1. Background
Coronavirus disease 2019 (COVID-19) is a new infectious disease that causes severe acute respiratory symptoms. It was first identified in December 2019, in Wuhan, China, and has since spread globally (1). This is a new viral infection that does not have a treatment and currently can only be treated symptomatically (2). On January 30, 2020, the World Health Organization (WHO) declared a public health emergency of international concern (PHEIC) and, on February 11, announced that the new coronavirus would be called “COVID-19” (3). On March 11, 2020, WHO declared the coronavirus outbreak a “Global Pandemic" (4). Until April 2, 2020, COVID-19 has been reported from 216 countries with 6,194,533 confirmed cases and 376,320 deaths (5). Iran was ranked 10th globally in terms of confirmed cases of the disease on July 10, 2020 (6).
The COVID-19 pandemic has affected all aspects of people’s lives and has changed their lifestyles (7). This pandemic may also affect communities psychologically by increasing fear and isolation and decreasing social and economic activities (8). Lack of knowledge about COVID-19 is one of the main causes of stress among people. When WHO declared COVID-19 a global pandemic, fear, and anxiety about COVID-19 spread as fast as the virus itself. While the whole world was trying to find a vaccine and effective drugs, the best intervention to reduce the rate of disease transmission was announced to be social distancing and quarantine (9). The change in the term "social distance" to "physical distance" by WHO has caused people to feel lonely and socially isolated. As a result, people may experience mental disorders such as depression and sleep problems (9, 10).
Sleep is a naturally reversible state that contributes to physical and mental health, but disturbed sleep can cause a range of physical, mental, and emotional problems (11). Sleep quality is a key indicator of physical and mental health (12). Research has shown that sleep deprivation suppresses the immune system and causes depression (13, 14). Depression is the first most common mental illness, and is a natural response to awkward life situations (15). In addition to stress and anxiety, there are several factors that increase the chance of depression, including loneliness, staying away from others, misinformation on social media, and economic insecurity (9). With the progress of the COVID-19 epidemic to different stages, sleep and psychological conditions such as depression may change (16), and research on these psychological outcomes is necessary because the spread of COVID-19 in the Iranian population can have long-term psychological impacts (9).
2. Objectives
The main purpose of this study was to investigate depression and sleep quality and demographic factors related to it among Iranians during the COVID-19 pandemic.
3. Methods
This nationwide web-based cross-sectional study was conducted to evaluate depression and sleep quality in the Iranian general population during the COVID-19 pandemic in 2020. Data were collected from April 19 to May 12; and 3,446 people completed the questionnaire via the link. The questionnaire included demographic variables, the pittsburgh sleep quality index (PSQI), and the depression center for epidemiologic studies’ depression scale (CES-D 20).
Convenient sampling was done. The questionnaire was distributed as a web link through social networks, including Telegram, WhatsApp, and Instagram. According to Hyland et al. (2020) (17) in which the prevalence of depression was 23%, with a 95% confidence level 0.05 and error d = 0.014, the minimum sample size required was 3,436. Inclusion criteria were people over 18 years old with the ability to read and write. Questionnaires were completed without a name. Participation in the study was completely voluntary.
Demographic variables included in the questionnaire were gender (male, female), age (≤ 20, 21 - 30 , 31 - 40 , 40 - 51, and > 50 years), marital status (single, married, separated, which included divorced and widowed), having a history of depression or current depressive disorder (yes, no), education (high school diploma and less, graduate diploma, bachelor, masters, and doctorate), job (unemployed, retired, student, freelance job, employee), income (good, moderate and poor), having a child (yes, no), having COVID-19 disease in the last two months (yes, no, I do not know), the number of people with COVID-19 in the past two months whom the participant had known (nobody, 1 - 2, 3 - 5, > 5 people) and hours spent outside home during a day in the past two months (no time, 1 - 3, 4 - 7, > 7 hours).
The PSQI is a useful instrument used to measure the quality and patterns of sleep. It includes seven domains, which are sleep duration, sleep disturbance, sleep latency, daytime dysfunction due to sleepiness, habitual sleep efficiency, sleep quality, and the need to use medicine for sleep over the last month. The questionnaire has nine items, but question 5 itself contains ten sub-items, so the whole questionnaire has 19 items, which are scored on a 4-point Likert scale from 0 to 3. The values of "0" and "3" indicate "better" and "worse" sleep, respectively. The value of all seven domains is summed to get the total score. The overall score range of the PSQI questionnaire is from 0 to 21. A total score of ≤ 5 represents poor sleep quality and > 5 represents good sleep quality (18).
