1. Background
In December 2019, the World Health Organization (WHO) announced a novel viral pneumonia originated from Wuhan, China (1). As of November 15 2020, over 53.7 million coronavirus cases and 1.3 million deaths were reported globally (2). Due to the COVID-19 pandemic, numerous unexpected and unprecedented changes happened in daily living activities of all individuals. Experiencing social isolation and quarantine, being exposed to the news regarding COVID-19 pandemic, the fear of being infected with the virus, and the uncertainty about the future have made people distressed (3-5). As the number of infected cases and death rates surged, drastic measures to control the rate of the virus spread increased universally. While an extensive effort has been put into finding individuals with COVID-19 infection, identifying the psychological issues of individuals affected by the COVID-19 pandemic has been forsaken comparatively (6).
In accordance with the literature regarding nations facing pandemics, it is clear that a large part of populations experience average to high levels of anxiety due to the pandemic (7-12). The COVID-19 pandemic has had a great impact on several dimensions of daily life in Iran, including how to socialize, live, work, shop, and plan for future. Studies focused on previous global pandemics have revealed that individuals suffering from anxiety (related to the pandemic they experienced) tend to demonstrate high levels of anxiety, including health anxiety, general anxiety, post-traumatic stress, and suicidality (12-15). In general, during recent pandemics, people seem to suffer from psychological distress (stress, fear, anxiety, and depression). Elevated rates of infection and death due to COVID-19 caused extensive anxiety (16, 17). An epidemic study of psychological symptoms in China (i.e., the first country where the coronavirus was identified) showed that in the first phase of COVID-19 pandemic, more than half of their respondents were affected by moderate to severe psychological symptoms, and about one-third of the participants had moderate to severe anxiety levels. In another study, more than 70% of their participants showed moderate to severe psychological symptoms, especially regarding their obsessive-compulsive, interpersonal sensitivity, anxiety, and psychosis scores (18, 19).
While the psychological effects of the changes in daily life have been well-recognized and shown by the media, the needs associated with psychological well-being of individuals who are suffering from the current pandemic have been neglected relatively (6). Moreover, to what extent the present psychological issues might be associated with COVID-19 anxiety has not been established (20). As a matter of fact, while healthcare systems across the globe are attentive to the increasing levels of anxiety among individuals, there is a need to have some evaluation tools to examine and identify the level of anxiety (20). Creating a reliable measuring tool could help healthcare systems, scholars, and policymakers to have adequate information regarding the psychological symptoms and significance of the anxiety due to the COVID-19 outbreak and how to approach it (20, 21). Accordingly, the Coronavirus Anxiety Scale (CAS) (20) was developed to help find individuals primarily affected by the fear and uncertainty of this current pandemic crisis. The 5-item CAS is designed to screen and identify people with coronavirus-related anxiety. This scale was shown to have high reliability (α = 0.93) and a stable factor structure (20). Also, in a study conducted by Lee (22), the Cronbach’s alpha (α) of this scale was 0.92, and the results of confirmatory factor analysis (CFA) confirmed the one-factor model of this scale. The results of the mentioned study showed that CAS scores were positively associated with functional impairment, fear of coronavirus, negative religious coping, severe frustration, alcohol or drug coping, and passive suicidal ideation (22). In the Turkish version of this scale, the validity and reliability were at satisfactory levels (α = 0.92) (23). Also, in the Korean version, the CAS scale had good psychometric properties and structural validity (24).
2. Objectives
Although nearly two years have passed since the onset of COVID-19 pandemic and various COVID-19-related tools to assess stress and anxiety have been developed, the length of the current questionnaire, its standardization in different countries, and convergent validity of Persian (Iranian) version of the Coronavirus Anxiety Scale (P-CAS) with different tools are the main strengths of the present study. Such an instrument may be helpful for healthcare systems to identify the psychological impacts of COVID-19 on people and develop suitable treatment programs to manage the anxiety caused by the COVID-19 pandemic. Thus, the current study aimed to assess the psychometric properties of CAS (20) in Iran.
