1. Background
In December 2019, a new virus, called SARS-CoV-2, was reported for the first time in Wuhan, China (1), which attracted the global attention (2). This virus spread rapidly from China to other parts of the world, and in less than three months, about 200 countries reported this viral infection (COVID-19). Iran is one of the countries that has been extremely affected by this virus (3). Considering the high rate of virus propagation, shortly after the first case of COVID-19 was reported, the number of hospitalizations started to increase dramatically. The healthcare staff, who are at the forefront of the fight against this disease, are under significant pressure due to the high risk of infection, inadequate protection against contamination, work overload, fatigue, lack of contact with family, and a sense of disability in disease control, all of which can lead to mental problems, such as anxiety, depression, insomnia, anger, and job burnout (4).
Nurses and physicians are the largest group of healthcare providers, who play a critical role in the healthcare system of all countries. Research conducted before the COVID-19 pandemic showed that healthcare professionals experienced higher levels of stress, compared to other occupational groups (5, 6). Also, previous studies in Iran revealed that the prevalence of mental problems was 43% in this group (7). Considering the pressure imposed by this pandemic on the healthcare staff, the rate of mental health problems may increase. In this regard, researchers conducted a cross-sectional study in China on a sample of healthcare workers, 42% of whom directly cared for patients affected by COVID-19. They found that among surveyed workers, 50% had depression, 45% had anxiety, 34% had insomnia, and 72% had distress symptoms. These problems were more common among nurses than physicians and among women than men. Besides, 10 to 20% of them had moderate or severe symptoms (8).
Another occupational hazard is job burnout, especially in stressful jobs. It is described as a type of emotional exhaustion, associated with personality deterioration and reduced self-esteem, which may lead to reduced functionality and job commitment (9). Medical staff are more prone to job burnout as a result of exposure to stressors, such as interpersonal problems, high exposure to patients’ mortality, long work shifts, insufficient knowledge or lack of appropriate decision-making skills, and the need to make quick decisions in emergencies (10-13). Since job burnout is a result of long exposure to chronic job stressors, it occurs later in one’s career and is relatively stable over time if the person stays in the same job.
The link between mental health and job burnout is complex. There are some arguments that job burnout has negative mental effects, such as anxiety, depression, and low self-esteem. However, an alternative and more common argument is that people who are mentally healthy are better able to cope with chronic stressors and are therefore less likely to experience burnout (14). In this regard, a previous study analyzed the archived longitudinal data of individuals who had interpersonally demanding jobs and revealed that people with better psychological health during adolescence and early adulthood were more likely to choose and stay in such occupations; they also showed more involvement and satisfaction with their jobs (15).
Another study investigating the physicians’ burnout revealed that 43% of the participants experienced high emotional fatigue, 35% experienced major personality changes, and 32% showed low self-efficacy on a burnout scale (16). In another study, the levels of stress and burnout were very high, and half of the surveyed physicians reported high levels of emotional exhaustion and change. Furthermore, there was a relationship between occupational stress and job burnout; in other words, by increasing occupational stress, the physician's burnout increased, as well (17).
Moreover, a study on the medical emergency personnel in Tehran, Iran, revealed that 37.5% of the staff were emotionally exhausted, 44% experienced depersonalization , and 57% experienced self-inadequacy (18). Therefore, it seems that stress caused by the spread of COVID-19, along with the long working hours, may increase the level of job burnout. According to previous research, exposure to stressful situations can lead to increased job burnout. However, some factors, such as resilience, may play a protective role (19).
Resilience is a person’s ability to adapt successfully to threatening situations. It is defined as a person's confidence in his/her coping skills, self-esteem, emotional stability, ability to cope with stress, and individual characteristics that increase social support. Conner and Davidson claimed that resilience does not only refer to resistance against trauma and threatening situations, but also involves active and constructive engagement with the environment (20). Numerous studies have shown that resilience is an important factor in some high-risk groups, which plays an essential mediating role in the development of mental disorders (21). Therefore, it may be considered as a protective factor for those who work in stressful situations, such as healthcare workers during pandemics. Besides, it may prevent the adverse psychopathological consequences of COVID-19 from becoming chronic (22).
