1. Background
Oppositional defiant disorder is relatively new and used for people who do not have the diagnostic criteria for conduct disorders (1). Approximately one in 10 people will display oppositional defiant disorder (ODD) criteria throughout life (2). The disorder is characterized by a pattern of persistent anger, irritability, and stubborn and resentful behavior (3). One to 6% of children and adolescents have oppositional defiant disorder, which indicates that this disorder is most common in this period. However, the prevalence varies according to age, gender, and cultural and social context (4-6). The economic costs associated with oppositional defiant disorder are not limited to treatment costs, but the criminal behaviors go beyond the treatment of the disorder (5). Oppositional defiant disorder affects family members and the community (7-9). Therefore, early diagnosis and initiation of treatment can prevent economic, social, family, and personal harm. Genetic predisposition is influential in the onset and persistence of ODD, while the role of genetics is combined with environmental factors. One of the major difficulties in diagnosing this disorder is its combination with other disorders such as Attention Deficit Hyperactivity Disorder (ADHD). This study aimed to develop a tool for the early detection of children with ODD. Early detection of ODD is essential to initiating treatment intervention for at-risk children (4, 10).
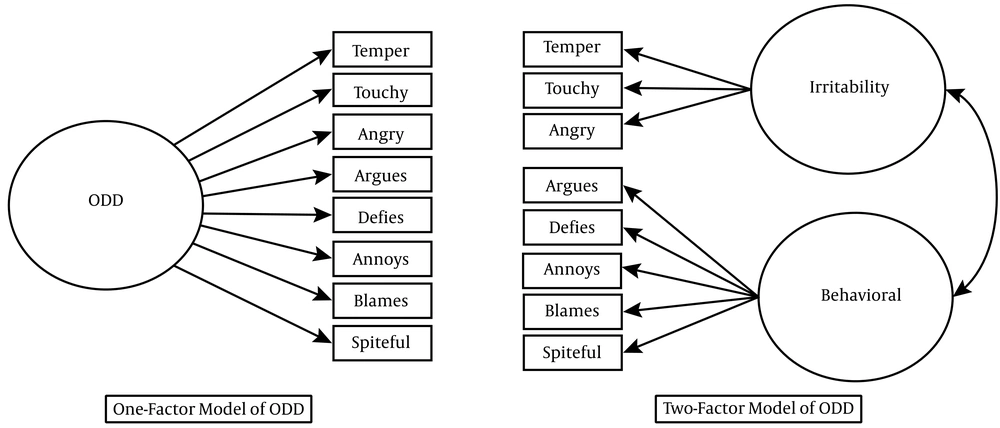
Different inventories have been developed to measure oppositional defiant disorder, the most important of which is the Achenbach Behavioral Problems Inventory, which has three versions of self-report, teacher report, and parent report, used for the age range of 11 to 18 years. Another inventory is the ODD rating scale of Hommersen, Murray, Ohan, and Johnston used for diagnosis of oppositional defiant disorder in the age range of 5 - 15 years (11). It has the teacher and parent forms. As the Achenbach Inventory is used for all behavioral disorders, a tool is needed that can specifically use to assess oppositional defiant disorder. Harada et al. developed an 18-item inventory that included only the parent-report version of it. In the present study, in cooperation with the developer of this inventory, we aimed to develop a cross-cultural adaptation self-report version of this inventory in Persian (12). Since the researcher's effort was to adjust the inventory with DSM 5, it was necessary to identify the dimensions that make up that concept. Research evidence has shown that oppositional defiant disorder is a multidimensional disorder, so it is useful in the clinical classification of disorders and research tools. Anger and irritable mood and deficit/arguing behavior are two distinctive aspects of this disorder in the Diagnostic & Statistic Manual of Mental Disorder Version 5 (DSM5). Although research models differ slightly in the number of factors, they are generally divided into two dimensions: Irritability, which is characterized by a relatively stable state of anger, and stubborn and destructive and resentful behavior (as a behavioral dimension), characterized by arguing, blaming, and harassing others (11, 12). The first dimension of irritability is a strong predictor of anxiety disorder and depression (13). The behavioral dimension of oppositional defiant disorder is the predictor of substance abuse, borderline personality disorder, violence, and criminal behavior. In a study by Johnston, Grossi, and Burke (13), a two-factor model (including irritability and behavioral factors), illustrated in Figure 1, described the oppositional defiant disorder.