The CES-D is a 20-item scale to measure the current level of depression symptoms in the general population during the past week. The questionnaire has four subscales, somatic complaints, depressed affect, positive affect, and interpersonal problems. The Likert scale is from “0 = rarely or none of the time” to “4 = almost or all of the time". Items 4, 8, 12, and 16 are reversely scored. Scores range from 0 to 60; higher scores reflect greater levels of the depression symptoms, while lower scores reflect fewer symptoms. The cut-off point that has been recommended for depression cases is 20. Individuals with a score ≥ 20 or more are classified as having depression during the past week (19).
The validity and reliability of the questionnaires have already been confirmed in the Iranian community (20-22). This study was approved by the Ethics Committee of Shahrekord University of Medical Science (SKUMS). The ethics code for this study is IR.SKUMS.REC.1399.027.
We used descriptive statistics to summarize demographic characteristics and questionnaire scores. The mean of sleep quality and depression was compared in the demographic sub-groups. Each province was assumed as a cluster, and generalized estimating equations (GEE) models were used to determine the demographic variables that were related to depression symptoms and sleep quality. All independent variables were entered into the univariable model, and variables with a p-value of less than 0.2 were entered into the multivariable model. The final model was achieved using a backward selection approach. Odds ratio (OR), adjusted odds ratio (AOR), and 95% confidence intervals (95% CI) were reported. P-values of < 0.05 were considered statistically significant. All analyses were conducted with SPSS software version 26.
4. Results
In the present study, most participants were female (66.7%), were married (65%), were unemployed (34.1%), had a bachelor degree (35%), had at least one child (56.6%), perceived their income was moderate (67.6%), had no history of depression (76.3%) or COVID-19 in the last two months (84.6%). The mean (± SD) age of the participants was 34.2 (± 11.60) years and the average number of hours they spent out of home during a day in the past two months was 3.71 (± 4.60). The median number of people with COVID-19 whom the participants had known was 2.
The mean (± SD) of sleep quality and depression scores in the Iranian provinces are reported in Table 1. The provinces with the worst situation in sleep quality were Ilam, Semnan, and West Azabayejan; and the provinces with the worst situation in regard to depression were Sistan and Baluchestan, Golestan, and South Khorasan.
| Variables | No. % | Sleep Quality | Depression | ||||
|---|---|---|---|---|---|---|---|
| Mean (± SD) | Good | Poor | Mean (± SD) | Depression | No Depression | ||
| Esfahan | 360 (10.4) | 18.16 (± 11.02) | 100 (27.8) | 260 (72.2) | 7.28 (± 2.79) | 48 (43.6) | 62 (56.2) |
| Alborz | 55 (1.6) | 18.54 (± 13.21) | 9 (16.4) | 46 (83.6) | 7.89 (± 2.78) | 24 (43.6) | 31 (56.4) |
| Khuzestan | 162 (4.7) | 18.63 (± 11.65) | 40 (24.7) | 122 (75.3) | 8.00 (± 3.09) | 63 (38.9) | 99 (61.1) |
| Tehran | 379 (11.0) | 18.21 (± 11.28) | 98 (25.9) | 281 (74.1) | 7.63 (± 2.96) | 144 (38.0) | 235 (62.0) |