Some studies have shown that the process of resilience changes over time and can greatly contribute to a person's mental health after painful and unwanted experiences (17). One study showed that greater resilience was related to lower levels of burnout among the medical emergency personnel and was associated with their adaptability to stressors (18). Since traumatic and challenging events can affect one’s psychological adjustment skills, evaluation of the mental health status of healthcare staff is an important issue during the stressful outbreak of COVID-19.
Although epidemiological data about the psychological effects of COVID-19 on the public mental health are still limited, psychological problems, including loneliness, boredom, anxiety, sleep problems, and anger, have been documented (23). Previous studies have revealed the mediating role of resilience in the relationship between traumatic events and psychopathology, whereas the mediating role of resilience in the relationship between the COVID-19 pandemic, job burnout, and mental health of healthcare workers remains unclear. Therefore, it seems necessary to investigate the mental health problems and burnout of medical staff during this pandemic to update the available information about its possible psychological consequences. These results may be helpful in identifying the medical staff at risk of mental health problems and can have some implications for delivering psychological services to this group to prevent the progression of these problems.
2. Objectives
The present study aimed to examine the job burnout and mental health of nurses during the COVID-19 pandemic and to explore the mediating role of resilience in the relationship between mental health and job burnout.
3. Methods
3.1. Participants
This cross-sectional study was carried out in two public hospitals of Kashan and Aran-o-Bidgol, Iran. The study population consisted of all nurses, who worked in Shahid Beheshti Hospital of Kashan or Seyed Al-Shohada Hospital of Aran-o-Bidgol from March 2020 to the end of June 2020. Green and Harris suggested a formula (N ≥ 50 + 8 m, where m denotes the number of predictors) for determining the minimum number of subjects required to conduct a multiple regression analysis (23, 24). According to this formula and the number of predictors in this study (m = 6), the minimum sample size was measured to be 98; for assurance, the sample size was increased by 10%. Finally, the sample size was measured to be 110 individuals. In this study, 108 nurses completed the questionnaires. All 20- to 60-year-old nurses working in these hospitals during the COVID-19 pandemic were included. Withdrawal from work in less than one week from the COVID-19 outbreak was the exclusion criterion.
3.2. Procedures
The questionnaires were prepared online in Google Docs. The link to the questionnaire was provided for the medical staff of Shahid Beheshti Hospital of Kashan and Seyyed-Al-Shohada Hospital of Aran-o-Bidgol in collaboration with the public relations sectors of these hospitals, public relations sector of Kashan University of Medical Sciences, and social networks so that individuals who were interested in participation could complete them. The participants were given the opportunity to access their results by providing their email address. The participants’ contact number was documented so that they could be followed-up and provided with counseling services if they had severe mental health problems.
3.3. Ethical Considerations
This study was approved by the Ethics Committee of Kashan University of Medical Sciences (Ethical ID: IR.KAUMS.MEDNT.REC.1399.019). The participants gave their informed consent to participate in the study before completing the questionnaires. The privacy and anonymity of the participants were completely protected.
3.4. Instruments
3.4.1. General Health Questionnaire-28 (GHQ-28)
The GHQ-28, which was originally developed by Goldberg and Hiller (25), is a well-known self-administered questionnaire for research purposes. This questionnaire examines the individual’s mental state over the past month. Its items cover four main areas: (1) somatic symptoms, (2) anxiety and insomnia, (3) social dysfunction, and (4) depression. All items of this questionnaire are scored based on a Likert scale, ranging from 0 to 3. A total score of 0 to 22 indicates a normal state, scores of 23 to 40 indicate mild problems, scores of 41 to 60 show moderate problems, and scores of 61 to 84 indicate severe mental health problems. In Iran, Taghavi examined the reliability and validity of this questionnaire and reported its reliability, using the test-retest method (0.70), split-half method (0.93), and Cronbach's alpha (0.90) (26).