3. Methods
3.1. Study Population
Online survey data from 305 adults were collected in Iran. Regarding the adequate sample size for CFA, three to 20 times the number of variables was recommended (25). With five variables, 305 was considered as a good sample size. The study sample included 121 males and 184 females with a mean age of 36.44 years (SD = 11.20). Regarding marital status, 40.4% of the participants were single, and 59.6% were married. In terms of educational level, 21.6%, 40.7%, and 37.7% of participants had a high school diploma, bachelor’s degree, and higher than bachelor’s degree, respectively. Most of the participants reported that they had not been diagnosed with coronavirus (78%).
3.2. Measures
The primary purpose of current study was to assess the psychometric properties of CAS in Iran. So, other measures were also used to evaluate the validity of P-CAS. The online survey included P-CAS, COVID Stress Scales (CSS), the short form of the Depression Anxiety Stress Scales (DASS-21), Whiteley index (WI), and Difficulties in Emotion Regulation Scale (DERS).
Background information. Participants reported their age, gender, marital status, education, and history of coronavirus diagnosis.
The CAS (20). CAS is a 5-item self-report questionnaire which evaluates the psychological reactions in relation to COVID-19. It is rated on a 5-point Likert scale from 0 (not at all) to 5 (nearly every day over the last two weeks). The scale showed an acceptable internal consistency and test-retest reliability. The cutoff score for this scale is ≥ 9, and it has good sensitivity (90%) and 85% specificity (20).
The CSS (10). CSS is a 36-item self-report questionnaire which measures fear of becoming infected, fear of coming into contact with possibly contaminated objects or surfaces, fear of foreigners who might be carrying infection, fear of the socio-economic consequences of the pandemic, compulsive checking, and reassurance-seeking regarding COVID-19. CSS is rated on a 5-point Likert scale, and it has yielded excellent internal consistency (> 0.80) and convergent validity (10). The Persian version of the scale is under publication; however, Cronbach’s alpha of CSS in the present study was 0.95.
The DASS-21 (26). DASS-21 is a 21-item self-report questionnaire with seven items for each of the subscales of depression, anxiety, and stress. Subjects should score all items on a 4-point Likert scale from 0 (did not apply to me at all) to 3 (applied to me very much). The DASS-21 is a reliable and valid instrument for evaluating depression, anxiety, and stress symptoms in clinical and non-clinical population (27-29). The Persian version of the DASS-21 has demonstrated a good construct validity, convergent validity, and test-retest reliability (30).
The WI (31). The WI is a 14-item self-report questionnaire that assesses health anxiety. It is reported on a 5-point Likert scale from 1 to 5. WI has demonstrated acceptable construct validity and high test-retest reliability (r = 0.80) (31). The Iranian version of WI has showed agreeable construct validity and internal consistency (α= 0.88) (32).
The DERS (33). The DERS is a self-report scale with 36 items that evaluates individuals’ typical tendencies toward emotion regulation. DERS is rated on a 5-point Likert scale from 1 (almost never) to 5 (almost always). It consists of six subscales, including 1- Not accepting emotional responses, 2- Difficulties engaging in behaviors which are based on goals, 3- Difficulties in impulse control, 4- Emotional awareness deficiency, 5- Restricted access to emotion regulation strategies, and 6- Emotional clarity deficiency. The DERS demonstrated acceptable internal consistency (α = higher than 0.80 for each subscale) and agreeable test-retest reliability (r = 0.88) (33). The Iranian version of the DERS has satisfactory reliability and validity (30). The Cronbach’s alpha of the DERS in the present study was 0.94.
