1. Background
Depression is a prevalent disorder. Its lifetime prevalence is between 4.4% to 20% in the general population. Kessler et al. estimated the economic cost of lack of productivity due to depression in America as more than 36 billion dollars (1). A large burden of damages caused by depression is probably related to treatment resistant depression (TRD). Several reasons could be suggested for this claim. First, considering response therapy as a criterion, 20% to 30% of patients do not respond to treatment and considering remission as a criterion, 50% to 60% of patients are not improved. Second, the duration and severity of disorder, which are both high in resistant depression, are important determinants of the burden of the disease. Third, resistant depressed patients are more likely to have simultaneous physical and mental disorders, which lead to obvious and continuing deficiencies in their performance and impose a lot of costs on the health system (2).
Resistance to treatment is the main concern in treatment of depressive disorders. Resistant-treatment depression is a term for describing the failure of therapy in a group of patients with MMD based on DSM-IV-TR or persistent depressive disorders in DSM-V after at least two trials of anti-depressive medications with enough doses and duration. The direct and indirect cost of resistant to treatment depression is higher than MDD patients, up to 40% to 50% (3).
Furthermore, STAR-D studies found that only 30% of MMD patients were improved in a trial attempt with antidepressant medication. The rate of remission for four successive trials was lower than this (4). From the psycho-social aspect, people with TRD have features, which make them prone to persistent depression. These people, compared with MMD, have more negative affect and dysfunctional cognitions (5). Teasdale proposed that perceived criticism strongly predicts depression recurrence and people with interpersonal problems experience severe and longer depressions (6).
However, fortunately, there are evidences, which imply that “Third Wave” therapy could be effective on chronic and recurrent depression and personality disorder. By weakening unhelpful verbal representations resulted from experiences and encouraging the patient to live at the present moment and promoting actions consistent with long term values, Act uses several methods for increasing psychological flexibility (7). The theory of ACT, primarily relates psychopathology to the lack of psychological flexibility, which is the result of experiential avoidance and problematic actions to control the inner experiences and fusion with thoughts and emotions. Psychological flexibility means the ability to contact moments of life and changing or stabilizing behavior. A behavior, which depends on a situation, is consistent with the values of the individual. In other words, ACT helps individuals have a more rewarding life, despite unpleasant thoughts, feelings, and emotions (8).
Another effective treatment for depression is behavioral activation. One of the models of behavioral activation, which was introduced by Lejuez et al. in 2001, is known as brief behavioral activation treatment for depression (BATD). The aim of BATD is to increase patient’s contact with healthy behavior, so that healthy behaviors are increased and depressed behaviors are decreased (9). The effectiveness of behavioral activation on patients with depression has been shown as compared to cognitive therapy and pharmacotherapy (10). Studies also reported the effectiveness of ACT compared to cognitive therapy (7) and other interventions (11).
2. Objectives
The current study investigated the effectiveness of ACT based on the fact that acceptance-based behavior therapies have been effective in patients with severe depression and TRD (7), and ACT among other acceptance-based behavior therapies (mindfulness- based cognitive therapy, dialectical behavior therapy) has received great attention in empirical studies and scientific debates (11) and its effectiveness on mood disorders has been indicated (8). Also, ACT was explored due to comorbidity in TRD patients (2) and that the ACT and behavioral activation due to their trans-diagnostic nature do not require distinguishing primary and secondary disorder, hence the evaluation and treatment of anxiety disorders and depression can be done in a better way. Furthermore, it is important to mention that there is no published source or conducted study either that has either distinctively or comparatively examined the effectiveness of ACT and BATD for TRD. Therefore, according to reviewing the existing research resources in Iran, the present study aimed at answering the following questions to optimize the treatment in patients with TRD using a case study: Is there any difference between the effectiveness of ACT and BATD in reducing symptom severity among patients with TRD? Is there any difference between the effectiveness of ACT and BATD in reducing rumination among these patients?