| Markazi | 45 (1.3) | 18.44 (± 12.12) | 9 (20.0) | 36 (80.0) | 7.55 (± 2.46) | 30 (66.7) | 15 (33.3) |
| Bushehr | 38 (1.1) | 18.52 (± 12.17) | 12 (31.6) | 26 (68.4) | 7.36 (± 2.68) | 17 (44.7) | 21 (55.3) |
| Chahar Mahal Bakhtiari | 482 (14.0) | 18.38 (± 11.41) | 160 (33.2) | 322 (68.4) | 6.97 (± 2.79) | 188 (39.0) | 294 (61.0) |
| Kerman | 100 (2.9) | 17.40 (± 12.18) | 19 (19) | 81 (81) | 7.58 (± 0.49) | 40 (40.0) | 60 (60.0) |
| Hormozgan | 71 (2.1) | 20.28 (± 12.07) | 21 (29.6) | 50 (70.4) | 7.38 (± 2.83) | 31 (43.7) | 40 (56.3) |
| Sistan and Baluchestan | 153 (4.4) | 23.99 (± 12.08) | 24 (15.7) | 129 (84.3) | 8.15 (± 2.83) | 100 (65.4) | 53 (34.6) |
| Zanjan | 110 (3.2) | 18.58 (± 12.02) | 30 (27.3) | 80 (72.5) | 7.17 (± 2.78) | 48 (43.6) | 62 (56.2) |
| Ilam | 7 (0.2) | 13.57 (± 8.05) | 1 (14.3) | 6 (85.7) | 7.28 (± 1.79) | 1 (14.3) | 6 (85.7) |
| Qom | 101 (2.9) | 21.46 (± 12.44) | 24 (23.8) | 77 (76.2) | 7.91 (± 3.20) | 49 (48.5) | 52 (51.5) |
| Lorestan | 74 (2.1) | 19.51 (± 12.23) | 21 (28.4) | 53 (71.6) | 7.45 (± 3.16) | 28 (37.8) | 46 (62.2) |
| Khorasan Razavi | 277 (8.0) | 22.00 (± 12.43) | 69 (24.9) | 208 (75.1) | 7.68 (± 2.79) | 145 (52.3) | 132 (47.7) |
| Kohgiluyeh and Boyer-Ahmad | 131 (3.8) | 17.70 (± 10.99) | 41 (31.3) | 90 (68.7) | 7.57 (± 3.11) | 49 (37.4) | 82 (62.6) |
| Fars | 160 (4.6) | 17.87 (± 11.85) | 55 (34.4) | 105 (65.6) | 7.45 (± 3.18) | 61 (38.1) | 99 (61.9) |
| Hamedan | 72 (2.1) | 18.51 (± 11.03) | 10 (13.9) | 62 (86.1) | 7.75 (± 2.56) | 33 (45.8) | 39 (54.2) |
| Yazd | 87 (2.5) | 17.05 (± 11.25) | 20 (23.0) | 67 (77.0) | 7.83 (± 2.84) | 35 (40.2) | 52 (59.8) |
| Semnan | 22 (0.6) | 15.13 (± 10.43) | 6 (27.3) | 16 (72.7) | 6.81 (± 2.70) | 3 (13.6) | 19 (86.4) |
| Golestan | 34 (1.0) | 21.00 (± 11.75) | 4 (11.8) | 30 (88.2) | 9.20 (± 3.20) | 17 (50.0) | 17 (50.0) |
| East Azarbaijan | 40 (1.2) | 18.57 (± 11.78) | 16 (26.7) | 44 (73.3) | 7.32 (± 3.18) | 15 (37.5) | 25 (62.5) |
| Kurdistan | 43 (1.2) | 17.13 (± 11.55) | 10 (23.3) | 33 (76.7) | 7.39 (± 2.47) | 17 (39.5) | 26 (60.5) |
| West Azerbaijan | 60 (1.7) | 15.55 (± 10.72) | 13 (32.5) | 27 (67.5) | 7.08 (± 2.27) | 18 (30.0) | 42 (70.0) |
| Qazvin | 72 (2.1) | 16.98 (± 10.65) | 19 (26.4) | 53 (73.6) | 7.34 (± 3.02) | 27 (37.5) | 45 (62.5) |
| Mazandaran | 68 (2.0) | 17.16 (± 10.48) | 16 (23.5) | 52 (76.5) | 7.55 (± 2.60) | 24 (35.3) | 44 (64.7) |
| Kermanshah | 51 (1.5) | 18.70 (± 11.20) | 13 (25.5) | 38 (74.5) | 7.31 (± 2.33) | 19 (37.3) | 32 (62.7) |
| North Khorasan | 37 (1.1) | 20.67 (± 12.54) | 11 (29.7) | 26 (70.3) | 7.72 (± 3.87) | 18 (48.6) | 19 (54.1) |
| Ardabil | 18 (0.5) | 22.83 (± 10.29) | 4 (22.2) | 14 (77.8) | 7.83 (± 2.83) | 11 (61.1) | 7 (38.9) |
| South Khorasan | 12 (0.34) | 25.41 (± 12.80) | 1 (8.1) | 11 (91.7) | 8.33 (± 2.83) | 7 (58.3) | 5 (41.7) |
| Gilan | 125 (3.6) | 18.02 (± 12.14) | 36 (28.8) | 89 (71.2) | 7.52 (± 2.91) | 44 (35.2) | 81 (64.8) |
The Mean (± SD) and Prevalence of Sleep Quality and Depression in the Provinces in Iran
The mean (± SD) of sleep quality and depression scores in demographic subgroups are presented in Table 2. Predictors of sleep quality and depression in univariable and multivariate analysis are outlined in Tables 3 and 4, respectively.