One- and two-factor models of ODD symptoms adopted from article of Johnston, Grossi, and Burke (13)
Given the importance and necessity of having a tool for diagnosing oppositional defiant disorders that can be used in different groups of children and adolescents for research and clinical diagnosis goals, it is necessary to provide a tool in this regard. Hence, this study aimed to provide a cross-cultural adaptation form of the self-report version of Harada et al.’s Oppositional Defiant Behavior Inventory and assess its reliability and validity. Thus, given the aim of the study, this question is asked: Whether versions of oppositional defiant behavior inventory have sufficient reliability and validity. The structure identifying the psychometric properties of this tool in clinical and research areas and its applicability in normal and abnormal populations justify the importance and necessity of this research.
2. Objectives
This study aimed to provide a cross-cultural adaption form of self-report Oppositional Defiant Behavior Inventory (SR-ODBI) in Persian and assess the validity and reliability of this Persian form.
3. Methods
3.1. Participants
This descriptive-correlational study was done on a statistical population of boy and girl high school students in Dezfoul city in the school year of 2019 - 2020. In the present study, two samples of parents (n = 320) and adolescents (n = 294) were selected using Cochran's formula. The age range of the total sample was 14 to 18 years, with a mean of 15.87 years and a standard deviation of 0.96. A multi-stage random sampling method was used in this study. To conduct this research, after obtaining official permission from the main developer of the inventory, the self-report version of the inventory was developed first based on the parent form, and it was reviewed by several psychology professors, and its content validity was examined. Then, it was implemented on several students, and the comprehensibility of its items was examined. After initial confirmation of the inventory, it was implemented on the main sample (294 students). Before students answered the questions of the inventory, the necessary explanations were given about the objectives of the research to encourage them to participate and cooperate in this study. Then, students were asked to rate their agreement with each of the items on a four-point Likert scale. A score of 0 to 3 was assigned to each item. All participants answered the oppositional defiant behavior inventory and the children and adolescents’ mental health inventory (to assess convergent validity). Also, by multi-stage random sampling method, 320 parents who had adolescents in this age group filled out the ODD questionnaire. This was a separate parent sample from the first sample. To assess the validity of the scale, the confirmatory factor analysis method and convergent validity were used. The reliability of the instrument was also assessed using Cronbach's alpha and split-half methods.
3.2. Ethical Considerations
The study was approved by the vice-chancellor of Research and Technology and the Ethics Committee of Chamran University of Ahvaz, Iran, on September 14, 2019 (registration No. EE/98.24.3.58240/Scu.ac.ir).
3.3. Measurements
The study used the self-report and parent forms of oppositional defiant behavior inventory to assess oppositional defiant disorder. The parent form of the inventory was developed by Harada et al. (12) in Japan for ages 6 - 15. The oppositional defiant inventory has 18 items and is filled out by parents or guardians of children and adolescents. Each question of the inventory has the options of "rarely, once or less a month", "sometimes, once a week", "often, two or three times a week", and "always, four times a week or more" with the scores of 0, 1, 2, and 3, respectively. The total score is in the range of 0 to 54, and according to the answers of parents and guardians, if the total score is more than 20, the oppositional defiant disorder will be diagnosed, and if the participant score is closer to 54, the disorder will be more severe (12).
Harada et al. (14) determined a cutoff score of 20 for distinguishing between children and adolescents with oppositional defiant disorder and other people who did not have this disorder. Concerning concurrent validity, both scores of oppositional defiant (test-retest) were correlated with the criteria of Diagnostic and Statistical Manual of Mental Disorders (0.65 and 0.659, P < 0.001) and disruptive behavior disorders rating (0.654 and 0.725, P < 0.00). The internal reliability of this test was obtained at 0.92 and 0.82, respectively, through Cronbach's alpha coefficient and split-half methods (12). The reliability of the oppositional defiant behavior inventory in the present was obtained as 0.73 for the self-report version and 0.85 for the parent version.