3.3. Procedure
The English version of CAS was translated into Persian by the first author and back-translated into English by an independent bilingual translator who is an English language expert. The two forms of translated and original CAS were compared by an independent person adept at the English Language (fourth author). After that, five assistant/associate professors of clinical psychology checked the translation to ensure the questionnaire’s content validity. The psychologists found the translated P-CAS fluent, friendly, and comprehensive in terms of assessing P-CAS (CVR = 0.91). To evaluate the psychometric properties of P-CAS, participants filled the self-report questionnaires online at http://porsall.com/Poll/Show/39b7b6618b4b4b1. Data collection procedure was conducted from August 5, 2020, to September 15, 2020. For the data collection procedure, when the questionnaires were available online, a link of the questionnaires along with the necessary descriptions and explanations were sent to the participants in various social networks (e.g., WhatsApp, LinkedIn, Telegram, and Instagram). After reading the descriptions, if the inclusion criteria were met (e.g., being over 18 years of age, being resident of Iran, having a certain literacy level, and having signed the informed consent form), the subjects were directed to the questionnaires page and answered the questions. Finally, the participants who fully answered the questionnaires entered the analysis. Completing the entire assessment required 20 - 30 minutes. To assess the test-retest reliability, 51 individuals were recruited among community samples to fill in the CAS in a two-week interval. The current study was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences, Tehran, Iran (IR.SBMU.MSP.REC.1399.263).
To minimize the potential biases related to convenience sampling method, which compromise the external validity, the questionnaire’s link was sent to different virtual spaces in which the users had different education levels and demographic variables.
3.4. Statistical Analysis