| Variables | No. (%) | Depression | Sleep Quality | ||||
|---|---|---|---|---|---|---|---|
| No Depression | Depression | P-Value | Good Sleep Quality | Poor Sleep Quality | P-Value | ||
| Overall | 3446 (100) | 2018 (58.6) | 1428 (41.4) | - | 912 (26.5) | 2534 (73.5) | - |
| Gender | < 0.001 | < 0.001 | |||||
| Male | 1146 (33.3) | 733 (64.0) | 413 (36.0) | 354 (30.9) | 792 (69.1) | ||
| Female | 2300 (66.7) | 1285 (55.9) | 1015 (44.1) | 558 (24.3) | 1742 (75.7) | ||
| Age (y) | < 0.001 | 0.004 | |||||
| 20 and under | 417 (12.1) | 183 (43.9) | 234 (56.1) | 90 (21.6) | 327 (78.4) | ||
| 21 - 30 | 973 (28.2) | 524 (53.9) | 449 (46.1) | 246 (25.3) | 727 (74.7) | ||
| 31 - 40 | 1132 (32.8) | 675 (59.6) | 457 (40.4) | 305 (26.9) | 827 (73.1) | ||
| 41 - 50 | 603 (17.5) | 399 (66.2) | 204 (33.8) | 180 (29.9) | 423 (70.1) | ||
| Over 50 | 321 (9.4) | 237 (73.8) | 84 (26.2) | 91 (28.3) | 230 (71.7) | ||
| Marital status | < 0.001 | 0.029 | |||||
| Single | 1106 (32.1) | 559 (50.5) | 547 (49.5) | 275 (24.9) | 831 (75.1) | ||
| Divorced/widow | 100 (2.9) | 52 (52.0) | 48 (48.0) | 20 (20.0) | 80 (80.0) | ||
| Married | 2240 (65.0) | 1407 (62.8) | 833 (37.2) | 617 (27.5) | 1623 (72.5) | ||
| Having a child or children | < 0.001 | 0.064 | |||||
| Yes | 1950 (56.6) | 1245 (63.8) | 705 (36.2) | 540 (27.7) | 1410 (72.3) | ||
| No | 1495 (43.4) | 733 (51.7) | 722 (48.3) | 372 (24.9) | 1123 (75.1) | ||
| Education | < 0.001 | 0.064 | |||||
| Diploma and less | 1182 (34.3) | 600 (50.8) | 582 (49.2) | 277 (23.4) | 905 (76.6) | ||
| Graduate diploma | 376 (10.9) | 220 (58.5) | 156 (41.5) | 94 (25.0) | 282 (75.0) | ||
| Bachelor | 1207 (35.0) | 741 (61.4) | 466 (38.6) | 337 (27.9) | 870 (72.1) | ||
| Masters/doctorate | 681 (19.8) | 457 (67.1) | 224 (32.9) | 204 (30.0) | 477 (70.0) | ||
| Job | 0.028 | 0.360 | |||||
| Unemployed | 1176 (34.1) | 581 (49.4) | 595 (50.6) | 268 (22.8) | 908 (77.2) | ||
| Freelance job | 575 (16.7) | 361 (62.8) | 214 (37.2) | 163 (28.3) | 412 (71.7) | ||
| Employee | 962 (27.9) | 661 (68.7) | 301 (31.3) | 305 (31.7) | 657 (68.3) | ||
| Student | 553 (16.0) | 281 (50.8) | 272 (49.2) | 121 (21.9) | 432 (78.1) | ||
