1. Background
Coronavirus disease 2019 (COVID-19) has spread exponentially across all continents over several months (1). Due to high mortality and infection, COVID-19 can lead to numerous psychological problems, including depression, fear, stress, anxiety (2), and possibly burnout. Recent research has shown that people in quarantine experience a variety of psychological problems such as stress, fear, and failure (3). So far, there is uncertainty about when and how the pandemic might continue despite the facilities and ease of COVID-19 measures, including wearing a face mask in public places and maintaining social distance (4).
Therefore, the uncertainty associated with COVID-19 and the length of time we should stay home can make a considerable difference in our daily lives. Such alters in daily life caused by COVID-19 can increase the levels of stress, anxiety, burnout, fear, and failure (2, 5). Stressful living conditions have notable adverse effects on psychological functioning and mental health and lead to mental problems such as social deprivation, mental confusion, anxiety, and depression (2). Extreme stress can lead to a broad range of psychological and psychosocial problems, including emotional disorders, burnout, and anxiety. Understanding how people react in stressful situations such as COVID-19 pandemic can be helpful in creating and developing interventions (6).
On a broader level, burnout has been found to be associated with a wide range of mental health problems and well-being indicators, such as increased anxiety, memory impairment, alcohol consumption, depression, sleep problems, and neck and back pain (7). Burnout is defined as a state of extreme fatigue that results from hard, unmotivated, and uninteresting work. In one study, 14.9% of students had burnout syndrome, and 57.7% were at risk for this syndrome (8). COVID-19 burnout studies have been performed primarily on health care professionals. The study of health care professionals showed a positive and significant relationship between stress and burnout (9). Another research examining the relation between stress disorders, anxiety, and burnout during the COVID-19 pandemic found that physicians and nurses experienced psychological problems, including burnout (10).
Maintaining positive mental health is just as important as physical health in the event of a COVID-19 pandemic. In this regard, evaluating the effect of COVID-19 on the mental health of individuals is an important topic for research during the pandemic. To achieve this goal, there is a need for valid and reliable epidemiological assessment tools. Because of the long duration of the COVID-19 pandemic, people might greatly suffer from the common burnout caused by the disease. However, no scale is available that directly indicates the experience of burnout during this pandemic. Hence, unlike the previous scale developed by Talaee et al. (5), there is a need for a scale that can be easily applied to the general populations.
In order to expand research on COVID-19 and evaluate its psychological consequences, such as burnout, it is important to have reliable and valid instruments to measure it. The present study can help increase knowledge about the cultural effects of burnout caused by COVID-19. Also, standardizing the COVID-19 Burnout Scale (COVID-19-BS) in societies with different cultures can contribute to its external validity (11, 12).
2. Objectives
Considering the psychological consequences of COVID-19, the present study was conducted to investigate the psychometric properties of the Persian version of the COVID-19-BS.
3. Methods
3.1. Subjects and Methods
The population of this descriptive (psychometric) study included all students of Ahvaz Jundishapur University of Medical Sciences, Iran, from October 2020 to November 2020. Using the convenience sampling method, 251 students were selected. According to the minimum sample size in the confirmatory factor analysis (CFA) based on Kline (13), which is 200 people, 251 people were selected.
The inclusion criteria were willingness to participate in the study and being at least 18 years old. Due to the COVID-19 pandemic, data collection was done using online social networks, including WhatsApp and Telegram. During the research, in case of any event that violated the continuation of the research, the cooperation with the volunteer was terminated. Also, the participants were free to withdraw from the study at any stage. Participation in the study was completely free, and participants did not pay any fees.
The COVID-19-BS was developed based on instructions and guidelines for cross-cultural adaptation of instruments (14). Initially, the original version of the COVID-19-BS was translated from English into Persian by four PhD students in clinical psychology. Any differences in translations were resolved by agreement. In the next step, the translated Persian version was translated into English by two fluent mental health specialists in both English and Persian. The final translation of the COVID-19-BS was reviewed by the authors. Then, in a pilot study, the COVID-19-BS was performed on 22 students of Ahvaz Jundishapur University of Medical Sciences, and the existing problems were corrected. Finally, the scale was used to evaluate all samples. In the pilot study, students did not report any problems, and Cronbach’s alpha was 0.73 on a population of 22.
3.2. Ethical Consideration
This study was approved by the Ethics Committees of Ahvaz Jundishapur University of Medical Sciences (IR.AJUMS.REC.1399.897).
3.3. Measures
3.3.1. The COVID-19 Anxiety Syndrome Scale
A short tools for reliably identifying the characteristics of COVID-19-related anxiety syndrome. This scale has nine items that measure two dimensions, including perseveration Anxiety Syndrome Scale (C-19ASS-P) and avoidance (C-19ASS-A). Participants respond to each statement on a five-point Likert scale from one (not at all) to 5 (nearly every day) (15). Cronbach’s alpha was for the perseveration dimension was 0.86, and for the avoidance dimension was 0.77 (15).