Descriptive statistics, including frequency, percentages, mean, and standard deviation, were used to assess the participants’ characteristics. Out of 320 participants, 15 individuals with more than 10% missing items were deleted from the analysis. Normality was checked using skewness and kurtosis (values between ± 2); all variables were normal. Using the classical test theory (CTT), internal consistency, and corrected item-total correlation were examined. The structure of the CAS was examined using a series of CFA with maximum likelihood estimation and fixing a factor loading to 1 method, performing AMOS 23 (one for whole and two for each gender). Goodness-of-fit index (GFI) for the CFA model was checked using the following criteria: Chi-2 (χ2) with a ratio < 5 as an acceptable ratio (34), as well as GFI, Adjusted Goodness-of-fit index (AGFI), and comparative fit index (CFI) with a cut-off ≥ 0.95 as acceptable (34). Root mean square error of approximation (RMSEA) with value < 0.08 was considered acceptable (34). Internal consistency was evaluated using Cronbach’s alpha. Test-retest reliability and convergent validity were evaluated using the intraclass and Pearson correlation coefficients, respectively. SPSS 23 and AMOS-23 were used to analyze the data.
4. Results
4.1. Factor Structure
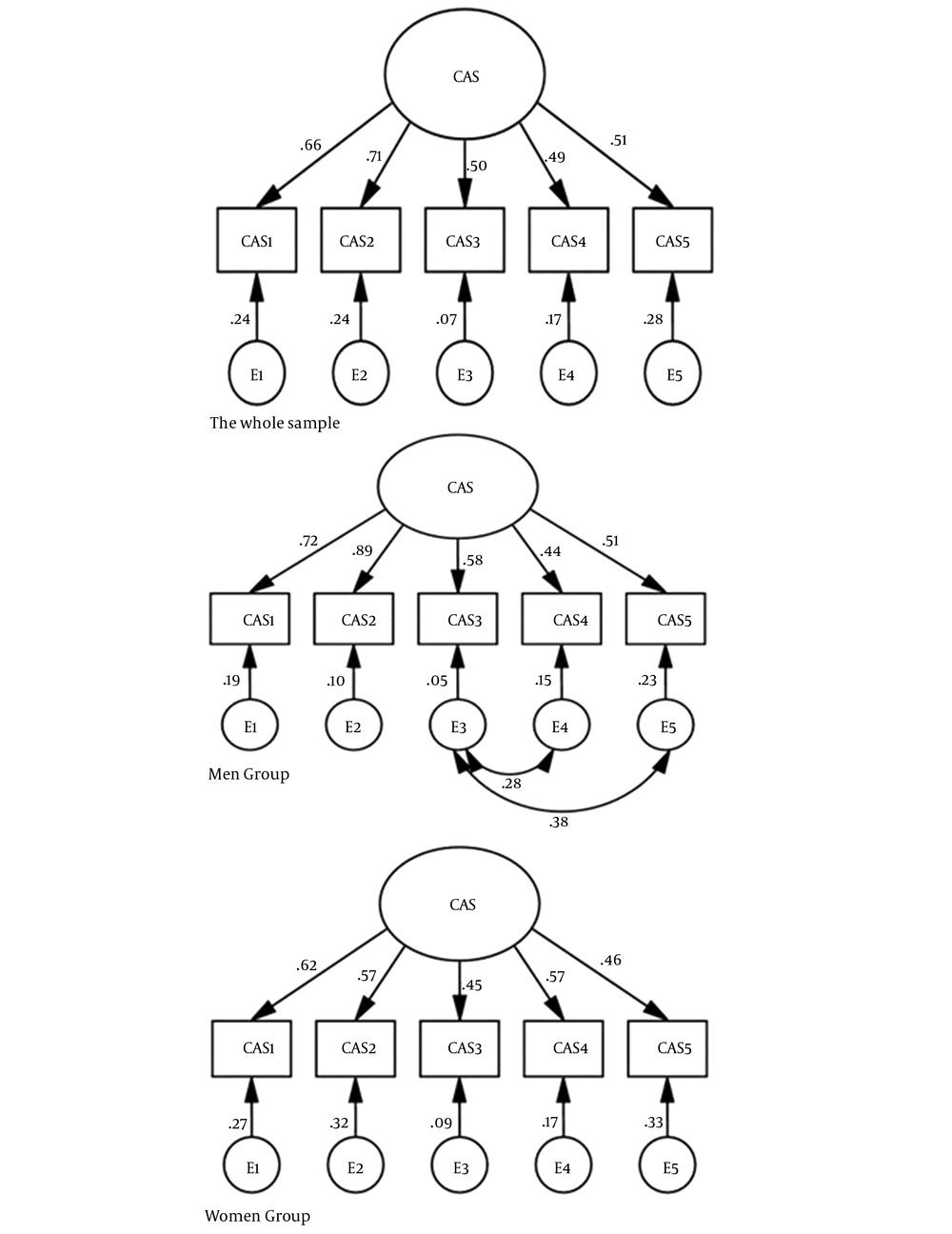
The unidimensionality of the Persian CAS was assessed using CFA with maximum likelihood. The single-factor CAS model yielded a good fit model (χ2/df = 1.19, GFI = 0.99, AGFI = 0.97, CFI = 0.99, and RMSEA = 0.02) (Figure 1, the whole sample). Another CFA was conducted for males; the results showed a good model fit except for RMSEA. So, modification indices were examined, which yielded an acceptable model fit (χ2/df = 1.001, GFI = 0.99, AGFI = 0.95, CFI = 1, RMSEA = 0.004) (Figure 1, males). The results of CFA for females demonstrated an agreeable model fit (χ2/df = 1.89, GFI = 0.98, AGFI = 0.93, CFI = 0.96, and RMSEA = 0.07) (Figure 1, females).
4.2. Reliability
The internal consistency of the P-CAS using Cronbach’s alpha coefficient was good (0.80) (Table 1). Furthermore, when deleting any of the five items of the scale, the Cronbach’s alpha did not increase. Moreover, item-total correlations for the P-CAS were agreeable, ranging from 0.53 (CAS 3) to 0.70 (CAS 2), and inter-item correlations of the CAS ranged from 0.37 (between items 1 and 3) to 0.60 (between items 1 and 2) (Table 1). Finally, the results of test-retest reliability coefficient using intraclass correlation coefficients for CAS was excellent (ICC = 0.95, P < 0.001) (Table 1).