| Retired | 180 (5.2) | 134 (74.4) | 46 (25.6) | 55 (30.6) | 125 (69.4) | ||
| Perceived income | < 0.001 | 0.001 | |||||
| Good | 486 (14.1) | 338 (69.5) | 148 (30.5) | 147 (30.2) | 339 (69.8) | ||
| Moderate | 2328 (67.6) | 1419 (61.0) | 909 (39.0) | 627 (26.9) | 1701 (73.1) | ||
| Poor | 632 (18.3) | 261 (41.3) | 371 (58.7) | 138 (21.8) | 494 (78.2) | ||
| Having COVID-19 disease in the last two months | 0.004 | < 0.001 | |||||
| Yes | 61 (1.8) | 34 (55.7) | 27 (44.3) | 14 (23.0) | 47 (77.0) | ||
| No | 2917 (84.6) | 1738 (59.6) | 1179 (40.4) | 808 (27.7) | 2109 (72.3) | ||
| I don't know | 468 (13.6) | 246 (52.6) | 222 (47.4) | 90 (19.2) | 378 (80.8) | ||
| The number of people with COVID-19 in the past two months whom they knew | 0.995 | 0.009 | |||||
| Nobody | 1113 (32.3) | 637 (57.2) | 476 (42.8) | 311 (27.9) | 802 (72.1) | ||
| 1 - 2 | 796 (23.1) | 475 (59.7) | 321 (40.3) | 235 (29.5) | 561 (70.5) | ||
| 3 - 5 | 804 (23.3) | 489 (60.8) | 315 (39.2) | 203 (25.2) | 601 (74.8) | ||
| Over 5 | 584 (16.9) | 325 (55.7) | 259 (44.3) | 132 (22.6) | 452 (77.4) | ||
| Hours spent outside home | < 0.001 | < 0.001 | |||||
| No time | 1218 (35.3) | 637 (52.3) | 581 (47.7) | 275 (22.6) | 943 (77.4) | ||
| 1 - 3 | 933 (27.1) | 544 (58.3) | 389 (41.7) | 237 (25.4) | 696 (74.6) | ||
| 4 - 7 | 365 (10.6) | 236 (64.6) | 129 (35.4) | 104 (28.5) | 261 (71.5) | ||
| Over 7 | 930 (27.0) | 601 (64.6) | 329 (35.4) | 296 (31.8) | 634 (68.2) | ||
Association Between Demographic Variables and the Psychological Impact of Novel Coronavirus Disease 2019 (COVID-19)
| Variables | Depression | Sleep Quality | ||
|---|---|---|---|---|
| OR (95% CI) | P-Value | OR (95% CI) | P-Value | |
| Gender | ||||
| Female | 1.40 (1.22, 1.61) | < 0.001 | 1.39 (1.20, 1.61) | < 0.001 |
| Male | 1 | 1 | 1 | 1 |
| Age (y) | ||||
| 20 and under | 3.60 (2.66, 4.88) | < 0.001 | 1.43 (1.03, 2.00) | 0.032 |
| 21 - 30 | 2.41 (1.86, 3.13) | < 0.001 | 1.16 (0.89, 1.53) | 0.261 |
| 31 - 40 | 1.91 (1.47, 2.46) | < 0.001 | 1.07 (0.82, 1.40) | 0.605 |
| 41 - 50 | 1.44 (1.09, 1.89) | < 0.001 | 0.93 (0.69, 1.24) | 0.620 |
| Over 50 | 1 | 1 | 1 | 1 |
| Marital status | ||||