3.3.2. The COVID-19 Burnout Scale
This scale consists of ten items and is adapted from the short version of Malach-Pines burnout (16). Each item is graded on a five-point Likert from 1 (never) to 5 (always). The total score can be calculated by adding ten items, and scores are from 10 to 50. A higher score demonstrates a higher level of burnout associated with COVID-19. The scale also has a very high internal consistency and has good psychometric properties (4).
3.3.3. The Compassion Scale
This scale is a 16-item scale that measures compassion for others and is based on the Neff model of compassion for oneself. It measures the four dimensions of mindfulness, a sense of common humanity, kindness, and lessened indifference. This scale has very desirable psychometric properties (reliability, convergent validity, structural validity, and internal consistency) (17). Cronbach’s alpha for this scale obtained in various studies was between 0.86 to 0.89 (17).
3.4. Statistical Analysis
Data were analyzed using SPSS version 25. For reliability, COVID-19-BS was evaluated using internal consistency by calculating Cronbach’s alpha coefficient. Cronbach’s alpha above 0.70 indicates good internal consistency (18). The validity of COVID-19-BS scale was evaluated using two methods of CFA and convergent and divergent validity. CFA was used to assess the validity of the COVID-19-BS structure. The one-factor structure of COVID-19-BS was tested as proposed in the original version using LISREL software (8.5). Parameters and fit indices of the model were estimated through the maximum likelihood model. The fit indices of COVID-19-BS were estimated using a number of indicators including chi-square statistic (χ2), comparative fit index (CFI), standardized root mean square residual (SRMR), non-normed fit index (NNFI), root mean square error of approximation (RMSEA), and adjusted goodness of fit index (AGFI). Model fit indices are assumed to be good if AGFI ≥ .90, NNFI ≥ .90, CFI ≥ .90, SRMR ≤ .10, and RMSEA ≤ .08 (19).
4. Results
4.1. Description of the Samples
The age range of participants was 18 - 56 years, with a mean and standard deviation of 27.52 ± 4.87. Of these, 146 (58.16%) were single, 99 (39.4%) were married, and six (2.4%) were divorced. Also, 79 (31.47%) students held a PhD, 107 (42.62%) a BSc, and 65 (25.9%) an MSc degree. The mean and standard deviation of the COVID-19-BS were 28.44 and 5.17, respectively.
4.2. Confirmatory Factor Analysis
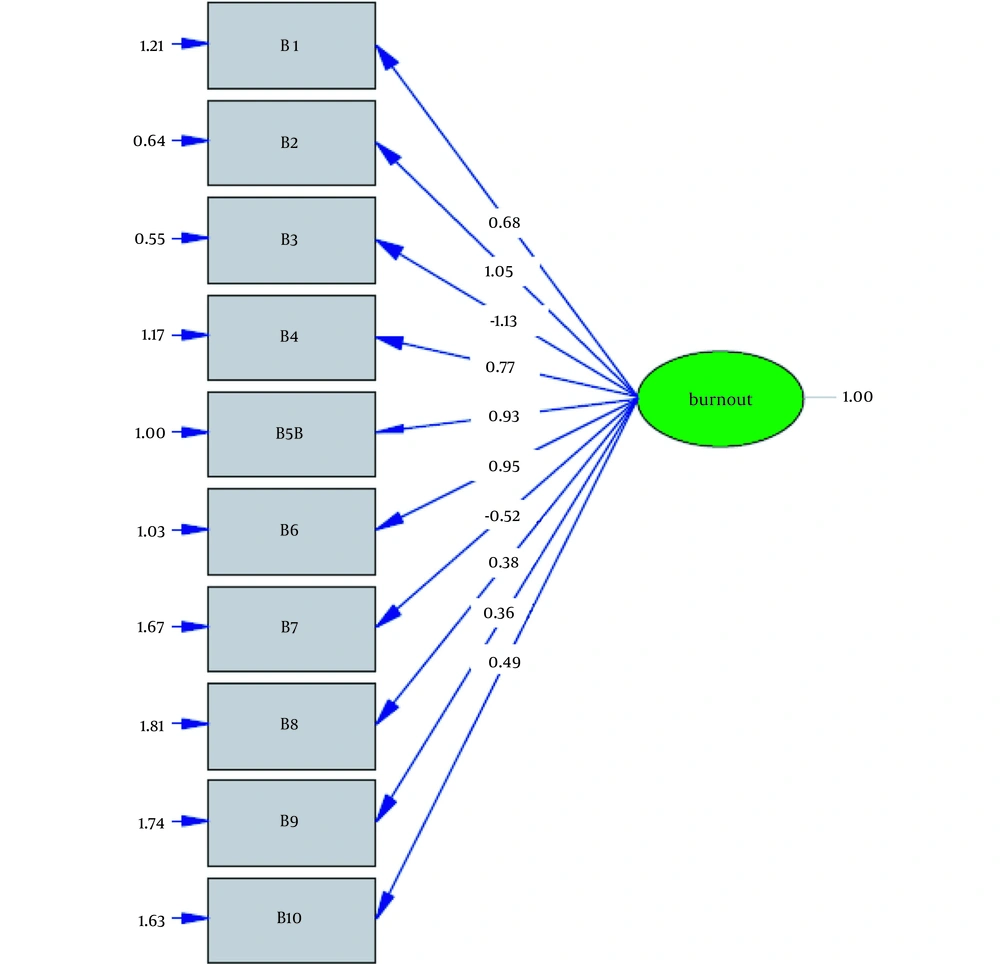
To evaluate the construct validity of the COVID-19-BS and determine the fit of the factor and subscales structure obtained from Yıldırım and Solmaz (4), CFA was performed. Based on the results of Table 1, the one-factor model of the COVID-19-BS had a good fit. Therefore, the results of the present study showed that the one-factor model had a good fit (Figure 1).