3. Materials and Methods
In this study, the method of multiple baseline was used (12). The samples, which were selected through accidental sampling consisted of all patients referring to two private psychiatric offices of Sari and a private consultant center of Babol (North of Iran). They were diagnosed with major depressive disorder and TRD based on a diagnostic interview conducted by a psychiatrist and referred to a clinical psychologist for conducting SCID-CV. The inclusion criteria included age of 18 to 60 years old, holding at least high.
School diploma, taking adequate doses of at least two anti- depressant drugs at least for 18 weeks without response to the treatment, scoring higher than 14 on BDI-II, and no change in the drug regiment from the past six weeks. Also, those, who had any of the following conditions were excluded from the present research: patients with psychotic spectrum, postpartum depression, substance abuse or substance dependence disorders, pervasive developmental disorders or intellectual disability, the presence of full criteria of personality disorders of cluster A, antisocial and borderline personality disorders of cluster B diagnosed by a psychiatrist based on diagnostic interview and clinical psychologist’s diagnosis according to the results of SCID-II(CV), co-occurrence of physical illnesses, which make attending the research difficult, receiving any psychological intervention in the past six months and the time of the study, and eventually the presence of self-harm and suicidal ideas.
Due the possibility of participants’ drop-out of the study, 12 patients were randomly selected after obtaining informed written consent, and then they were randomly divided to two groups of ACT and BATD. Two patients from the ACT group and three patients from the BATD group withdrew from the therapy during the baseline phase due to problems, such as far distance of their residence. In accordance with the principles of the single case study with non-concurrent multiple baseline design, selected samples were simultaneously entered in the baseline .They differed only in the number of the baseline phase. This means that patients in group one (patients one, two and five) had three baselines, patients in group two had five baselines (patients three and six), and patients in group three had seven baselines (patients four and seven).
Evaluating the effectiveness of ACT and BATD, the researcher employed the ACT and BATD protocol with 12 one-hour sessions developed by Zttel’s and Lejuez et al., respectively (the protocol content of two treatments is summarized in Table 1) (8, 9). Both therapies were conducted by a person, who was a PhD student in clinical psychology.
| Sessions | BATD | ACT |
|---|---|---|
| 1 | Introducing behavioral activation -explanation of depression / Introducing the rational of the treatment, daily monitoring and rating of enjoyment and importance. | Introduction to ACT-Verification of presenting problem-.Obtaining client’s life story-Identification of therapeutic goals and relationship to values. |
| 2 | Daily monitoring: Review of assignment and problem solving / Treatment rationale: review / Complete life areas, values. | To increase client awareness of emotional control-The introduction of willingness and acceptance as an alternatives to experiential control. |
| 3 | Daily monitoring and review assignment/ Life checklist in different domains, values and activities and review assignment / Activity selection and ranking. | The introduction of defusion method. |
| 4 | Daily monitoring and review assignment./ Daily monitoring with activity planning | Employing the defusion for self - evaluation and reason giving-The introduction of mindfulness. |
| 5 | Daily monitoring with activity planning: review assignment / Contracts / Daily monitoring with activity planning for the upcoming week. | Employing the defusion for life stories -The use of mindfulness in daily activities and self as context metaphor- clarify the values. |
| 6 | Daily monitoring with activity planning: review assignment / Contracts: review assessment / Daily monitoring with activity planning for the upcoming week. | To complete defusion from the life story-Breathing mindfully- To further promote a transcendent sense- To complete defusion from the life stories. |
| 7 | Daily monitoring with activity planning: review assignment / Life areas, values, and activities inventory: concept review and edit / Daily monitoring with activity planning for the upcoming. | The use of the mindfulness for thought and feeling To identify value-congruent goals / To initially instigate related committed action. |
| 8 | Daily monitoring with activity planning: review assignment / Activity selection and ranking: concept review and edit / Daily monitoring with activity planning for the upcoming week. | To determine the status of further mindfulness training / To clarify the nature of commitment / To further address ways of managing barriers to committed action and its promotion. |
| 9 - 11 | Daily monitoring with activity planning: review assignment / Contracts: Concept Review and Edit / Daily monitoring with activity planning for the upcoming week. | To promote the continuation of value-directed activities- To increase willingness to experience unwanted thoughts and feelings surrounding persistent committed action- To clarify distinction between the process and outcomes of committed action- To further promote mindfulness |
| 12 | Daily monitoring with activity planning: review assignment / Daily monitoring with activity planning for the upcoming week / Preparing for the end of treatment / Assignment: / Daily monitoring with activity planning: review assignment / Continue adding / editing contract. | To process the reaction of you and your client to treatment termination / To review ACT-consistent strategies and techniques / To promote the post-termination maintenance of therapeutic gains |
The Summary of Treatments Protocol Related to ACT and BATD
3.1. Measures
3.1.1. Structured Clinical Interview for DSM-IV to Assess the DSM-IV Axis I Disorders (SCID-I)
The SCID-I is a standardized and comprehensive tool, which facilitates the assessment process and also provides a reliable and valid clinical interview. The Kappa value (0.7) has been reported for most diagnoses. The Persian clinician version of the SCID-I has favorable reliability with kappa higher than 0.95 for one week (13).