3.4. Youth Self-Report Test of Achenbach
The youth self-report test of Achenbach was developed by Achenbach (15). This list has three parallel forms, one of which is completed by the teacher, the other by the child, and the third one by the parents. In this study, the youth self-report test of Achenbach (YSR) was used. This list has two versions, one for children aged one to five years and the other for children aged six to 18 years. The second version of this list was used in this study. The subscales of this list are scored based on three options (incorrect, correct to some extent, and completely or mostly correct that received scores of zero, one, and two, respectively). In the present study, the oppositional defiant disorder subscale was used. Achenbach (16) standardized the youth mental health test on 1,753 children and adolescents aged six to 18 years from different cultures (American-African, Indian, European, Spanish-American, and other groups). In this standardization, Achenbach reported the validity of this tool at a satisfactory level. Achenbach reported the reliability of the subscales of this tool between 0.95 and 1 using the test-retest method, between 0.78 and 0.97 using the internal consistency method, and between 0.93 and 0.96 using the inter-rater reliability method (15). Minaei’s research presented acceptable validity and reliability for all three Persian versions (self-report, teacher, parents), and the range of internal consistency coefficients of the scales through Cronbach's alpha was 0.63 - 0.95 (16). In the present study, the reliability of this inventory was obtained at 0.72 through the Cronbach's alpha method and 0.69 through the Spearman-Brown split-half method.
3.5. Statistical Analysis
The analysis began with various preliminary analyses (mean, standard deviation, and Pearson correlation) to gain an initial insight into the data. Confirmatory factor analysis was then performed using AMOS software. All analyses were performed using SPSS version 22 and AMOS version 22 software. The model retention indices were reported.
4. Results
The demographics of children and parents and the mean and standard deviation of variables are shown in Table 1.
| Variable | Range | Full Sample (n = 294) | Male (n = 140) | Female (n = 154) |
|---|---|---|---|---|
| Age (y) | 14 - 18 | 15.87 ± 0.95 | 16.05 ± 0.79 | 16.11 ± 0.81 |
| CGPA | 11 - 20 | 18.43 ± 1.47 | 13.39 ± 6.62 | 18.09 ± 1.49 |
| ODB | 0 - 41 | 12.42 ± 7.56 | 24.65 ± 17.51 | 14.38 ± 10.56 |
| ODB (parents) | 0 - 31 | 7.1 ± 5.38 | 7.1 ± 5.38 | 7.1 ± 5.38 |
| Irritability | 0 - 24 | 6.30 ± 4.23 | 9.17 ± 5.99 | 6.85 ± 5.01 |
| Behavioral | 0 - 29 | 6.11 ± 4.22 | 14.04 ± 11.08 | 6.93 ± 5.74 |
| YSR | 0 - 10 | 2.98 ± 2.13 | 5.79 ± 4.42 | 3.63 ± 2.61 |
Abbreviations: CGPA, cumulative grade point average; ODB, oppositional defiant behavior; DBDR, Disruptive Behavior Disorders Rating Scale; YSR, Youth Self-Report test of Achenbach.
a Values are expressed as mean ± SD unless otherwise indicated.
As shown in Table 1, the mean (standard deviation) of the total score of students was 12.42 (7.56) in the oppositional defiant behavior inventory, while it is 7.1 (5.38) in the parent form. Besides, the mean score of students in the Achenbach youth mental health test was 2.98 (2.13). In the present study, in addition to confirmatory factor analysis, to examine the convergent validity of SR-ODBI, this inventory was implemented simultaneously with the youth mental health test. As mentioned earlier, 294 people filled out the inventories for this purpose. The correlation of students' scores in SR-ODBI and its two subscales with those in the Achenbach youth mental health test is given in Table 2.
a P < 0.01.
As shown in Table 2, the correlation between student scores in oppositional defiant behavior inventory and the Achenbach youth mental health test was significant at the level of P < 0.01. Investigating the correlation between the subscales of the two tools showed that the two subscales of the inventory, including irritability and stubborn/resentful behavior, and behavioral problems inventory were correlated (0.46 and 0.51, respectively). The correlation coefficients of subscale scores with each other and with the inventory were between 0.86 and 0.87, which were significant at the P = 0.01 level. A single question was also used to investigate the validity of the oppositional defiant behavior inventory, which was correlated with the total inventory (0.44).