| Fit Indices | χ2 | df | P-Value | χ2/df | RMSEA | IFI | CFI | SRMR | NNFI | NFI | GFI | AGFI |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| One-factor | 150.29 | 35 | 0.000 | 4.29 | 0.08 | 0.91 | 0.91 | 0.08 | 0.89 | 0.90 | 0.89 | 0.83 |
4.3. Convergent and Divergent Validity of the COVID-19-BS
As can be seen in Table 2, the relationship between the COVID-19-BS and the CS is negative, indicating divergent validity of the scale (P < 0.01). On the other hand, the relationship between the COVID-19-BS and C-19ASS is positive, which indicates the convergent validity of this scale.
4.4. Reliability
Internal consistency obtained by Cronbach’s alpha method for the total score of C-19ASS was 0.72, which indicated a good internal consistency.
5. Discussion
COVID-19 has led to an increase in mental health problems, including psychological distress, anxiety, depression, post-traumatic stress disorder (PTSD), insomnia, fear, stress, and anger (20-22). Stress and anxiety can weaken the immune system and make them vulnerable to diseases such as COVID-19. The COVID-19-BS scale is a useful tool to understand the COVID-19 burnout.
The aim of this study was to investigate the psychometric properties of COVID-19-BS. In this study, psychometric properties (validity and reliability) of the Persian version of COVID-19-BS were studied on 251 students of Ahvaz Jundishapur University of Medical Sciences. The results showed that one-factor structure is confirmed in Iranian society. These results are consistent with the study of the factor structure of this scale by Yıldırım and Solmaz (4). The Iranian version of the COVID-19-BS has a good internal consistency, which is in line with the results of Yıldırım and Solmaz. This finding is consistent with the original version of the scale, which suggests a global factor structure for the scale (4).
Our research findings support the use of COVID-19-BS as a short, convenient, cost-effective, and one-dimensional scale for assessing COVID-19 burnout. Even if COVID-19-BS is valid for use in the current epidemic, it can easily be used to assess burnout in other future public health crises. This can be done simply by modifying the text of the relevant items, such as replacing the term "COVID-19" with a specific term for another epidemic.
To evaluate the convergent validity of the COVID-19-BS, we examined its relevance to the C-19ASS, which showed a positive and significant correlation (23, 24). To examine the divergent validity of the COVID-19-BS, we examined its relationship with the CS, which showed a significant negative correlation, indicating an appropriate divergent validity (25, 26).
Compassion helps people understand that much of what goes on in our minds is not designed by us, and therefore not our fault. Clarifying this point when people are upset, anxious, depressed, tired, or feeling out of control has a key role to play in eliminating feelings of worthlessness, uselessness, and inadequacy. Compassion helps people realize that most of life’s problems and how to respond to them are not their own choice or planning, and that they should not blame themselves. Compassion helps people accept suffering under the influence of compassion and face it voluntarily, but not to drown in it. One of the results of helping clients is that it leads to the growth and development of compassionate motivation.
There are some limitations in interpreting and generalizing the results of our study. First, all the evaluated instruments in this study were self-report questionnaires. Therefore, correlations could have been inflated by common method variance. Second, this study had a cross-sectional and correlational design that does not allow causal interpretations and inferences. Third, the participants in this study may not have represented the general population; so, it is important to examine the general population. The psychometric properties of COVID-19-BS should be assessed in other communities and related samples. Fourth, since the study was conducted online, it was not possible to control how the questionnaires were filled out, and this problem may limit us in generalizing the results.
5.1. Conclusions
The main purpose of our study was to investigate the psychometric properties of COVID-19-BS in an Iranian population. COVID-19-BS can help to investigate the relationship between COVID-19 and the manifestations of psychopathology in constructing explanatory models. The present psychometric study complements the cross-cultural literature of this tool and is a suitable tool for research and clinical work. COVID-19-BS has a good validity and reliability in Iranian population.