3.1.2. Structured Clinical Interview for Axis II Disorders (SCID-II)
The SCID-II is a semi-structured diagnostic interview used to assess axis II personality disorders. The Kappa coefficient was found to be 0.53 (14). The content validity of the Persian version was confirmed by psychology professors and its test-retest reliability was reported as 0.87 for a one-week interval (15).
3.1.3. Beck’s Depression Inventory- II (BDI-II)
This inventory includes DSM-IV diagnostic criteria for depression and has shown good psychometric properties. The results have shown a high internal consistency (a = 0.92, 0.93 respectively) and a test-retest reliability (r = 0.93) was also reported. The BDI-II Persian version has demonstrated good internal consistency (a = 0.87) and acceptable reliability (r = 0.74) (16).
3.1.4. Ruminative Response Scale (RRS)
The RRS is a self-report scale with 22 items that assess the rumination and the tendency towards rumination as a response to depressive mood. The reliability coefficient of the scale varied from 0.88 to 0.92, using Cronbach’ alpha and the test-retest reliability was 0.67. Internal consistency of the Persian version was computed for the Iranian population and its Cronbach’s alpha coefficient was 0.88 (17).
4. Results
Characteristic features of the enrolled patients are shown in Table 2. Like most single-case designs, for analyzing the results of this study, several methods were used. One of these methods is standard of visual inspection, through which, changes observed in patients were investigated by assessment tools at different phases of baseline, during therapy, follow-up after six weeks by patterns of visual inspection of changes with BDI-II and RRS. Also, for calculating the reliability of statistical change, the RCI index was used. Results obtained from patients in target variables are shown on Tables 3 and 4, Figures 1 and 2. The Table 3 shows that, in the phase of baseline, the mean score of BDI-II in all patients was above 21. Except for the fourth and sixth patient, whose depression is in a moderate range, other patients’ depression was in the severe range before treatment.