| Single | 1.65 (1.43, 1.90) | < 0.001 | 1.14 (0.96, 1.36) | 0.118 |
| Divorced/widow | 1.55 (1.04, 2.32) | 0.030 | 1.52 (0.92, 2.49) | 0.097 |
| Married | 1 | 1 | 1 | 1 |
| Having a child or children | ||||
| No | 1.64 (1.42, 1.90) | < 0.001 | 1.15 (0.97, 1.37) | 0.097 |
| Yes | 1 | 1 | 1 | 1 |
| Education | ||||
| Diploma and less | 1.97 (1.62, 2.40) | < 0.001 | 1.20 (1.11, 1.75) | 0.004 |
| Associate degree | 1.44 (1.11, 1.87) | 0.005 | 1.28 (0.96, 1.70) | 0.086 |
| Bachelor | 1.28 (1.05, 1.55) | 0.012 | 1.10 (0.88, 1.37) | 0.378 |
| Masters/doctorate | 1 | 1 | 1 | 1 |
| Job | ||||
| Unemployed | 2.98 (2.11, 4.20) | < 0.001 | 1.49 (1.08, 2.05) | 0.015 |
| Freelance job | 1.72 (1.23, 2.42) | 0.002 | 1.11 (0.77, 1.60) | 0.571 |
| Employee | 1.327 (0.93, 1.87) | 0.112 | 0.94 (0.67, 1.34) | 0.762 |
| Student | 2.820 (1.95, 4.06) | < 0.001 | 1.57 (1.06, 2.32) | 0.023 |
| Retired | 1 | 1 | 1 | 1 |
| Perceived income | ||||
| Poor | 3.24 (2.56, 4.10) | < 0.001 | 1.55 (1.19, 2.01) | 0.001 |
| Moderate | 1.46 (1.20, 1.78) | < 0.001 | 0.78 (0.95, 1.45) | 0.129 |
| Good | 1 | 1 | 1 | 1 |
| Having COVID-19 disease in the last two months | ||||
| Yes | 1.17 (0.70, 1.95) | 0.545 | 1.28 (0.72, 2.27) | 0.388 |
| I don't know | 1.33 (1.07, 1.64) | 0.008 | 1.60 (1.27, 2.03) | < 0.001 |
| No | 1 | 1 | 1 | 1 |
| The number of people with COVID-19 in the past two months whom they knew | ||||
| 1 - 2 | 0.90 (0.75, 1.08) | 0.266 | 0.92 (0.77, 1.10) | 0.403 |
| 3 - 5 | 0.86 (0.71, 1.04) | 0.133 | 1.14 (0.93, 1.40) | 0.181 |
| Over 5 | 1.06 (0.86, 1.31) | 0.544 | 1.32 (1.04, 1.68) | 0.018 |
| Nobody | 1 | 1 | 1 | 1 |
| Hours spent outside home | ||||
| 1 - 3 | 1.66 (1.41, 1.96) | < 0.001 | 1.60 (1.31, 1.95) | < 0.001 |
| 4 - 7 | 1.30 (1.09, 1.56) | 0.004 | 1.37 (1.12, 1.67) | 0.002 |
| Over 7 | 0.99 (0.78, 1.26) | 0.990 | 1.17 (0.90, 1.52) | 0.236 |
| No time | 1 | 1 | 1 | 1 |
| Depression history | ||||
| Yes | 4.74 (4.09, 5.49) | < 0.001 | 2.97 (2.41, 3.66) | < 0.001 |
| No | 1 | 1 | 1 | 1 |
Univariable Generalized Estimating Equation Results about the Association between Demographic Variables, Depression, and Sleep Quality