3.4.2. Nurse’s Job Burnout Questionnaire
This 25-item questionnaire was developed by Salaree et al. in Iran in 2018 (27) to measure burnout in nurses by modeling the general Burnout questionnaires and conducting interviews with nurses working in the army medical centers. After extracting the items, they examined the validity and reliability of this scale. The validity of the questionnaire structure confirmed seven factors, based on the exploratory factor analysis, which explained 57.56% of total variance. The Cronbach's alpha coefficient of this scale was reported to be 0.91, and its reliability was measured to be 0.96.
3.4.3. Resilience Scale
This 25-item scale was designed by Connor and Davidson and rated on a five-point Likert scale, ranging from 0 to 4. The minimum score of this questionnaire is zero, and the maximum score is 100, with higher scores indicating higher resilience. Connor and Davidson reported a Cronbach's alpha coefficient of 0.89 and a reliability coefficient of 0.87 (21). So far, the psychometric properties of this scale have been investigated in several studies. In a previous study, 500 nursing students completed the questionnaire. Its internal consistency based on Cronbach’s alpha and test-retest coefficients was 0.66 and 0.66, respectively (28).
4. Results
As shown in Table 1, the mean age of the participants was 36.6 years (SD = 6.05), and the mean duration of employment was 8.07 (SD = 2.21) years. Most of the participants were married (67.6%). According to the cut-off values of the scales, 61.1% of the participants had mild to severe anxiety, 86% had mild to severe somatic symptoms, 73.2% experienced mild or moderate social withdrawal, and 14.9% had mild or moderate depression; none of the subjects reported severe symptoms of depression or social withdrawal. Only 13% of the respondents reported no job burnout. In terms of resilience, the results showed that most of the participants (88.9%) had moderate resilience (Table 2).
| Characteristics | No. (%) |
|---|---|
| Gender | |
| Female | 85 (78.7) |
| Male | 23 (21.3) |
| Age (y) | |
| 20 - 25 | 18 (16.7) |
| 26 - 30 | 30 (27.8) |
| 31 - 35 | 16 (14.8) |
| 36 - 40 | 22 (20.4) |
| 41 - 45 | 14 (13) |
| > 45 | 8 (7.4) |
| Marital status | |
| Single | 31 (28.7) |
| Married | 73 (67.6) |
| Divorced | 4 (3.8) |
| Duration of employment (y) | |
| < 3 | 30 (27.8) |
| 3 - 6 | 20 (18.5) |
| 7 - 10 | 14 (13) |
| 11 - 15 | 22 (20.35) |
| > 15 | 22 (20.35) |
The Sociodemographic Characteristics of Nurses Working During the COVID-19 Outbreak (n = 108)
| Variables | None | Mild | Moderate | Severe |
|---|---|---|---|---|
| Anxiety | 42 (38.9) | 28 (25.9) | 22 (20.4) | 16 (14.8) |
| Somatic symptoms | 14 (13) | 48 (44.4) | 32 (29.6) | 14 (13) |
| Social withdrawal | 29 (26.9) | 65 (60.2) | 14 (13) | 0 |
| Depression | 92 (85.2) | 14 (13) | 2 (1.9) | 0 |
| Total GHQ | 42 (38.9) | 36 (33.3) | 30 (27.8) | 0 |
| Job burnout | 14 (13) | 32 (29.6) | 44 (40.7) | 18 (16.2) |
| Resilience | 0 | 0 | 96 (88.9) | 12 (10.1) |
The Frequency Distribution of the Severity of Variables in Nurses During the COVID-19 Outbreak a
Moreover, the results showed that there was no significant difference between men and women regarding mental health and job burnout. Also, there was no significant difference between different age groups regarding these variables (P > 0.05). Pearson’s correlation coefficients of the total GHQ score, resilience, and job burnout revealed that resilience was negatively associated with job burnout (r = -0.38) and mental health problems (r = -0.32). On the other hand, the total score of GHQ was positively associated with job burnout (r = 0.62).
