortage of nurses, near misses, and adversely affect the team dynamism, communication efficacy, information transfer, and accountability, resulting in negative effects on care process. Factors that contribute to this ongoing problem include a history of tolerance, a complex hierarchic-based medical care system, different stakeholder motivations, and a general problem in addressing behavioral rather than clinical issues (9, 10).
Maddineshat et al. (11), in their study conducted in the emergency department in 2016, indicated that 81% of physicians and 52% of nurses had DB,s which negatively affected the communication and cooperation among the staff as well as the quality of care. Fallahi Khoshknab et al. (12) reported that 74.7% of the participants in Iran had experienced psychological violence as a form of DB. In a qualitative study by Sanagoo et al. (13) on the concept of workplace incivility among Iranian nurses, such behaviors occur to varying degrees and in different aspects in the nurses’ workplace. Another study in Iran assessed the perceived incivility in medical centers, which reflects the experience of incivility by nurses from various sources, especially from physicians and patients. This study was performed only among nurses and addressed the origin of incivility (7). Since DBs are common, measurable, and associated with safety culture and health care worker well-being (14), it seems that assessing the prevalence of DBs and related effects in different parts of health care settings requires more studies. The results of these studies not only can indicate the current situation but also can be used as a basis for broader, deeper, and qualitative studies by providing problem-solving strategies.
2. Objectives
The aim of the current study was to investigate the incidence of DBs among physicians and nurses in different wards and assess their impacts on health care.
3. Methods
This descriptive cross-sectional quantitative study was conducted after getting scientifically and ethically approval (code: 292227) from the “Research and Technology Committee” and Psychosomatic Research Center in Isfahan University of Medical Sciences from January 2017 to February 2018. A modified printed/electronic 25-item questionnaire was given to participants. The participants in this study were volunteer nurses, physicians, and other staff working in teaching health care centers as well as medical and paramedical students in 4 major hospitals affiliated to the Isfahan University of Medical Sciences, Iran. Information related to ones who were away from the workplace for more than a year, and questionnaires that were not filled out or incomplete were excluded. Information about the purpose of the study was collected using a modified questionnaire by the research team. For this purpose, based on the number of staff targeted in this study, 4000 electronic and printed questionnaires were sent and distributed. The web-based questionnaire address was sent to students and faculty members’ academic e-mails. If they answered “No” to the “Complete the paper version of the questionnaire”, they were able to respond electronically. In order to distribute the printed version, the researcher was present in different shifts in the medical wards of the studied hospitals, and the questionnaire was provided to all staff. Boxes were put in the places mentioned, and people were asked to put the filled questionnaires inside the box.
The questionnaire was developed according to other questionnaires in similar studies, and some modifications were made based on the cultural and treatment differences under the supervision of a group of faculty members working in Isfahan University of Medical Sciences (10, 11, 15). After preparing the primary draft of the questionnaire, the validation of its translation was approved by English experts. Then, the questionnaire was distributed for content validity appraisal to different experts, including faculty members of the critical care and psychiatric nursing departments in Isfahan Nursing and Midwifery School, as well as two senior psychiatric nursing practitioners and a psychiatrist. The questionnaire consisted of two parts. Demographic information of responders (gender, educational level, job, hospital, and workplace ward) was questioned in the first part. The second part contained questions on the frequency of physician, nurse and other personnel’s DB (6 items: the general atmosphere of the nurse/physician relationship and related open question; witnessing DB by physicians, nurses and others; incidence of DB in different wards; percentage of physicians, nurses and other personnel with DB; frequent occurrences of DBs by physicians, nurses, and others), its effects on patient care and safety, clinical and psychological outcomes (8 items: severity of DB; negative effects and severity of those effects on patients and care of DB, effects on staff psychologic factors of DB; unwanted clinical outcomes; being informed about the adverse events as a result of DB; occurrence of adverse event and its preventability, and the rules related to DB and the status of the handling the DBs in the center (5 items: existence of behavioral statute; existence of executive support for that statute; the effect of admonition on staff; status of reporting DBs and related barriers). The questionnaire consisted of questions with three types of responses: yes or no, Likert-type responses (based on a scale of 1 to 10, in which the score of 10 shows the strongest agreement or the most positive response), as well as an open-ended question. Test-retest reliability was used in the pilot study with 30 respondents, and Cronbach’s alpha was 0.959. Before completing the questionnaire, at the beginning of the questionnaire, an explanation about the purpose of the study and voluntary participation was explained. Next, a definition of DB was provided to prepare the participant to answer the questions. They were assured that their response would be without mentioning their names. The data were analyzed using SPSS (version 16, SPSS Inc., Chicago, IL, USA) by descriptive statistics, including frequency rating and percentage.
