1. Background
Suicide is the third leading cause of death among people between 15 and 24 and the 10th leading cause of death among all ages (1). According to the World Health Organization (WHO), the global age-standardized suicide rate was 11.4 per 100,000 person-years in 2012 (2). The reported rates of suicide in Iran are variable in different studies, partly because of inaccurate records of suicide. However, the average suicide rate in Iran is estimated to be 6.67 per 100,000 (3). Moreover, suicide is the fifth cause of all deaths in Iran (4).
Despite all efforts, suicide is one of the most important concerns in public health, while suicide prevention measures are among the biggest challenges for health systems. Several studies have shown that most people victims of suicide saw at least a healthcare professional, such as a general practitioner or psychiatrist, during the last few weeks or months before suicide death (5).
There are several suicide prevention strategies with some beneficial outcomes. In a systematic review of interventions for suicide prevention, the following interventions were studied: Screening, public and physician education, psychological crisis intervention, media strategies, restricting access to suicide means, and hotline support. Among these strategies, not a single measure fared better than the others, and the authors suggest a combination of these evidence-based strategies (6).
For many patients at high suicide risk, psychiatric admission and intensive monitoring in psychiatric wards are necessary. However, this poses challenges in most low and middle-income countries with insufficient inpatient beds and the limited capacity of psychiatric hospitals for admitting new patients. For example, the inpatient bed occupancy in our center (Roozbeh Hospital), a major referral hospital in the capital city of Iran, is close to 100% almost every day. As a referral hospital with many caseloads, it could admit less than half of the patients who need admission. Therefore, effective outpatient services are needed to abort the crisis and prevent suicide attempts or commitments.
There is much evidence of the efficacy of brief acute interventions for suicide prevention (7). One successful strategy is crisis intervention services with follow-ups. In a study by Fleischmann et al. in five low and middle-income countries, brief intervention and contact, which included patient education and follow-up, was significantly associated with fewer deaths (8). Telephone follow-ups in several other studies could reduce the suicide rate (9-11). At a more comprehensive level, case management can also reduce the risk of suicide, at least for the short term (12, 13). Thornicroft defines case management as the "coordination, integration, and allocation of individualized care within limited resources," which includes ongoing contact with one or more identified key personnel (14). An important barrier in suicide risk management, especially in low- and middle-income countries, is the psychiatric bed shortage. Hence, services based on case management could provide a solution. There is a paucity of data regarding the strengths and weaknesses of an outpatient service based on case management for suicide prevention.
Nevertheless, because of the complexity and multi-aspect nature of suicide, barriers to receiving mental health services, and social and other support resources, we need to develop comprehensive, yet less resource-demanding, services that contain different aspects of care.
2. Objectives
We aimed to develop (phase 1) and investigate the short-term outcomes of piloting an outpatient psychiatric crisis intervention service enhanced with case management for patients with suicide risk where hospital admission was impossible because of the bed shortage (phase 2). Indeed, this is a preliminary study of the service.
3. Methods
3.1. Service Development (Phase 1)
In the first phase of this study, we did a comprehensive review of the literature to seek available evidence-based interventions for patients with high suicide risk. Then, we discussed the findings in several meetings at the Division of Community Psychiatry at Roozbeh Hospital, where the various aspects of the intended service design were explored. We also conducted a quick qualitative and quantitative situation analysis of the emergency department at the hospital, which included an evaluation of the rates of any psychiatry visits per day to the ED, the proportion of visits associated with suicidality to all visits, and the rate of hospitalization of patients with suicide risk, as well as individual interviews with the stakeholders at the ED and the hospital. Then, considering the dimensions of equity, cost-effectiveness, availability, and accessibility of the existing interventions, we chose a broad multi-component intervention model and tailored it to our patient's needs and the context of the service provision. The developed service was entitled the "psychiatric crisis intervention" (PCI or MODABBER as a Persian acronym).