| Patients | Age | Gender | Education | Job | Marital Status | Time Duration of Depression, Y | Psychiatric Comorbidity | Medical Backgrounds | Consuming Drugs at the Moment and Their Duration of Time |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 36 | Female | Electricity, B.Sc | Employee | Single | 6 | OCD- Narcissistic personality disorder | 2 times hospitalized, 2 phases ECT-Three times attempting to suicide | Citalopram 40- lamotrigine 200 bupropion 300- maprotiline 225- 7 month |
| 2 | 43 | Female | Diploma | Homemaker | Married | 18 | GAD- social phobia- avoidant personality disorder | Consuming of sertraline, buspirone, bupropion, clonazepam and ritalin- 4 times hospitalization- several times ECT | Sertraline 250- bupropion 300- clonazepam 1- 9 months |
| 3 | 40 | Female | Diploma | Homemaker | Married | 16 | GAD- panic disorder- dependent personality disorder | Various drugs such as sertraline, venlafaxine, buspirone, TCA- prazosin and aripiprazole in the last 2 years | Venlafaxine 200- buspirone 20- clonazepam 1 mg- 5 months |
| 4 | 37 | Male | Diploma | Worker | Married | 8 | OCPD | SSRI- SNRI- bupropion | Fluoxetine 40- bupropion 300- 4 months |
| 5 | 34 | Female | Diploma | Homemaker | Married | 13 | OCD | SSRI- SNRI- TCA- Bupropion | Sertraline 150, topiramate 150-propranolol 20 mg- 1 year |
| 6 | 30 | Female | B.Sc | Homemaker | Married | 4 | Dependent personality disorder | SSRI- SNRI- atypical antipsychotic | Venelafaxine 200- fluvoxamine300- 1 year |
| 7 | 33 | Female | Diploma | Homemaker | Married | 6 | GAD- avoidant personality disorder | SSRI- TCA- lithium-T3 | Sertraline 200- oxcarbazepine 50- clordiazpoxide 10 mg- 4 month |
Demographic and Clinical Characteristics of the Enrolled Patients
| Measures | Patients | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | Total %of Improvement | 5 | 6 | 7 | Total %of Improvement | |
| BDI-II | PT = 64, FU = 71 | PT = 34 FU =32 | |||||||
| BL | 35 | 33 | 30 | 21 | 35 | 26 | 32 | ||
| PT | 5 | 20 | 17 | 2 | 19 | 23 | 20 | ||
| %of improvement | 85 | 39 | 44 | 90 | 51 | 13 | 38 | ||
| FU | 3 | 18 | 15 | 0 | 18 | 25 | 20 | ||
| % of improvement | 91 | 46 | 50 | 100 | 53 | 5 | 38 | ||
| RCI | 8/96 | 6/60 | 6/84 | 8/80 | 7/52 | 3/23 | 8/70 | ||
| RRS | PT = 41, FU = 45 | PT = 17, FU = 21 | |||||||
| BL | 67 | 59 | 65 | 45 | 53 | 69 | 64 | ||
| PT | 31 | 46 | 32 | 36 | 45 | 59 | 51 | ||