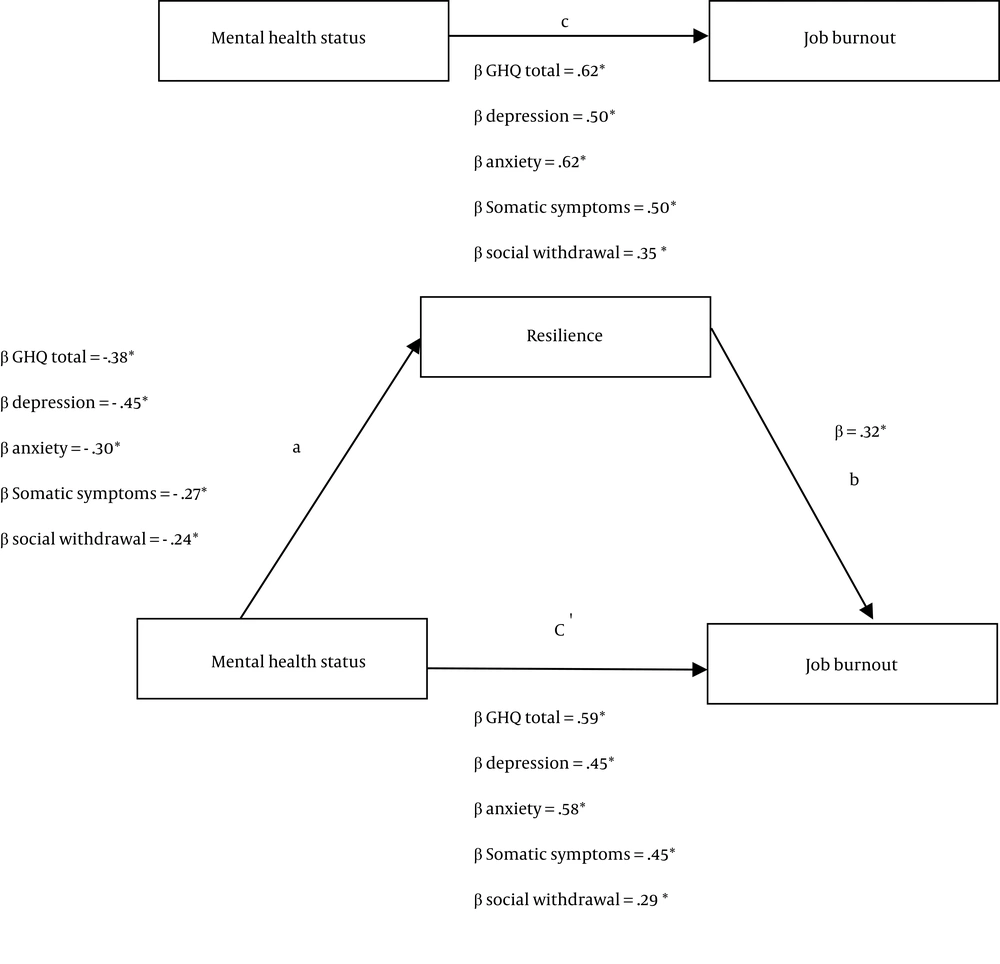
The effects of depression, anxiety, somatic symptoms, and social withdrawal on job burnout, mediated by resilience, were examined by path analysis, based on an approach proposed by Baron and Kenny (29). According to this approach, a four-step regression analysis was performed to evaluate the mediating role of resilience. In this model, (1) mental health problems should predict job burnout (path C); (2) mental health problems should predict changes in the mediator (path A); (3) changes in the mediator (resilience) should predict job burnout (path B); and (4) the effect of mental health problems on job burnout should be reduced or become insignificant after adding resilience to the model (path C). The results of this analysis are demonstrated in Tables 3 - 7.