From the outset and during the development phase, we engaged several stakeholders, including the hospital's head and manager, the head of the emergency department, and the legal advisor of the hospital. The expert panel comprised these persons and the study's authors. We held several meetings and discussed the situation analysis findings, the literature review findings, and administrative issues, including barriers to implementation and how they can be resolved.
3.2. Service Description
During the development phase, we concluded that employing a psychological crisis intervention enhanced by a case management approach and psychiatric consultations has a sufficient evidence base and can be employed for our patients who need hospital admissions but are deprived of any services because of a lack of available beds. Currently, patients with psychiatric problems that visit the emergency ward at the hospital are visited by a junior psychiatry resident, and in case of high or moderate suicide risk (based on the clinical judgment), they may need to be admitted. However, our situation analysis noted that these patients are usually deprived of appropriate care because of the limited capacity for immediate hospital admissions.
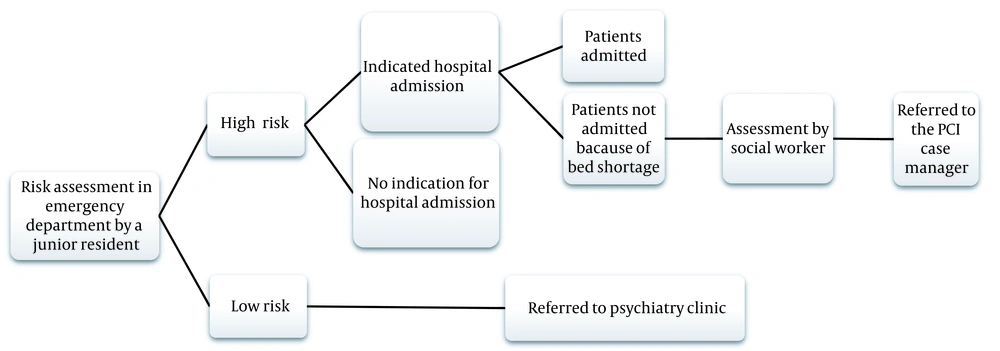
In case of unavailability of hospital beds and if the patient meets the PCI's admission criteria (Box 1), the intervention is offered. The flow of the patients to receive the PCI is shown in Figure 1. The PCI aimed to fill the gap between psychiatric emergency visits and admission. Based on our situation analysis findings, for nearly half of the patients that indicated psychiatric admission, hospitalization was not possible immediately, and they had to wait for a psychiatric bed, which usually lasted one to five days.
| Criteria |
|---|
| Admission criteria |
| High or moderate risk of suicide that mandates a hospital admission |
| Admission is not possible because of full bed occupancy at the hospital |
| Age > 18 years |
| Patient and his/her caregivers/relatives are cooperative to make sure outpatient care/follow-up is possible |
| Low risk of severe violence/aggression |
| Consent to receive the service |
| Discharge criteria |
| Inpatient admission |
| Suicide risk resolution (low suicide risk for at least two successive visits) |
| Withdrawal of the consent to continue the PCI service by the patient and/or his/her caregiver/relative |
| Death or serious medical condition that needs hospital care |
Abbreviation: PCI, psychiatric crisis intervention.
It must be emphasized that this service is not an alternative to psychiatric hospitalization; indeed, the PCI tries to provide the best available care for patients with suicide risk. In this regard, the patient is referred to a psychologist who works both as a psychological crisis intervention provider and a case manager, and the care and follow-ups are provided by her/him. Usually, on the same day, patients are visited by a senior psychiatry resident for further treatment planning and pharmacological management under the supervision of a faculty member in the Hospital's psychiatric outpatient clinic. Case managers are responsible for assessing each patient's needs and trying to meet these needs through the facilitation of pharmacological, psychological, and social interventions. Therefore, case managers establish contact with patients and caregivers/family relatives, provide essential psychoeducation considering the patient's conditions, and encourage them to look for psychiatry beds in other hospitals. Psychoeducation includes information for caregivers/family relatives on reducing suicide risk, for example, not leaving the patient alone at home, monitoring the use of drugs, and keeping dangerous objects away. Moreover, she/he arranges for any necessary psychological and psychiatric visits and follows the patients to ensure their attendance at the visits, while active follow-up measures will be considered, usually including repeated telephone calls. In the case of psychological intervention, the case manager employs Robert's seven-stage crisis intervention protocol (15).