Cronbach's alpha and split-half methods (Spearman-Brown and Guttman) were used to evaluate the reliability of the inventories. Here, the data of the whole sample were analyzed. The results of the data analysis are given in Table 3.
| Reliability | Cronbach's Alpha | Split-Half | ||||
|---|---|---|---|---|---|---|
| ODBI-SR | ODBI-P | Spearman-Brown | Guttman | |||
| ODBI-SR | ODBI-P | ODBI-SR | ODBI-P | |||
| Disruptive Behavior Disorders Rating Scale | 0.73 | 0.85 | 0.74 | 0.74 | 0.73 | 0.89 |
| Irritability | 0.72 | 0.79 | 0.73 | 0.80 | 0.70 | 0.80 |
| Behavioral | 0.81 | 0.76 | 0.83 | 0.73 | 0.80 | 0.79 |
| Youth Self Report test of Achenbach (YSR) | 0.70 | 0.69 | 0.70 | |||
As shown in Table 3, the reliability coefficients of the oppositional defiant behavior inventory by Cronbach's alpha, Spearman-Brown split-half, and Guttman methods were obtained at 0.73, 0.74, and 0.73, respectively, and they were obtained at 0.85, 0.74, and 0.89, respectively, for the parent form, indicating good reliability coefficients.
Confirmatory factor analysis was used to investigate the validity of the oppositional defiant behavior inventory. For this purpose, the data obtained from the implementation of the inventory were analyzed using analysis of moment structure (AMOS) version 22. Table 4 shows the factor loads of the oppositional defiant behavior inventory items (parent form and children form). Since this inventory has two scales of irritability and stubborn and resentful behaviors separately, confirmatory factor analysis was performed on both forms, and the results are shown in Table 4.
| Sub-scale and Questions | Self-report | Parent Report | ||
|---|---|---|---|---|
| Factor 1 | Factor 2 | Factor 1 | Factor 2 | |
| Irritability | ||||
| 1. I have temper tantrums when things do no go as I wish | 0.45 | 0.69 | ||
| 5. I blame my failure on someone else | 0.40 | 0.67 | ||
| 10. I feel inferior and get annoyed | 0.45 | 0.57 | ||
| 11. I get upset when warned | 0.55 | 0.60 | ||
| 12. I have temper tantrums when treated unkindly | 0.60 | 0.71 | ||
| 14. I interrupt others | 0.50 | 0.43 | ||
| 16. I get annoyed when things do no go as I wish | 0.52 | 0.52 | ||
| 17. I get upset when things are not to my liking | 0.54 | 0.62 | ||
| Behavioral | ||||
| 2. I talk back when I am warned | 0.43 | 0.65 | ||
| 3. I no dot obey others | 0.54 | 0.67 | ||
| 4. I deliberately do things that others dislike | 0.54 | 0.56 | ||
| 6. I misinterpret words or situations and become sulky | 0.31 | 0.46 | ||
| 7. I do mean things to siblings and friends | 0.46 | 0.68 | ||
| 8. I talk back when my thoughts or behavior are denied | 0.56 | 0.67 | ||
| 9. I make fools of siblings and friends | 0.30 | 0.42 | ||
| 13. I insist on my demands being accepted | 0.43 | 0.59 | ||
| 15. I do not apologize when I am to blame | 0.41 | 0.46 | ||
| 18. I grumble at people | 0.57 | 0.68 | ||
As shown in Table 4, in performing confirmatory factor analysis of oppositional defiant behavior inventory (parent and children forms), in the self-report form in the irritability subscale, the highest factor load was related to item 12 (0.60), and the lowest factor load was related to item 5 (0.40). Concerning the stubborn and resentful behavior subscale, the highest factor load was related to item 18 (0.57), and the lowest factor load was related to item 9 (0.30). In the parent form, the highest factor load was related to item 12 (0.71), and the lowest factor load was related to item 9 (0.42). Due to the appropriateness of the factor loads of both subscales, which are higher than 0.30, all the factor loads of the inventory were confirmed.