| Model | Predictor Variable | Dependent Variable | Total R2 | F | B | SE | Beta |
|---|---|---|---|---|---|---|---|
| 1 | Total GHQ | Job burnout | 0.395 | 67.88 | 1.04 | 0.12 | 0.628* |
| 2 | Total GHQ | Resilience | 0.146* | 17.78 | -0.421 | 0.10 | -0.382* |
| 3 | Resilience | Job burnout | 0.102* | 11.82 | -0.482 | 0.14 | -0.320* |
| 4 | Resilience and total GHQ | Job burnout | 0.402* | 34.66 | -0.14; 0.98 | 0.12; 0.13 | 0.093; 0.593* |
| Model | Predictor Variable | Dependent Variable | Total R2 | F | B | SE | Beta |
|---|---|---|---|---|---|---|---|
| 1 | Depression | Job burnout | 0.254* | 35.43 | 3.35 | 0.56 | 0.504* |
| 2 | Depression | Resilience | 0.210* | 27.70 | -2.02 | 0.38 | -0.459* |
| 3 | Resilience | Job burnout | 0.102* | 11.82 | -0.482 | 0.14 | -0.320* |
| 4 | Resilience and depression | Job burnout | 0.264* | 18.47 | -0.46; 3.01 | 0.14; 0.63 | -0.20*; 0.45* |
| Model | Predictor Variable | Dependent Variable | Total R2 | F | B | SE | Beta |
|---|---|---|---|---|---|---|---|
| 1 | Anxiety | Job burnout | 0.390* | 66.44 | 2.51 | 0.30 | 0.624* |
| 2 | Anxiety | Resilience | 0.09* | 10.34 | -0.804 | 0.25 | -0.301* |
| 3 | Resilience | Job burnout | 0.102* | 11.82 | -0.482 | 0.14 | -0.320* |
| 4 | Resilience and anxiety | Job burnout | 0.409* | 35.63 | -0.21; 2.33 | 0.12; 0.32 | -0.16*; 0.581* |
| Model | Predictor Variable | Dependent Variable | Total R2 | F | B | SE | Beta |
|---|---|---|---|---|---|---|---|
| 1 | Somatic symptoms | Job burnout | 0.256* | 35.81 | 2.41 | 0.40 | 0.506* |
| 2 | Somatic symptoms | Resilience | 0.077* | 8.73 | -0.881 | 0.29 | -0.278* |
| 3 | Resilience | Job burnout | 0.102* | 11.82 | -0.482 | 0.14 | -0.320* |
| 4 | Resilience and somatic symptoms | Job burnout | 0.291* | 21.11 | -0.29; 2.15 | 0.13; 0.41 | -0.194*; 0.542* |
| Model | Predictor Variable | Dependent Variable | Total R2 | F | B | SE | Beta |
|---|---|---|---|---|---|---|---|
| 1 | Social withdrawal | Job burnout | 0.125* | 14.85 | 3.00 | 0.77 | 0.353* |
| 2 | Social withdrawal | Resilience | 0.058* | 6.34 | -1.35 | 0.53 | -0.240* |
| 3 | Resilience | Job burnout | 0.102* | 11.82 | -0.482 | 0.14 | -0.320* |
| 4 | Resilience and social withdrawal | Job burnout | 0.183* | 11.56 | -0.37; 2.49 | 0.13; 0.77 | -0.249*; 0.294* |
As shown in Figure 1, by adding resilience to the regression model, the β-coefficients of all variables decreased. The Sobel test showed that resilience had a significant mediating effect on the relationship between mental health problems and job burnout (Z = -3.18 and P < 0.001 for total GHQ; Z = 2.88 and P < 0.003 for depression; Z = 2.33 and P < 0.01 for anxiety; Z = 2.27 and P = 0.02 for somatic symptoms; and Z = 2.04 and P < 0.05 for social withdrawal). These results indicated that resilience partially mediated the effect of mental health problems on job burnout.