Our staff included three psychiatry residents, three psychologists, and three social workers. The treatment procedure of each patient in PCI service is handled by the same psychologist, psychiatry resident, and social worker until discharge from the service. Disagreement between social workers, psychologists, and psychiatry residents is discussed and resolved in weekly meetings. This service is offered until the risk of suicide is resolved or admission becomes possible. It should be noted that before the case manager visits, a social worker informs the patient and his/her family about the PCI and assesses whether the patient possesses enough social support for outpatient care.
The patient is visited at least once a week for pharmacological interventions by a psychiatry resident, and crisis intervention sessions are offered by the psychologist (case manager) in the hospital's psychiatric outpatient clinic multiple times a week (even daily). The patient is discharged from the PCI if meeting at least one of the discharge criteria described in Box 1. One discharge criterion is low suicide risk in two consecutive visits, based on residents' clinical judgment made following reviewing records and conducting a separate interview. Patients discharged from the crisis intervention are referred to the conventional outpatient clinic.
A faculty member of the Hospital holds weekly staff meetings. In this way, we ensured the quality of the clinical and social service provisions.
3.3. Piot Implementation and Evaluation of the Service (Phase 2)
Following the development of the intervention, we trained the service providers by holding a six-hour crisis intervention workshop based on Robert's seven-stage crisis intervention model (15). The training was ongoing through supervision meetings of the care providers held by a faculty member, which employed a coaching and mentoring approach.
This study was carried out using an action research design and methodology. We developed and implemented the intervention and assessed the preliminary outcomes for the first two months after the development of the PCI. The study outcomes included patient recruitment rate, patient satisfaction, patient adherence to appointments (and dropout), crisis resolution rate, suicide attempts, and deaths during the two-month follow-up period (Table 1). Research assistants called patients and their caregivers/family relatives to evaluate the outcomes. The assistants were not among the care providers of those individuals. Informed consent was obtained from patients and their caregivers/relatives. Ethical permission was received from the Ethics Committee of Tehran University of Medical Sciences (TUMS) with the code of IR.TUMS.MEDICINE.REC.1398.498.
| Outcome | Definition |
|---|---|
| Patient recruitment | The number and the proportion of patients who were included relative to all those that met the admission criteria and needed the service during the study period |
| Patient satisfaction | The number and proportion of the patients who reported a high or a very high satisfaction in the client satisfaction questionnaire on a Likert scale two months after admission to the PCI |
| Suicide attempts | The number and proportion of patients who reported an attempted suicide within two months after admission to the PCI |
| Death due to suicide | The number and proportion of patients who attempted suicide and died within two months after admission to the PCI |
| Adherence to the appointments (and dropouts) | The number and proportion of the patients who attended (or did not attend) all the scheduled intervention sessions during the two months after admission to the PCI |
| Crisis resolution | The number and proportion of patients whose need for hospitalization because of suicide risk was resolved at least in two consecutive visits based on the clinical judgment during the two months after the admission to the PCI |
Abbreviation: PCI, psychiatric crisis intervention.