Table 5 presents the goodness-of-fit index resulting from confirmatory factor analysis, including chi-square, degree of freedom, significance level, normed chi-square measure, root mean square error of approximation (RMSEA), goodness-of-fit index (GFI), adjusted goodness-of-fit index (AGFI), normed fit index (NFI), comparative fit index, and incremental fit index.
| Fit Indicators | χ2 | df | χ2/df | GFI | AGFI | IFI | TLI | CFI | NFI | RMSEA |
|---|---|---|---|---|---|---|---|---|---|---|
| Final model (self-report form) | 328.618 | 148 | 2.22 | 0.91 | 0.88 | 0.90 | 0.85 | 0.90 | 0.83 | 0.06 |
| Final model (parent form) | 430.608 | 146 | 2.94 | 0.90 | 0.85 | 0.85 | 0.84 | 0.88 | 0.80 | 0.08 |
As shown in Table 5, the results of confirmatory factor analysis confirmed the relatively good fit of the two-factor structure of oppositional defiant behavior inventory. In the present study, the RMSEA index for the self-report version was obtained at 0.06. The other fit indices of the model were obtained as follows: (1) GFI = 0.91, (2) CFI = 0.90, and (3) IFI = 0.90. In the parent version, the RMSEA index was obtained at 0.08 and other fit indices were obtained as follows: (1) GFI = 0.90, (2) CFI = 0.88, and (3) IFI = 0.85. These data indicate the good fit of the self-report model while the parent form showed the indicators of the model were acceptable, but it is suggested that results be replicated in future research.
5. Discussion
In many countries, the parent version has been used, but the self-report version was not considered a special report for students. So, in this study, an attempt was made to adapt this self-report tool for children in Persian. The present study aimed to obtain a self-report version of the Harada et al. (12) tool and investigate the validity and reliability of the Persian version of the oppositional defiant behavior inventory using the confirmatory factor analysis method. As stated earlier, in this study, due to the emphasis of the research literature on two underlying factors and adjusting the inventory with the structure of DSM 5, a two-factor model of oppositional defiant disorder was used (17). The confirmatory factor analysis showed that the two-factor model fit was confirmed. All items of the questionnaire were preserved due to the desirability of the factor loads.
The Achenbach test was also used to examine the convergent validity of the scale. Both subscales of irritability and stubborn and resentful behavior showed a high correlation with the Achenbach test. Its self-report version was used for the first time in the present study, while many studies have been conducted around the world to assess the validity of the parent version. In examining the concurrent validity, Harada et al. (12) found that both scores of the oppositional defiant test (test-retest) were correlated with the criteria of DSM and Disruptive Behavior Disorders Rating Scale (DBDRS-ODD), as shown in Table 2.
To calculate the discriminative validity of this test, the mean scores of three groups of hyperactive-attention deficit/defiant-oppositional, hyperactive-attention-deficit, and control group were used. The mean scores were 20.5, 33.3, and 10.7, respectively, for the hyperactive-attention deficit, hyperactive-attention deficit/defiant-oppositional, and control groups, indicating that the difference between the scores of these groups was significant. In the study conducted by Naghdi Nasab, the Spielberger anxiety inventory was used (18, 19). The correlation coefficients between oppositional defiant behavior inventory, responded by parents, and Spielberger and anxiety inventory, completed by 100 middle-school girl students, were calculated. The results showed a relatively strong correlation between oppositional defiant behavior inventory and Spielberger and anxiety inventory and depression inventory.
In summary, the results of the present study showed that the oppositional defiant behavior inventory has acceptable validity and reliability and can be used to assess this structure. This scale can have many applications in psychological research, as well as in the field of diagnosis and differentiation of oppositional defiant disorder and conduct disorder and hyperactive-attention deficit.
5.1. Study Limitations
Since the statistical population of the present study was limited to the age group of 14 - 18 years, the results of this study may not apply to other populations such as children of lower age or other communities.
5.2. Recommendations
It is recommended that more studies be conducted in the future to examine its reliability and validity on a larger sample of children in lower age groups to investigate the effect of age on the efficiency of this scale. It is also proposed for counselors and therapists to use this tool as a practical index to identify and diagnose high-risk clients.
5.3. Conclusions
In general, the results of the present study indicated that the version of the oppositional defiant behavior inventory in Iran has good reliability and validity. This inventory is a useful tool for screening and early diagnosis so that with the help of this inventory, people with oppositional defiant behavior can be diagnosed in the early stages, and the necessary measures can be taken to treat them because these characteristics are thought to be treated in early life.