5. Discussion
Healthcare workers are at the frontline in the fight against COVID-19, and among all occupational groups, they are bearing the greatest burden due to this global health emergency. Although these professionals are generally exposed to high risks of stress, job burnout, and suicide, given the occupational pressure associated with their career, the recent pandemic has caused even more stress in this group (30). The current study was carried out in two general hospitals of Kashan city and Aran-o-Bidgol county, as the main centers for COVID-19 treatment, to examine the mental health problems and burnout of nurses during this outbreak.
In the current study, the most common psychological symptoms of nurses were mild social withdrawal and somatic symptoms (60.2 and 44.4%, respectively). The present findings were consistent with the results of a systematic review on the mental health status of healthcare workers during the COVID-19 pandemic, which showed that despite the use of different scales and cut-off values in each study, the majority of healthcare workers experienced mild symptoms; however, moderate and severe symptoms were less common among the participants (31).
The rate of depression among nurses in the present study was noticeable, and most of the participants did not report any depression symptoms (85.2%). Only 13% of the participants reported mild depression, which is lower than the rate reported in other studies. In this regard, a systematic review of the prevalence of psychological symptoms in healthcare workers showed that the prevalence of depression was 22.8% (32). Moreover, in a study by Lu et al., the rate of mild depression in nurses (n = 764) was 38.1%, based on the Patient Health Questionnaire (PHQ-9), and the prevalence of moderate and severe depression was 8.4 and 7.1%, respectively.
On the other hand, in another study on the medical staff (n = 2042), the results were consistent with our findings. In this study, based on the Hamilton depression scale, 87.9% of nurses reported no depression symptoms, 11.8% reported mild to moderate symptoms, and 0.3% experienced severe symptoms (33). Generally, work-related stressors, such as long working hours, high workload, sleep deprivation, and the challenging and changing nature of healthcare workers’ job predispose them to depression; therefore, the impact of the current health crisis on the mental health status of this group is prominent. Healthcare workers are influenced by various factors, such as worry and concerns about the risk of transmitting the virus to family members, increased demands and work pressure, social isolation, and exposure to the patients’ trauma reactions due to invasive treatments, such as intubation (34).
In different studies, having access to personal protective equipment has been introduced as a factor that consistently decreases the risk of adverse psychological outcomes in healthcare workers. Kashan was one of the first counties to be extremely affected by COVID-19, and the healthcare workers experienced immense pressure, especially due to unforeseen conditions that negatively affected the protective factors. Therefore, the lower rate of depression in Iranian nurses might be attributed to other factors. One explanation can be the use of different tools in different studies for mental health assessment. Another explanation is related to cultural factors. Since Kashan is a religious and traditional province in Iran, the observed differences might be related to the beliefs of nurses; however, further studies are needed to investigate this claim.
On the other hand, social support has positive effects on the mental health status and self-efficacy of individuals. Social interactions reduce negative emotions and improve one’s mood. Overall, having a large social network can help the medical staff to perceive stressful events as less threatening and may decrease physiological responses and dysfunctional behaviors that result from stress. Besides, social support increases self-efficacy, which in turn leads to more encouragement, courage, and sense of professionalism. The increase in self-confidence may help the medical staff to be more optimistic and accelerate their coping with pressure. During the COVID-19 pandemic, Kashan University of Medical Sciences formed different support groups to inform and appreciate the efforts of healthcare staff, as such activities can positively influence the mental health of the staff. Overall, it seems that in Kashan, the nurses’ reaction to this crisis mostly involved somatic symptoms and social withdrawal; however, further research is needed to identify the protective factors during crises.