4. Results
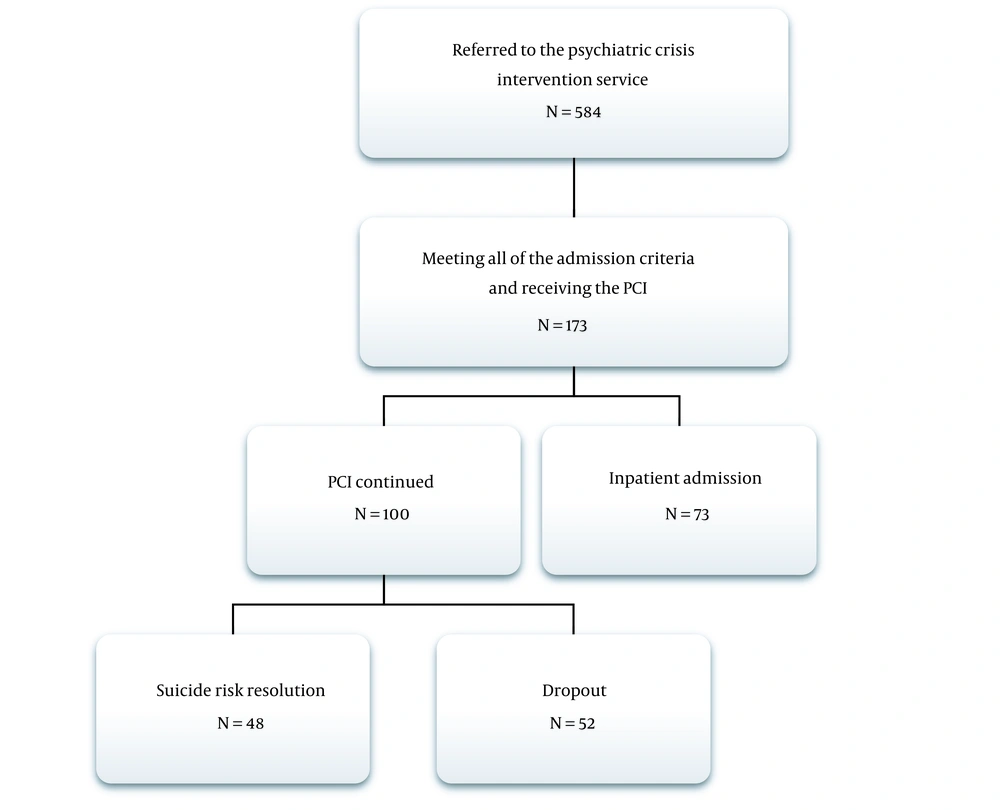
The pilot phase of the PCI implementation began in January 2019 and lasted 12 months. The total number of patients referred to the PCI during this phase was 584, of whom only 173 (29.6%) had the requirements of admission criteria (the recruitment rate). This rate could show the acceptability of the service. The reason for most of those who did not enroll was negative patients' or family attitudes towards outpatient care and preference for hospitalization.
Among these 173 patients (including 100 males and 73 females), the suicide risk resolved in 48 (27.7%), and they were successfully referred to a psychiatry clinic for long-term treatment (Figure 2). This group consisted of 19 males and 29 females. It should be noted that after this period, the suicide risk was resolved, and the patient did not need hospitalization and active care anymore. It did not mean the patient was in full remission, and the rest of the treatment should be continued in the outpatient clinic. The crisis resolution happened in seven intervention sessions or less for all of them. On average, for patients whose suicide risk was resolved, the number of psychological crisis intervention sessions was 3.2, and the number of psychiatric visits was 3.5. As said, the crisis resolution was defined as "suicide risk being reduced at least in two consecutive visits based on the clinical judgment." This outcome was achieved in sessions 2 to 7 if the patient was not admitted. Therefore, the number of sessions could be attributed to several factors, including the severity of the illness, treatment adherence, treatment response, and bed availability, among others.