| Item | Mean ± SD | Factor Loadings | Item-Total Correlation | Inter-Item Correlation | |||
|---|---|---|---|---|---|---|---|
| 2 | 3 | 4 | 5 | ||||
| CAS 1 | 0.44 ± 0.77 | 0.66 | 0.63 | 0.60 | 0.37 | 0.50 | 0.47 |
| CAS 2 | 0.44 ± 0.87 | 0.71 | 0.70 | 0.50 | 0.47 | 0.55 | |
| CAS 3 | 0.15 ± 0.45 | 0.50 | 0.53 | 0.47 | 0.35 | ||
| CAS 4 | 0.27 ± 0.62 | 0.49 | 0.58 | 0.43 | |||
| CAS 5 | 0.31 ± 0.79 | 0.51 | 0.59 | ||||
| Mean ± SD | |||||||
| Cronbach’s alpha | 0.80 | ||||||
| Test-retest reliability | 0.95 | ||||||
| AVE | 0.50 | ||||||
| CR | 0.83 | ||||||
Abbreviations: CFA, Confirmatory factor analysis; CAS, Coronavirus Anxiety Scale; SD, Standard deviation; AVE, average variance extracted; CR, composite reliability.
a All factor loadings and item-item Pearson correlations were statistically significant (P < 0.001).
4.3. Convergent Validity
Convergent validity was assessed by correlating P-CAS scores with the scores of related scales (CSS, DASS-21, WI, and DERS). The correlations between CAS and total score of CSS (r = 0.49, P < 0.001), subscales of CSS including danger (r = 0.25, P < 0.001), socio-economic consequences (r = 0.25, P < 0.001), xenophobia (r = 0.27, P < 0.001), contamination (r = 0.34, P <0.001), traumatic stress (r = 0.70, P < 0.001), and compulsive checking (r = 0.38, P < 0.001), CAS and anxiety (r = 0.49, P < 0.001), P-CAS and stress (r = 0.36, P < 0.001), P-CAS and depression (r = 0.32, P < 0.001), P-CAS and WI (r = 0.36, P < 0.001, ), and P-CAS and DERS (r = 0.30, P < 0.001) were statistically significant (Table 2).
| Variables | Mean | SD | Skewness | Kurtosis | Correlation | P Value |
|---|---|---|---|---|---|---|
| CSS-total | 51.76 | 23.55 | 0.26 | -0.37 | 0.49 | 0.001 |
| Danger | 11.84 | 5.41 | -0.26 | -0.22 | 0.25 | 0.001 |
| Socio-economic | 4.40 | 4.57 | 1.11 | 0.77 | 0.25 | 0.001 |
| Xenophobia | 10.39 | 5.92 | 0.32 | -0.53 | 0.27 | 0.001 |
| Contamination | 12.04 | 5.59 | 0.018 | -0.70 | 0.34 | 0.001 |
| Traumatic stress | 4.30 | 5.07 | 1.46 | 1.50 | 0.70 | 0.001 |
| Compulsive checking | 8.77 | 5.14 | 0.51 | -0.16 | 0.38 | 0.001 |
| Anxiety | 4.38 | 4.04 | 1.08 | 1.03 | 0.49 | 0.001 |
| Stress | 7.24 | 5.39 | 0.45 | -0.51 | 0.36 | 0.001 |
| Depression | 6.06 | 5.00 | 0.76 | -0.24 | 0.32 | 0.001 |
| WI-total | 34.02 | 9.92 | 0.41 | -0.38 | 0.36 | 0.001 |
| DERS-total | 86.89 | 23.66 | 0.63 | 0.12 | 0.30 | 0.001 |
Abbreviations: CSS, COVID Stress Scales; WI, Whiteley index; DERS, Difficulties in Emotion Regulation Scale.