In terms of job burnout, the results showed that most of the participants experienced moderate job burnout. This finding is consistent with previous research on the medical staff (16, 17). Generally, burnout can be caused by the persistence of job pressure that an individual cannot successfully manage. It seems that medical staff, due to exposure to high work pressure and patient mortality (13), long work shifts (17), and the need to make quick decisions in emergencies, are at a higher risk of burnout (10). Since all of these factors have been present during the COVID-19 outbreak, nursing burnout is highly predictable.
Our findings revealed no significant gender or age differences in the study variables, which is inconsistent with other studies, reporting higher rates of anxiety and depression in female healthcare workers than males (35, 36); this finding may be related to significant differences in the sample size of men and women in the current study. As reported earlier, most of the participants were female in our study; therefore, the results may be confined by the predominant female sample of the study.
This cross-sectional study revealed that individuals with higher resilience had fewer problems in terms of mental health and burnout. Besides, a mediation analysis was performed to determine whether resilience mediated the association between mental health and job burnout in healthcare workers. The results showed that resilience had a significant mediating role in the relationship between mental health problems and job burnout among healthcare workers during the COVID-19 pandemic. Our findings indicated a significant indirect mediator through which higher resilience was associated with lower levels of job burnout. However, it is important to note that this indirect mediator was analyzed in a cross-sectional, correlational study and could not be interpreted casually.
Resilience was found to be a partial mediator. Therefore, there are other variables, such as job satisfaction, social support, spiritual health, and religious beliefs, which can explain the association between mental health and job burnout. These results are consistent with previous studies, which investigated the relationship between resilience and stress, well-being, psychological distress, and mental health problems. Evidence suggests that healthcare workers with higher levels of resilience show lower levels of mental health problems (37-39). Although the sample size of these studies was small, the association between resilience and better mental health was consistent. Another study which investigated the effects of resilience on stress and job functionality in difficult work environments applied an online survey-based tool to assess healthcare workers. The results revealed that resilience had a protective effect on stress, burnout, job satisfaction, intention to quit, probability of absenteeism, low functionality, sleep problems, and likelihood of depression (40).
The COVID-19 outbreak and the resulting social isolation have increased the levels of anxiety and depression. As mentioned earlier, the healthcare staff, who work under high pressure, may face various difficulties, which negatively affect their mental health and well-being. Also, their resilience may be affected by isolation and loss of social support, as well as vigorous and unforeseen changes in the work environment (41). Psychological resilience is generally crucial for the healthcare staff, who face various risk factors during the COVID-19 pandemic and are responsible for providing healthcare services to patients. It consists of three components, including self-commitment, control, and challenges. Self-commitment refers to being purposeful and having active participation in daily events and activities. Control refers to the belief that one can deal with various challenging situations rather than being negatively affected by them. Finally, challenge is the expression of one's belief in change (42). These characteristics may enable the healthcare staff to cope more effectively with challenging situations during the COVID-19 outbreak.
There were some limitations in this study. First, since the study population only included nurses working in Kashan hospitals, the external validity of the findings was limited, and the results cannot be generalized to more diverse healthcare populations; further research is needed with a more diverse sample of healthcare workers. Second, considering the self-survey nature of this study, the participants’ responses could have been influenced by factors, such as social desirability, incorrect memory recollection, and inaccurate reporting; therefore, use of more objective behavioral assessments can be beneficial.
5.1. Conclusion
The present results had some implications for assessing and improving the psychological health of nurses. Our findings revealed that resilience was related to higher mental health and lower job burnout; accordingly, evaluation of one’s resilience resources and traits may be helpful in predicting individuals at risk of psychological problems and job burnout. Overall, resilience is critical to protecting healthcare workers against the COVID-19 pandemic, and the importance of interventional approaches that focus on increasing flexibility to improve well-being has been highlighted. Overall, cognitive, emotional, and interpersonal skills can be developed by organizations and mental health professionals to promote adaptive coping responses.