3.1. Ethical Considerations
The approval of the Research and Technology Committee at Isfahan University of Medical Sciences (permission number: 292272) was granted before the study. The aim of the study was explained to the participants before data gathering, and they were assured about confidentiality and anonymity of their information. They were assured that participation in this study is voluntary, and they can leave the study at any time.
4. Results
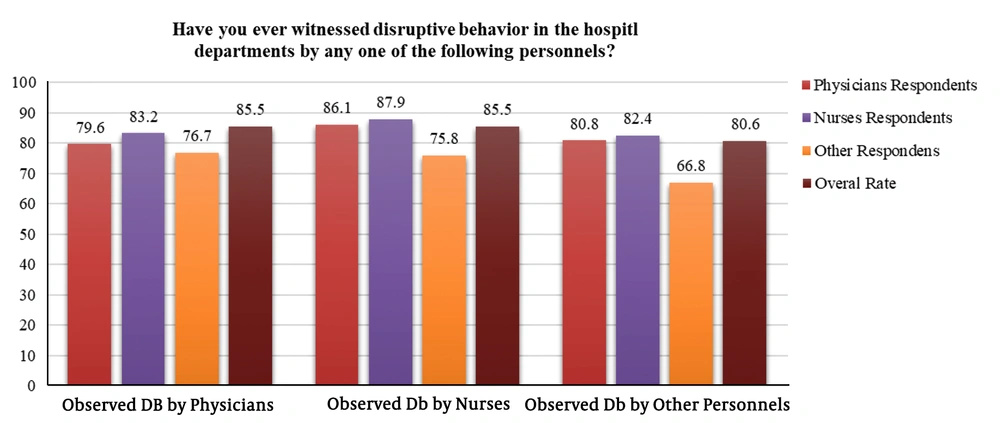
Fifty online questionnaires and 112 printed ones were excluded because the answers were incomplete or repeated. Finally, 248 questionnaires were completed by participants, including 133 nurses, 71 physicians, 11 office staff, 5 executive staff, 6 janitors, and 22 others, and they were collected. Most of the participants were working in the emergency ward (68 persons, 42.3%), and the least were from the recovery room (22 persons, 8.9%). DBs displayed by disciplines are illustrated in Figure 1. Those who had observed such behaviors done by physicians were 79.6% of physicians, 83.2% of nurses, and 76.7% of others. The most observed DBs by nurses were reported by 87.9% of nurses and 83.2% of the physicians. It was revealed that the highest prevalence of DB (85.5%) was performed by nurses and physicians.