| % of improvement | 53 | 26 | 59 | 28 | 16 | 15 | 21 | ||
| FU | 33 | 44 | 30 | 29 | 42 | 58 | 48 | ||
| % of improvement | 50 | 26 | 62 | 41 | 21 | 17 | 26 | ||
| RCI | 2/50 | 2/11 | 2/87 | 4/30 | 2/68 | 2/69 | 3/19 | ||
| Average improvement, % | PT = 52.5, FU = 58 | PT = 25.5, FU = 26.5 | |||||||
The Scores of Patients and the Rate of Improvement in the Target Variable at the Baseline and During the 45 Days of Follow- Up
| Group | Measures | No. | Pre-Treatment | Post-Treatment | Follow-Up | Effect Size Pre-Post, Hedges’g | Effect Size Pre-Follow, Hedges’g |
|---|---|---|---|---|---|---|---|
| ACT | BDi-II | 4 | 30.25 ± 6.1 | 11 ± 7.6 | 9 ± 7.6 | 2.42 | 2.68 |
| PRS | 4 | 63.5 ± 11.6 | 35.75 ± 3.4 | 34 ± 5.7 | 2.82 | 2.63 | |
| BATD | BDi-II | 3 | 32.66 ± 3.7 | 20.66 ± 1.7 | 21 ± 2.9 | 3.33 | 2.80 |
| PRS | 3 | 61.33 ± 8.1 | 51.66 ± 7.2 | 49.33 ± 6.6 | 1.00 | 1.29 |
Descriptive Statistics and Effect Sizes for Outcome Variables a Post-Treatment 45-Days Follow Upa
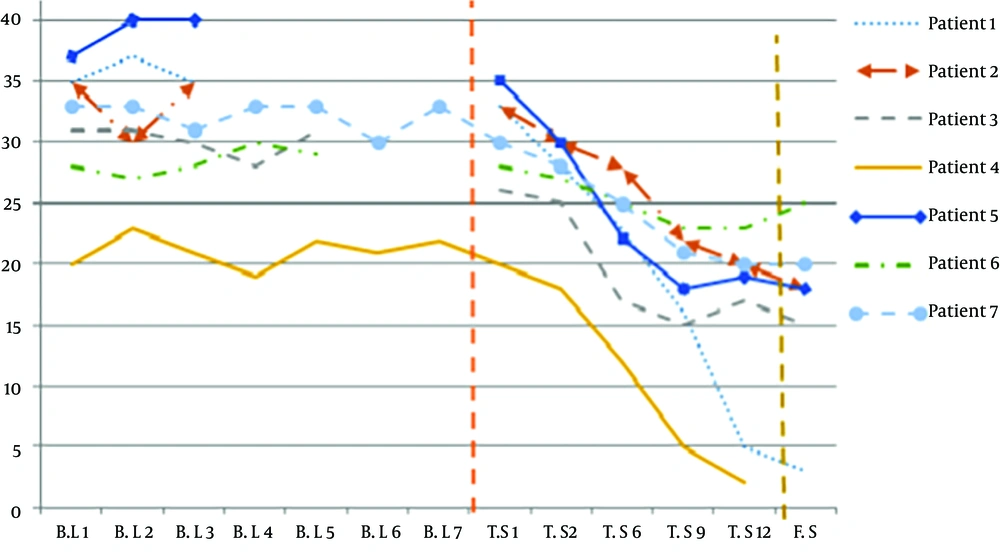
Observing Figure 1 indicates that the patients’ BDI-ll scores in ACT and BATD group in the absence of the psychological intervention was almost consistent. However, by changing the phase from base line to therapeutic intervention, particularly in the ACT group, a gentle and continuous slope was observed to the end of the treatment. At the end of therapy, patient’s BDI-II decreased to below 20% in the sixth patient. In the stage of follow-up, a greater decrease in BDI-II score in the ACT group was observed.
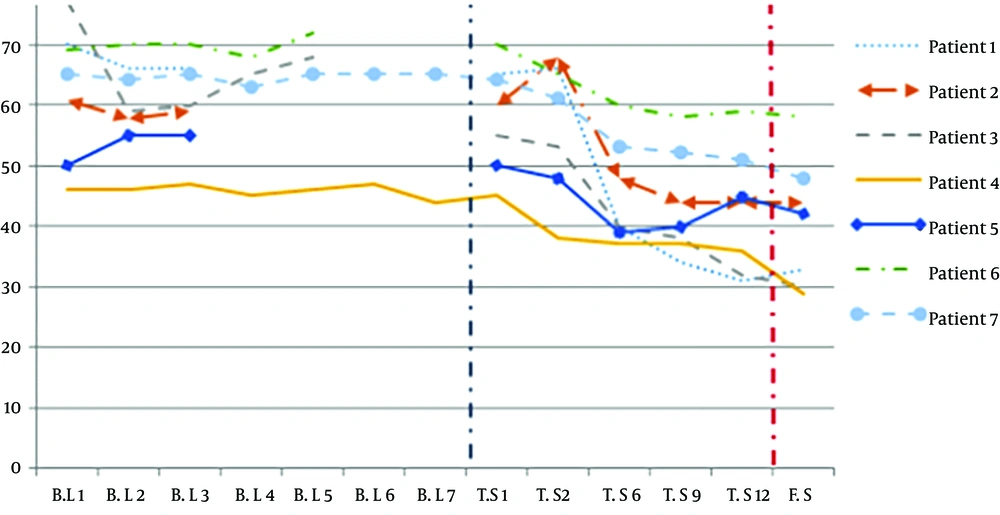
Also, what can be inferred from Figure 2 is a dramatic improvement of rumination scores in the ACT group compared with the behavioral activation group. The slope of this change started from the third session in the ACT group and except for the first patient, it continued to the end of the treatment and follow-up phase. The slope of change in the BATD group was slower and started from the sixth session onwards. Table 3 shows that after the treatment, patient’s rumination in ACT and BATD group had 41% and 17% improvement, respectively. In the follow-up phase, this improvement increased to 45% and 21%, respectively. According to the obtained RCI, which was above 1.96, in all patients in the follow-up phase, it can be concluded that therapeutic interventions increase the effect of pharmacotherapy in TRD patients (12).