Fifty-two (30.1%) patients dropped out of the service (36 males and 16 females). From patients' and their families' points of view, the reasons for dropout included the following: Distance from the hospital, which made it difficult to attend the intervention sessions, resolution of psychiatric symptoms and suicidal ideation, financial problems, and seeking another psychiatric service such as a private psychiatrist or other psychiatric hospitals. The rest (73 patients, 42.2%) were admitted to the hospital after receiving at least one crisis intervention session. This group included 45 males and 28 females. If the patient's suicide risk persisted and a psychiatric bed became available, the patient was admitted at any time during treatment. Nevertheless, if hospitalization was impossible because of the bed shortage, the service was offered until the resolution of the suicide risk, and the patient was discharged from the service. In total, 296 crisis intervention sessions and 272 psychiatric visits were offered to these patients. The maximum number of crisis intervention visits was seven sessions, in which the crisis was resolved for those who did not drop out of the service.
After two months of admission to the PCI, in a convenience sample of 50 persons who could be reached, the satisfaction of patients and their caregivers/relatives was assessed through telephone calls. This assessment was performed for all three groups of patients (persons with crisis resolution, dropped-out patients, and patients who were finally admitted). It should be emphasized that we tried to fill the gap between ED visits and psychiatric admission. Therefore, patients admitted to the psychiatric ward also received PCI care from the ED visit to admission; therefore, we should have included them in the satisfaction assessment and inquired about their satisfaction with the PCI service. The overall satisfaction was very good or good for 43 (86%, 95% CI = 76.4 - 95.6%). During the two-month follow-up, only one patient attempted suicide. It should be noted that this patient was not adherent to the PCI and had already dropped out of the service. No death by suicide was reported.
5. Discussion
The PCI in our study included three important components: (1) psychological crisis intervention; (2) case management with active and assertive follow-up; and (3) psychiatric consultations. Some specific psychological interventions can reduce the rate of suicide attempts (16, 17). Psychological crisis intervention has become the most widely used time-limited treatment modality (18), and problem-solving, an important component of crisis intervention, could decrease suicide attempts (19, 20).
Case management services have recently been studied for patients with suicide risks. Kim et al. in Korea evaluated the long and short-term effects of case management on suicide prevention; in this study, case managers provided weekly interviews in a four-week case management service. In the long term, they found no difference in the time to suicide re-attempt between the control group and individuals receiving case management service (21). However, unlike our study, the case manager was a social worker, and the service did not include any psychological crisis intervention or psychiatric consultation.
Other programs incorporate some crisis resolution interventions, follow-ups, and case management services. Crisis resolution and treatment groups in the home have been introduced in England. They aim to evaluate all patients considered for acute hospitalization (including those with suicide risk) to offer intensive home treatment rather than hospital admission if possible. The main features included 24-hour accessibility, intensive contact, and case management in the community, with visits twice daily if needed (22). Internationally, the most extensive implementation of crisis resolution home treatment teams (CRT) has been in the UK. These teams provide a hospital-at-home service for acute episodes of mental disorders. Furthermore, most CRT teams also provide gate-keeping functions for admissions into psychiatric services and facilitate early discharge into the community (23).
In Australia, the northern crisis assessment and treatment team (NCATT) provides multidisciplinary 24-hour community assessment and treatment of psychiatry emergencies. The patients can ring at any time. For admission, all agencies (except NAMHS rehabilitation services) must first refer to NCATT. In this service, if the patient is planning to receive outpatient care, he/she can be visited up to twice daily (24). Also, a study in Australia comparing the efficacy of intensive case management with usual treatment for suicide attempters following discharge from psychiatric care revealed that this service could reduce the risk of suicide re-attempt. Like our study, in this service, there was a high dropout rate (25).
In Japan, through the ACTION-J study, the effectiveness of an assertive case management service has been evaluated to prevent suicide re-attempts. In this approach, the case manager facilitates the care of the patient after an attempt by periodic contact, collection of information about the patient's status, psychological education, collaboration with psychiatrists and primary care physicians, referrals for outpatient treatment, coordination of the use of social resources, and usage of internet-based services (26, 27). This study showed that case management services following emergency admission for a suicide attempt could reduce the rate of repeat self-harm (13). In this study, contrary to our service, patients had been visited on a fixed schedule. In our PCI service, the frequency of contact was variable (at least one visit weekly) based on the patient's condition and the clinician's clinical judgment.