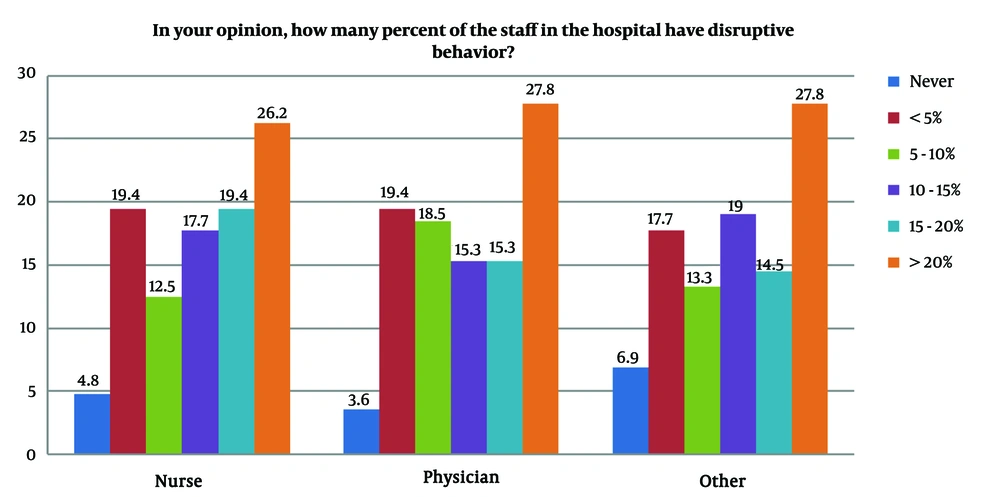
The results showed that the emergency department (56.9%) followed by the operation room (21.8%) had the highest incidence of DB. Outpatient clinics (20.16%) and maternity wards (20.4%) were in second place regarding the prevalence of DB. Other wards for the prevalence of DB included Intensive Care Unit (ICU) (18.95%), Cardiac Care Unit (CCU) (9.67%), recovery (8.87%), Laboratory (7.66%), and finally, Radiology Department (6.5%), respectively. Participants’ attitudes about the percentage of DB by hospital staff are shown in Figure 2. It can be observed that the highest percentage of DB done by physicians (27.8%), nurses (26.2%), and other staff (27.8%) included “more than 20%” item, while those who selected “no” in the questionnaire expressed the least prevalence in physicians (3.6%), nurses (4.8%), and other staff (6.9%). (Question: In your opinion, how many percent of the staff in the hospital have DB?)
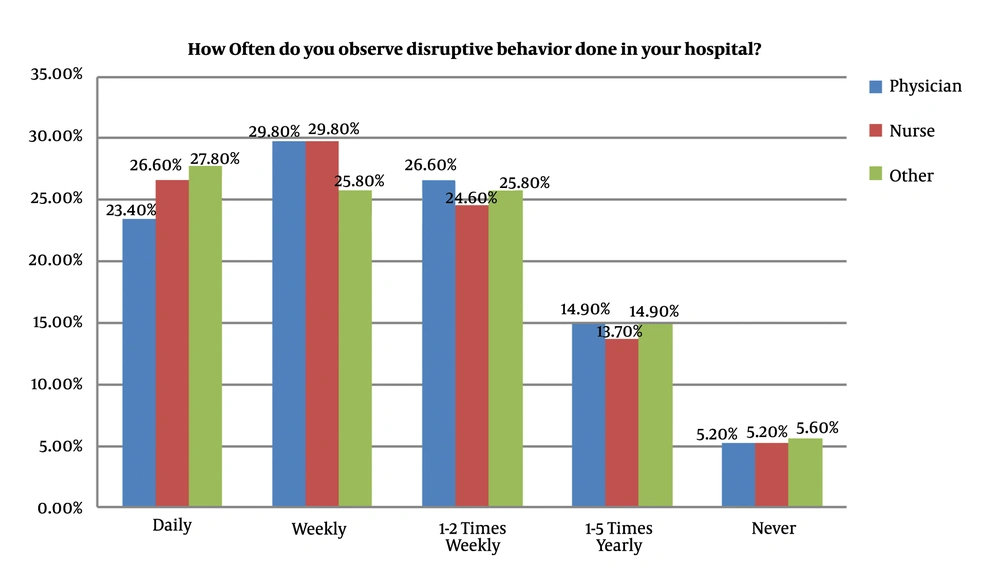
The frequency of DB done by the physicians, nurses, and other staff is illustrated in Figure 3. The weekly prevalence of DB had the highest frequency and it was 29.8% in physicians and nurses, and 25.8% among other staff. Daily prevalence shows the highest frequency of such behaviors occurs among other staff (27.8%), nurses (26.6%), and physicians (23.4%), in the second step. (Question: How often do you observe DB done in your hospital?)