| Variables | Depression | Sleep Quality | ||
|---|---|---|---|---|
| OR (95% CI) | P-Value | OR (95% CI) | P-Value | |
| Gender | ||||
| Female | 1.36 (1.15, 1.59) | < 0.001 | - | - |
| Male | 1 | 1 | - | - |
| Age (y) | ||||
| ≤ 20 | 2.51 (1.73, 3.64) | < 0.001 | - | - |
| 21 - 30 | 1.90 (1.40, 2.58) | < 0.001 | - | - |
| 31 - 40 | 1.66 (1.24, 2.22) | 0.001 | - | - |
| 41 - 50 | 1.28 (0.93, 1.77) | 0.123 | - | - |
| Over 50 | 1 | 1 | - | - |
| Having a child or children | ||||
| No | 1.43 (1.16, 1.75) | 0.001 | - | - |
| Yes | 1 | 1 | - | - |
| Education | ||||
| High school Diploma or less | 1.58 (1.24, 2.01) | < 0.001 | - | - |
| Graduate diploma | 1.27 (0.95, 1.71) | 0.097 | - | - |
| Bachelor | 1.19 (0.95, 1.48) | 0.114 | - | - |
| Masters/doctorate | 1 | 1 | - | - |
| Perceived income | ||||
| Poor | 3.17 (2.45, 4.11) | < 0.001 | 1.43 (1.09, 1.89) | 0.009 |
| Moderate | 1.46 (1.25, 1.91) | < 0.001 | 0.78 (0.90, 1.41) | 0.282 |
| Good | 1 | 1 | 1 | 1 |
| Having COVID-19 disease in the last two months | ||||
| Yes | 1.14 (0.61, 2.12) | 0.676 | 1.01 (0.56, 1.84) | 0.952 |
| I don't know | 1.37 (1.09, 1.73) | 0.006 | 1.59 (1.24, 2.03) | < 0.001 |
| No | 1 | 1 | 1 | 1 |
| The number of people with COVID-19 in the past two months whom they knew | ||||
| 1 - 2 | - | - | 0.94 (0.78, 1.13) | 0.519 |
| 3 - 5 | - | - | 1.17 (0.95, 1.43) | 0.132 |
| Over 5 | - | - | 1.41 (1.10, 1.81) | 0.007 |
| Nobody | - | - | 1 | 1 |
| Hours spent outside home | ||||
| 1 - 3 | - | - | 0.88 (0.71, 1.09) | 0.245 |
| 4 - 7 | - | - | 0.73 (0.57, 0.94) | 0.014 |
| Over 7 | - | - | 0.63 (0.51, 0.77) | < 0.001 |
| No time | - | - | 1 | 1 |
Multivariable Generalized Estimating Equation Results about the Association between Demographic Variables, Depression, and Sleep Quality
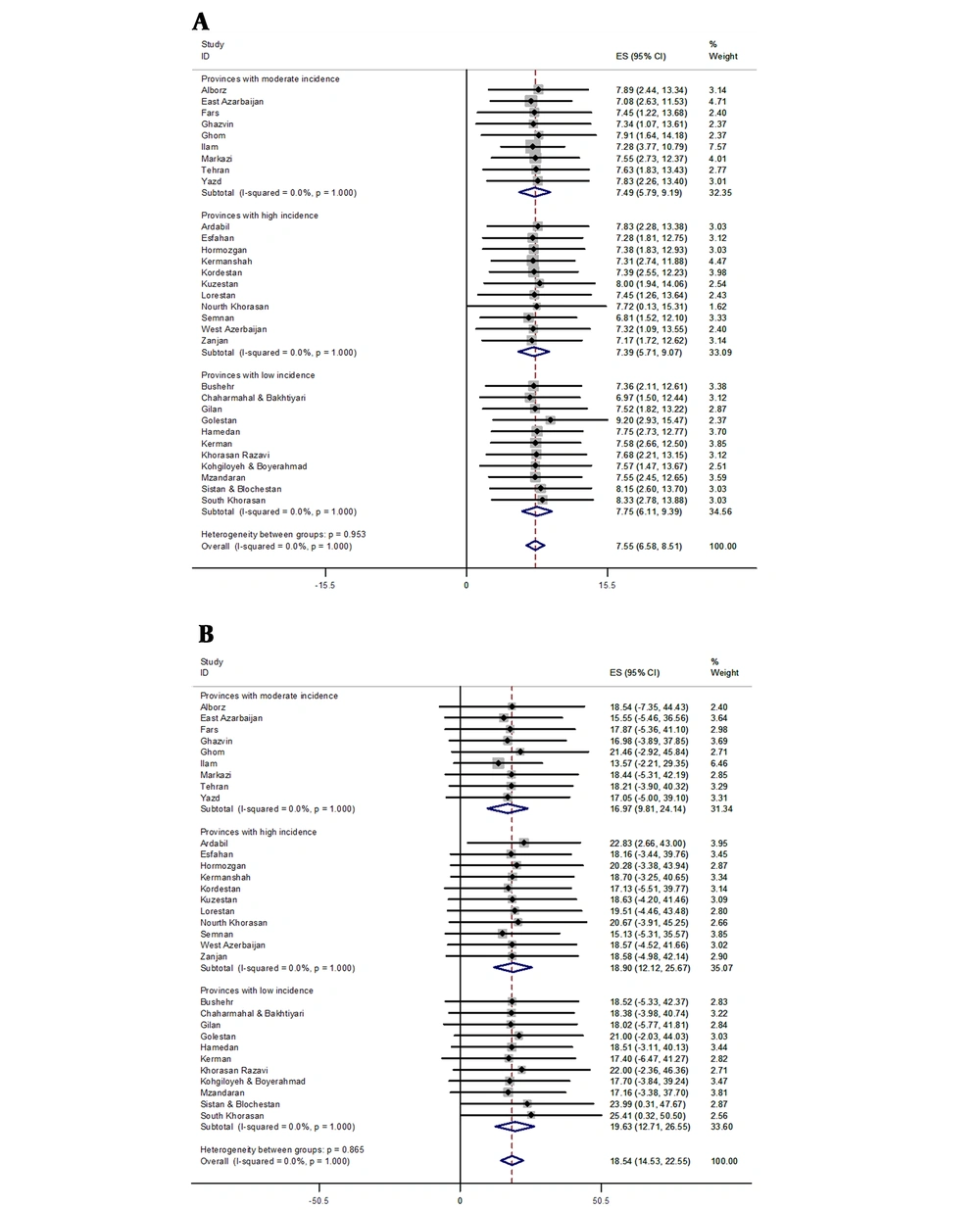
In this study, 73.5% of participants had poor sleep quality. The mean (± SD) of the sleep quality scores was 7.51 (± 2.88). The mean scores of sleep quality in different COVID-19 incidence (high, medium, and low) provinces are shown in Figure 1A. There was no significant difference between these provinces in terms of sleep quality.