As shown Table 3, the rate of improvement at the end of the treatment in ACT and BATD groups was 52.5 % and 25.5%, respectively. In the follow-up phase, this reached 58% and 26.5% in ACT and BATD groups, respectively. According to the amount of RCI, all patients’ target variables at the follow- up phase were above 1.96 compared to the baseline, which is an indication of statistical significance.
The patients’ RCI showed that these changes are not the result of unreliability of the tests and treatment could increase the patients’ improvement. Also, the success of therapies is different from each other, and ACT was superior to other therapies.
In this study, for calculating the effect size, Hedges was used. The effect size obtained from Hedges is interpreted similar to Cohen’s d (0.20 = small, 0.50 = medium, 0.80 = large). In Table 4, the average, standard deviation, and acceptable effect size of patients in two groups at different stage of study were observed. Here, greater reduction in the average of depression severity and rumination in post-treatment and follow-up phase were observed in the ACT group compared with the BATD group (18).
Independent evaluation at the end of follow-up phase was done by a psychiatrist. The rate of improvement in acceptance and commitment group and behavioral activation group was estimated as 72% and 43%, respectively. On the other hand, the fidelity of therapist to the therapeutic protocol was also approved.
5. Discussion
The first aim of this study was to determine the effectiveness of settle’s ACT protocol for depression (8) and BATD for depression (9) on add on pharmacotherapy in TRD and then make a comparison between these two treatment methods .The important finding of this study was that, as shown in the Table 3 and Figures 1 and 2, the target variables of all patients at the very beginning was above the cut of point. Regardless of the number of patients at baseline before treatment, despite at least seven to ten weeks of pharmacotherapy, the target variables were almost constant. This does not mean pharmacotherapy had no effectiveness, since there is no information about the variable scores of the patients at least in the first 18 weeks before the start of study. Therapeutic changes started with different speeds in both groups. The average rate of improvement in the two variables in the ACT and BATD were 52.5%, 25.5%, 58%, and 26.5% at the end of the treatment and in the follow-up phase, respectively. However, the severity of the depression in the second, third, fifth, and seventh patient in the follow-up phase was mild and in the sixth patient it was moderate.
The remarkable result is that the intensity of depression improved more during the follow-up phase rather than the end of the treatment in the ACT group, which is a common finding of studies related to the effectiveness of ACT (7). It should be noted that at the follow-up phase, one of the first patients reported that in early treatment, they completely stopped taking their medication and the second patient reduced the dosage of Sertraline to 50 mg a day. Also, effect size post-treatment in both groups was large and this power was maintained in the follow-up phase. Improvement in depression and rumination in the BATD group is consistent with other study findings. Although, the published literature regarding application of BATD and ACT in TRD is limited, the findings of the current study are to some extent consistent with Bottonari et al.’s findings. They treated a 62-year-old patient diagnosed with TRD. He had comorbid disorders, and also unsuccessful long background of pharmacotherapy, electric shock, and cognitive therapy (19). Also, Marial et al. reported that behavioral activation therapy leads to rumination reduction in patients under their therapy (20). Moreover, improvement in the BATD group was similar to Dobson et al.’s extended findings, which compared behavioral activation therapy with CBT and antidepressant medication. The findings of this study showed a significant improvement in depression and rumination (10).