Several questions were asked about the severity and negative effects on patients and the provided care and the linkage between these behaviors and undesirable behavioral factors and unwanted clinical outcomes in health care centers; the relevant information is summarized in Table 1. At the highest level, respondents believed that physicians, nurses, and others had “moderate levels” of DB. Regarding the negative effects of such behaviors, the highest score was related to “much” (101 cases, 40.7%) and the lowest went to “very little” with 9 (3.6%) cases. Participants stated that at the highest level (91.12%), DB leads to decreased concentration, and at the lowest level (81.85%), it leads to reduced information transfer, which is a high figure in its own right. Regarding the relationship between DB and unwanted clinical outcomes, respondents believed that, at the highest rate (87.50%), it leads to patient and nurse dissatisfaction, and at the lowest level (49.59%), it affects patient mortality.
| Physicians, No. (%) | Nurses, No. (%) | Others, No. (%) | |
|---|---|---|---|
| Severity of DB From the Respondents’ Point of View, Question: How Serious is Disruptive Behavior Issue in Your Hospitals? | |||
| Severity | |||
| Very much | 17 (6.9) | 18 (7.3) | 37 (14.9) |
| Much | 49 (19.8) | 43 (17.3) | 75 (30.2) |
| Moderate | 80 (32.3) | 91 (36.7) | 77 (31) |
| Little | 72 (29) | 67 (27) | 34 (13.7) |
| Insignificant | 30 (12.1) | 29 (11.7) | 25 (10.1) |
| Negative Effects on Patients and Their Cares of DB. Question: How Much Does DB Negatively Affect Patients and Their Care? | |||
| Values | |||
| Very much | 36 (14.5) | ||
| Much | 101 (40.7) | ||
| Moderate | 84 (33.9) | ||
| Little | 18 (7.3) | ||
| Very little | 9 (3.6) | ||
| Linkage Between DB and Undesirable Behavioral Factors. Question: How Much DB Influences Psychologic Factors of the Staff and Causing a Change in Their Performance? | |||
| Psychologic factors | |||
| Stress | 219 (88.30) | ||
| Frustration | 206 (83.06) | ||
| Decreased concentration | 226 (91.12) | ||
| Reduced N/P collaboration | 217 (87.50) | ||
| Reduced information transfer | 203 (81.85) | ||
| Reduced communication | 222 (89.51) | ||
| Impaired N/P relationship | 224 (90.32) | ||
| Relationship Between DB and Unwanted Clinical Outcomes. Question: Do You Think DBs Lead to the Following Unwanted Clinical Outcomes? | |||
| Unwanted clinical outcomes | |||
| Adverse events | 140 (56.45) | ||
| Medical error | 179 (72.17) | ||
| Reduced patients’ safety | 174 (70.16) | ||
| Reduced quality of care | 209 (84.27) | ||
| Patient mortality | 123 (49.59) | ||
| Nurse dissatisfaction | 217 (87.50) | ||
| Physician dissatisfaction | 209 (84.27) | ||
| Patient dissatisfaction | 217 (87.50) | ||
Abbreviations: DB, disruptive behavior; N/P, nurse/physician.
Fifty-two percent of the participants were informed about the adverse events as a result of DB, and 53.2% stated that they had observed such situations in their workplaces; 52% expressed that it could be prevented. Among the participants, 71% stated that there was no behavioral statute related to DB in their workplaces, and 89.1% expressed that even if there was a statute, there would be no executive support. The participants stated that the effect of admonition on physicians was 34.3% quite ineffective (high frequency) and 1.6% quite effective (low frequency) using a Likert scale of 1 (quite ineffective) to 10 (quite effective). The results of this scale for nurses showed that 43% had the highest frequency, and 2.4% had the lowest frequency. Among the participants, 61.3% stated that in their workplaces, they could not report such behaviors out of fear. There were some barriers to report DBs, such as fear of retaliation (65.3%), fear of no change in the situation (58.5%), confidentiality (51.6%), and finally lack of subsequent notice (33.1%).
5. Discussion
DB is one of the threatening factors in the quality of health care services that affects the relationship between the staff and has a considerable impact on the dynamicity of the health care team. Patient care is highly considerable, which is negatively influenced by DB, as well (10). The adverse effects due to such behaviors can impose a high burden on health care centers; as in a study in 2013, the combined costs for disruptive physician behaviors were over a million dollars (16). Although the unpleasant consequences are considerable, DB has a high prevalence. The present study revealed that 77% of physicians and 83% of nurses who participated in the study had witnessed DB performed by physicians, and 83% of physicians and 88% of nurses had witnessed such behaviors done by nurses; on the whole, 85.5% of the DBs were committed by nurses and physicians. This shows a high prevalence of DBs by physicians and nurses from the point of view of nurses and physicians. Rahder et al. (14) also pointed to the high prevalence of DB in their study, so that one or more of six DBs were reported by 97.8% of work settings.