The variables in the multivariable model that were significantly associated with sleep quality were poor perceived income, not knowing about getting infected with COVID-19 in the last two months, knowing more than 5 people who got COVID-19, spending 4 - 7 hours or more than 7 hours outside the home, and having a history of depression (Table 4).
About 41.4% of the participants had depression symptoms. The mean (± SD) of participants' depression score was 18.89 (± 11.72). The mean scores of depression in different COVID-19 incidence (high, medium, and low) provinces are shown in Figure 1B. There was no significant difference between these provinces in terms of depression.
The variables that were significantly associated with depression and stayed in the final multivariable model were female sex, age groups, including ages ≤ 20, 21 - 30 and 31 - 40 years, not having children, high school diploma or less education, perceived poor or moderate-income, not knowing about getting infected with COVID-19 in the last two months, and having a history of depression (Table 4).
5. Discussion
The present study found that most participants had poor sleep quality and less than half had depression symptoms during the COVID-19 pandemic in Iran.
In a web-based cross-sectional survey in China during COVID-19 outbreak, about 18.2% of the general population had poor sleep quality (4), and among medical staff who manage patients with COVID-19 in January and February 2020, social support was significantly associated with self-efficacy and sleep quality; thus anxiety, stress, and self-efficacy were mediating variables related to sleep quality (2). Also, in China, the PSQI score was significantly higher in nursing interns during outbreak of COVID-19 than national norms, and depression positively correlated with the sleep quality score (23). Studies have shown that good quality sleep enhances psychoneuroimmunity against COVID-19 (7). The world sleep society has highlighted the importance of sleep as the basis of health, which helps in better decision making and cognitive understanding, even in big issues like COVID-19 pandemic (24). Researchers think getting enough sleep is not a luxury, it is something people need for good health, and sleep disorders can increase a person’s risk of health problems (25). Mental health is also affected by disturbed sleep. Insufficient sleep, less than 5 h per day, is associated with higher rates of depression, stress, and suicide. Sleep deficiency is also associated with bad moods, poor emotional regulation (26), poor mental health, and even early death (27). Sleep deficiency and sleep latency can cause behavioral problems that include (28) internalized behaviors such as anxiety, depression, excess worry, psychosomatic symptoms, and externalized behaviors such as aggression, impulsive or disruptive behaviors, delinquency, and non-compliance (29). Many factors play a role in sleep quality, including occupation, beliefs, age, the living environment, and social factors. It is important to discover populations at high risk of sleep deprivation and provide the right type of intervention (11).
In this study, less than half of the participants had symptoms of depression. In a survey conducted during the COVID-19 pandemic in Iran, the prevalence of depression was significantly higher among doctors (52%) and nurses (51.4%) compared with other occupations (30). In Guiyang, during the COVID-19 outbreak, the mean scores of depression among medical staff members were significantly higher than the general Chinese population (31). In the present study, unemployed people and students were more depressed in the univariable analysis. Similarly, during the COVID-19 pandemic in China, college students were more depressed than the normal national population (32) and younger participants were more likely to show depression symptoms than older participants, which is similar to our study (4). In Nepal, during the COVID-19 pandemic, the prevalence of depression was 34.0%, and multivariable analysis showed that females and those living alone were significantly more likely to have depression, which is consistent with the present study (33). A review study has mentioned that depression is one of the common psychological reactions to the COVID-19 pandemic (34).
Long-term self-isolation, social distancing, and lockdowns are not well tolerated by people and can have adverse psychological effects (35). In this study, most people with poor sleep quality and depression had poor income. This is probably because, COVID-19 pandemic has stopped or slowed down many businesses and industries, borders are closed, and traveling has decreased significantly (35).
The limitations of the study are that we enrolled volunteers by an online link, and we did not do random sampling. Another limitation of this cross-sectional study is that it shows associations but cannot prove causality.
5.1. Conclusion
Less than half of the participants of this study had symptoms of depression, and almost two-thirds had poor sleep quality. These psychological problems may disrupt their daily routines, cut their social ties, and increase their worries and fears of the future. These psychological issues should be monitored and need increased attention in times of crisis. Psychological interventions may be necessary during the COVID-19 pandemic.