Improvement in the BATD group and even the ACT group could have been due to a reduction in avoidance, which is consistent with the conceptualization of depression that has been proposed by these therapies (8-10). It was stated that behavioral activation tries to reverse the cycle between depression and avoidance through providing various sustainable sources of reinforcement (21). Behavioral activation states three basic premises, including activity of rewarding activity increases positive reinforcement, the positive reinforcement leads to a reduction in symptoms of depression, and the positive reinforcement is a mediator between the activity and depressive symptoms (22). The avoidance of the fifth and seventh patient, who showed a better improvement than the sixth patient in all indexes was supported by their environment, as is clear in the rumination index. The findings of this study is compatible with previous studies, which indicated that activation can lead to changes in beliefs and cognitions, which are essential elements in long term emotional and behavioral changes (22, 23). Kanter believed that changes in rumination are the direct result of activity increase (20). The usefulness of behavioral activation can be proposed by another explanation as well. Behavioral activation can create positive emotions, such as pride, honor, sharpness, etc. that can support individuals against negative life events and enhance their resistance to those events (24). Improvement in depression and rumination index in the ACT group is in accordance with Clark et al.’s findings, which investigated the efficacy of CBT and ACT in 45 treatment resistant patients, in which the results showed the priority of ACT in the follow-up phase (7). Also, the current findings is in accordance with Yovel et al.’s findings, which showed that the ACT method leads to a reduction in rumination (25). Even though ACT does not directly aim at reducing depression as a goal, the therapeutic elements, such as diffusion, value directed behaviors and mindfulness, all reduced depression in this study, indirectly. This finding is in accordance with other study findings (26, 27). Further improvement in the severity of depression at follow-up compared to post-treatment (71% versus 64%) is consisted with the results of other studies in the ACT field or other third wave therapies, which use mindfulness (7). In explanation of the results, it can be said that ACT considers depression and emotional problems as a result of experiential avoidance, which appears in case of lack of willingness to stay and having contact with private experiences and trying to get rid of this annoying experience ranging from negative emotions and painful memories. In the theory of ACT, experiential avoidance is the result of a verbal process like “depression is bad”, “I cannot endure these feelings”, and “I must always be happy”.
Experiential avoidance lead to psychological inflexibility and usually greater suffering. However, hexaflex processes, which are used in ACT, lead to reduction of avoidance and an increase of psychological flexibility. Also, it has been stated that depressed patients usually tend to find reasons for their depression and this leads to more rumination. By mindfulness and self as context methods, the kind of patient’s relationship with his or her emotions and thoughts will be changed (8). Twohing et al. proposed that techniques used in ACT, increase the acceptability of treatment among patients (28). Also, greater improvement in the follow-up phase is because of the fact that ACT does not merely seek symptom reduction, yet a meaningful living based on value will be targeted (7). Goldin and grass, assert that practice of mindfulness influences the brain mechanisms related to information processing. They stated that the techniques can lead to an increase of positive self-talk and a decrease of negative self-talk. This method creates greater activity in the brain network related to deployment of attention and reduction of linguistic-conceptual activity (29). The results of this study may be affected by non-specific factors, such as therapeutic alliance, so that, for example some of the patients like patient number four, had been motivated to report that he enjoyed the benefits of treatment. Although a 90-% improvement in symptoms of the disorder was reported for this patient that was done by psychiatrist in independent evaluation at the follow-up phase, it is recommended for future studies to examine the efficacy of trans-diagnostic approaches in comparison with non-active interventions, such as group support.
5.1. Conclusion
The results of this study provide greater evidence for ACT and BATD efficacy. Also, the present study supports the role of trans-diagnostic approaches as an add on to pharmacotherapy in TRD.
These treatments can help change the degree of improvement from treatment response to remission. They can also reduce disadvantage of mere pharmacotherapy and biological therapy, such as drugs’ side effects, which result in a decrease in quality of life and ultimately non-compliance (30). This fact is particularly applicable for BATD, as a cost effective treatment that does not need any long term training and can be conducted in different cultures (21).
5.2. Limitations
Although the findings of this study are preliminary and have some limitations, it has been shown that new approaches in psychotherapy may play an important role in strengthening the TRD treatment
One of the limitations of this study was the inadequate follow-up period. Also, another limitation was the single case design, including limited sample, which makes generalizability difficult.