Morthorst et al. applied an alternative case management model for suicide attempters. The intervention was provided as case management with crisis intervention, problem-solving, motivational support, and actively assisting patients to and from scheduled appointments. The trial found no significant difference between the group receiving the intervention and the group receiving treatment as usual in suicide repetition rates (28).
Chen et al. in Taiwan evaluated the effectiveness of case management in preventing suicide re-attempts. In their study, a case manager, mainly a psychiatric nurse, coordinated the services. Their study showed that case management service appears to be effective in preventing suicide repetition (12). In this service, case management is principally done via telephone conversations and home visits as a secondary option.
The Brimblecombe et al. study that evaluated home treatment as an alternative to hospitalization found that 21% were admitted to the hospital before home treatment was finished. Notably, 'risk to self' was the most common reason for hospitalization (29). Alba Pale et al. in Barcelona designed home treatment and crisis intervention as an alternative approach to hospitalization. They found home treatment was an alternative to hospital admission (30). As seen in these studies, home care could be an important part of the case management service, but it was impossible in our study because of a lack of resources.
In Iran, Malakouti et al. established a charge-free "Suicide Prevention Consultation Office" (SPCO) for persons with suicide attempts, patients with depressive disorders, and any individuals at risk of suicide. The main task was to make immediate contact with suicide attempters at Emergency Department and provide five consultation sessions and educational brochures to the patients and their families. The intervention phase included the treatment process in primary health care and education for general practitioners; these interventions were done for one year and showed some reductions in suicide risk (31). Furthermore, active telephone follow-up and case management can markedly reduce the risk of suicide re-attempt (9, 32, 33). In our model, a close follow-up that occurs through both psychiatry visits and telephone contacts can be associated with increased patient adherence to PCI and perhaps reduced suicide thoughts and attempts.
As noted above, our discharge criteria included a lowered risk for suicide in two consecutive visits. Resolving the risk of suicide in our study implies that patients had low suicide risk in two consecutive visits, based on clinical interview and risk assessment according to a physician's clinical judgment. After discharge from our service, patients were referred to the conventional outpatient service for continuity of care.
We have realized that a significant proportion of patients who were considered dropped-out experienced resolved suicidal risk, but since they did not attend two consecutive sessions, we included them as dropped-out subjects.
There are barriers to the implementation and sustainability of novel programs, especially in low-resource settings, which may include, among many others, inadequate financial resources to cover the expenses and wages of the service providers, the challenges of the integration of a new program into the existing services, and the attitudes of the other hospital's staff and patients/families.
The study's major limitations included the lack of a control group and the short follow-up period. Also, satisfaction was assessed in a convenience sample of reachable persons, which could not represent all participants. Moreover, it would be much better to assess patients' satisfaction with more reliable methods and obtain the opinion of different stakeholders. Another limitation was difficulties working with suicidal patients, influencing the decision-making process and limiting the researchers' ability to control the setting or define or measure the outcomes.
5.1. Conclusions
Taken together, we can argue that the suicide risk and the need for hospitalization were resolved for many patients who otherwise needed hospital care. A randomized controlled trial is mandated to ascertain the efficacy of this service compared with the existing services.
In the future, we would revise our service based on the findings of the current pilot study and conduct more studies employing a controlled design, such as a formal implementation-effectiveness study, to assess the outcomes and effectiveness of the PCI. If effective, we can think of expanding the coverage of the PCI to include pediatric patients, self-mutilation with no or low risk for suicide, traumatic crises such as physical and sexual abuse, and domestic violence. It is important to draft guidelines to define appropriate candidates for PCI and describe the most appropriate interventions.