4.4. Mean Differences Analysis
Independent sample t-tests revealed no significant differences in P-CAS scores between males and females at educational level, and between participants who had COVID-19 diagnosis history and participants who did not have it. However, independent samples t-tests revealed significant differences between those who had higher scores on anxiety (≥ 10), depression (≥ 14), and stress (≥ 19) scales (N = 54, MD = 2.37, SD = 2.54) and those who did not have it (N = 251, MD = 1, SD = 1.69 in P-CAS scores, t (303) = 4.90, P < 0.001).
5. Discussion
The current COVID-19 pandemic has had several impacts on the mental health of individuals in different societies. Recent studies showed that the experience of quarantine and social isolation (4), the news associated with COVID-19 (5), fear of dying from the virus, and worries about the future (3) can affect one’s mental health. In general, research states that the COVID-19 and its related conditions are associated with the experience of symptoms of anxiety and depression in individuals (7, 17, 35). The primary purpose of the present study was to assess the psychometric properties of the CAS in a sample recruited from the general population in Iran.
A single-factor solution for the P-CAS was demonstrated in the CFA for all samples, as well as for both males and females, which was in accordance with the previous study regarding the unidimensional factor structure of the CAS (22). Moreover, the CFA results were shown to be statistically significant and relatively high factor loadings, illustrating all items were suitable indicators of the construct, which was the dysfunctional anxiety due to the COVID-19 pandemic. Consistent with the previous studies (22, 23), the Cronbach’s alpha measured for the Persian version was acceptable (α = 0.80), and P-CAS also showed excellent test-retest reliability (ICC = 0.95).
The high inter-item correlation between items 1 and 2 is a finding which needs further analysis. As these two items evaluate different symptoms (item 1: Dizzy, lightheaded, or faint, and item 2: Trouble falling or staying asleep), they do not have the same content. Since both items 1 and 2 evaluate symptoms related to coronavirus anxiety, they have an equal value in assessing these symptoms and can be interchangeable. Hence, it is suggested to keep both items because they evaluate different contents (36).
Furthermore, convergent validity was supported due to positive correlations between the P-CAS and the related measures, including CSS, DASS-21, WI, and DERS. The results of mean differences analysis showed that individuals with higher scores on anxiety, depression, and stress reported higher COVID-19 anxiety.
The results of the present study showed that COVID-19-related anxiety is significantly associated with symptoms of stress, anxiety, and depression. These findings are consistent with some previous studies (17, 22). Furthermore, findings of this study illustrated that anxiety associated with COVID-19 has a significant relationship with dysfunctional emotion regulation and health anxiety, which was in line with other previous studies (37, 38). Moreover, emotion regulation and health anxiety are among the factors influencing the individuals’ coping styles associated with the COVID-19 (37). People with health anxiety interpret bodily functions as dangerous ones. Depending on the previous experiences with the flu and current information about the current disease (COVID-19), these individuals may experience severe anxiety by experiencing even single symptoms such as coughs or muscle pain (37). Also, emotion regulation styles play an important role in experiencing anxiety symptoms in individuals (38).
The most robust finding of this study was the results of convergent validity. Traumatic stress had the highest relationship with P-CAS. This is an important finding because P-CAS is a clinical screener designed to identify those who are probably suffering from clinical levels of anxiety, and the fact that this is strongly correlated with a measure of extreme distress supports this perspective. This finding is also in line with the primary goal of developing P-CAS which is a mental health screener designed to find those few people who are really suffering. (20, 22).
Overall, in this study, the validity and reliability of the P-CAS was confirmed. Thus, this instrument could be utilized for diagnostic and academic aims among the general Iranian population.
5.1. Limitations
There were some limitations in this study. First, the current study was conducted as an online survey. Consequently, individuals who did not have access to Internet or were not technology savvy could not partake in the current study. Secondly, the results of the current study were obtained mostly from participants’ self-reports. So, the results might be biased to some extent since self-reports have their specific limitations (e.g., social desirability, or short-term recall).
5.2. Conclusions
The results from this research indicated that the P-CAS had a unidimensional construct as an instrument. The P-CAS had suitable psychometric properties for identifying the anxiety caused by the COVID-19 outbreak among Iranians.