In the present study, the prevalence of DB was assessed in 10 wards; the emergency ward with 56.9% was in the first place, followed by the operation room with 21.8% and the maternity ward with 20.4%. Similarly, in Rosenstein and Naylor study, 57% of participants witnessed the DBs by physicians, and 52% witnessed the DBs by nurses in the emergency department (10). In another study, it was revealed that in the emergency ward, the prevalence of DB was 81% for physicians and 52% for nurses (11). These findings indicate that the frequency and severity of DBs are more in stressful wards, such as the emergency ward, operation room, and maternity ward, in comparison with other wards (9, 10, 17). Several factors in the emergency department, such as the growing unscheduled and critical patient admission rate, the provision of care in a busy environment, and the presence of multiple care providers in the care process, can make several mistakes, which is a major contributor to the DBs in the emergency department.
The highest prevalence of DB was observed in physicians and nurses (over 20%) with a weekly frequency of 29.8% and a daily mean frequency of 25%. Similarly, Maddineshat et al. (11) concluded that the most weekly DB was committed by physicians and nurses. Respondents believed that the DB in the physician and nurse was moderately serious, but 87% of them believed that this type of behavior had a negative effect on the patient care and this negative effect on the patient and her/his treatment, has reported at a “high” (40.7%) level.
Regarding the psychological effects of DB, the respondents believed that the most negative effects were lack of staff concentration, impaired physician-nurse relationship, poor physician-nurse relationship, and stress, respectively. The least frequency was related to a decrease in information flow (81.85%), though it was high enough. In fact, the effects of DBs on psychological factors can affect the occupational performance of staff working in stressful workplaces. It is of great importance since, in such places, the job responsibilities and vital information should be appropriately and precisely shared among the multidisciplinary team during the patient’s care and treatment process. Similarly, Rosenstein and O’Daniel (15) found that DB in more than 90% of cases led to stress and disappointment as well as impaired physician-nurse communication, and in over 80% of cases led to the lack of concentration, less cooperation among team members, and imperfect information transfer.
Also, more than 80% of the respondents in the present study thought that DB had a negative effect on patient’s, nurse’s, and physician’s satisfaction and the quality of care. Moreover, more than 70% expressed that DB had a direct relationship with medical errors and endangered the patient’s safety. In a review by Oliveira et al. (4), DBs are a contributing factor in reducing the nurses’ and patients’ satisfaction, compromising patient care and safety, and increasing medical errors. Proper management of DB will be effective in reducing its incidence and consequences. In the present study, participants reported that the existence of behavioral statute and supporting such a statute was meager. They also mentioned that in one-third of the cases, the admonition to the physicians was quite ineffective, while it was more effective for nurses. Most of the participants thought that they could not report cases of DB out of fear, and half of them reported that they did not do it because of fear of retaliation, fear of no change in the condition as well as confidentiality. The findings of this study and other studies indicate a high prevalence of DB and its negative effects. Control and management of the DB are of great importance because it deteriorates the professional relationship and teamwork, while these two are crucial to improve the treatment outcomes and prevent undesirable events.
One of the limitations of this study, which was not addressed and required further and comprehensive study, is the investigation of different types of DB and their causes. Achieving such information will be necessary for more precise planning to manage DB in health care centers considering the different environments, cultures, and working conditions. In addition, another limitation of the present study was that the results could not be generalized to the other populations.
5.1. Conclusions
DBs in health care centers, especially in the wards with a high level of stress, are highly prevalent. Also, such behaviors have many psychological and functional consequences on health care staff and have destructive effects on the patient care process. It is important to have standards for professional behavior, related policies and procedures, a committee to evaluate and implement the standards, as well as to pay attention to and control stress in the workplace.