1. Background
Obesity is defined as excess body fat accumulation that may threaten personal health. Body mass index (BMI) is a measure of weight that shows underweight, normal weight, and overweight. It is calculated by dividing weight in kilograms by height in meters squared (1). The obesity crisis is one of the major public health issues in the 21st century. The incidence of obesity has increased dramatically worldwide in recent years (2). The World Health Organization claims that a higher percentage of women is found to be obese than men in all regions of the world per year. No less than 2.8 million people die of obesity worldwide per year. It is estimated that 2.3% of all deaths occur because of obesity (1). Obesity has a negative impact on vital organs, especially the cardiovascular system and metabolism. It also reduces life expectancy by 10 years (3). The psychosocial experience of “feeling overweight” is linked to psychological consequences that increase the risk of unhealthy behaviors and emotional suffering (2).
Depression, anxiety, and stress are the psychological factors that mediate obesity. Obesity and anxiety are interactive factors. Anxiety is an unpleasant feeling that increases emotional eating behavior in some people (4). Being overweight also increases the risk of anxiety (5). Stress has a direct impact on physiological factors and healthy behaviors (e.g. diet). It may influence appetite and increase f food intake in people (6). The relationship of anxiety and depression with obesity was not explicit in the studies. Some studies showed an insignificant relationship between these factors (7).
Various therapies are recommended for losing weight. Cognitive-behavioral Therapy (CBT) is one of the widely used psychotherapies for obesity disorder (8). Cognitive-behavioral therapy for obesity focuses on not only losing weight but also finishing weight regain, thereby, deviating the dissatisfactory long-term results of earlier behavioral treatments. It firmly differentiates between weight loss and weight maintenance, allowing patients to exercise effective weight-maintenance strategies, for example, avoiding unrealistic weight goals and addressing obstacles to weight maintenance (9). It motivates nearly 50 to 60% of the patients to avoid emotional overeating at the end of treatment. This result also persisted at long-term follow-ups (10). However, the expense of face-to-face CBT and the long distance to visit the center hinder this therapy (11). Obese people are ashamed of face-to-face meetings due to their physical appearance. This issue also hinders face-to-face therapy (12). Therefore, internet-based cognitive behavioral therapy can be a solution to these obstacles.
Internet-based cognitive behavioral therapy (ICBT) is an internet-based psychological intervention that employs CBT factors and uses multimedia technology, either a website or an application, to interact with the patients (13). Thus, ICBT is a promising method of improving access to CBT for a variety of mental health conditions, and the therapist can contact the patients via phone calls, emails, and text messages (14). The patients benefit from psychotherapy services regardless of physical presence in the centers and fear of negative evaluation. They can remain anonymous, a unique feature of this therapy, which encourages others to participate in this therapy (15). Remote psychotherapy is an effective kind of treatment best used for different populations and media. It ensures the persistence and accessibility of treatment and greatly reduces the cost of treatment (16).
The results of a randomized clinical trial that compared face-to-face CBT and ICBT showed that face-to-face CBT was more effective in four- and six-month follow-up than ICBT. Exploratory analysis in a smaller sample showed that these differences were negligible in a 1.5-year follow-up (17). In their study, van den Berg et al. developed and assessed ICBT and showed the effectiveness of this therapy in patients with binge eating disorder or other types of eating disorders (18). In another study, patients with eating disorders underwent CBT via a mobile video app. The patients reported significant decreases in the number of meals they ate and symptoms of the disease. They were satisfied with the format of the therapy (19). Ebert et al. provided evidence of the effectiveness of computer-based and internet-based CBT in treating anxiety and depressive symptoms in young people (20). Tham and Chong reported the effectiveness of ICBT in reducing stress, anxiety, and depression (21). But, Waite et al. did not produce better results in the ICBT intervention group than in the waiting list (22). Online chat groups can increase access to therapy and serve as a cost-effective approach to psychotherapy services (23). The results of research on ICBT are divergent, and this relationship has not been significant in some studies (24). However, ICBT has promised to be an effective and potentially cost-effective alternative and complement to face-to-face therapy. More studies are needed before firm conclusions can be drawn (14).
2. Objectives
The study aimed to assess the effectiveness of the ICBT therapy package using a WhatsApp group on BMI, stress, anxiety, and depression.
3. Methods
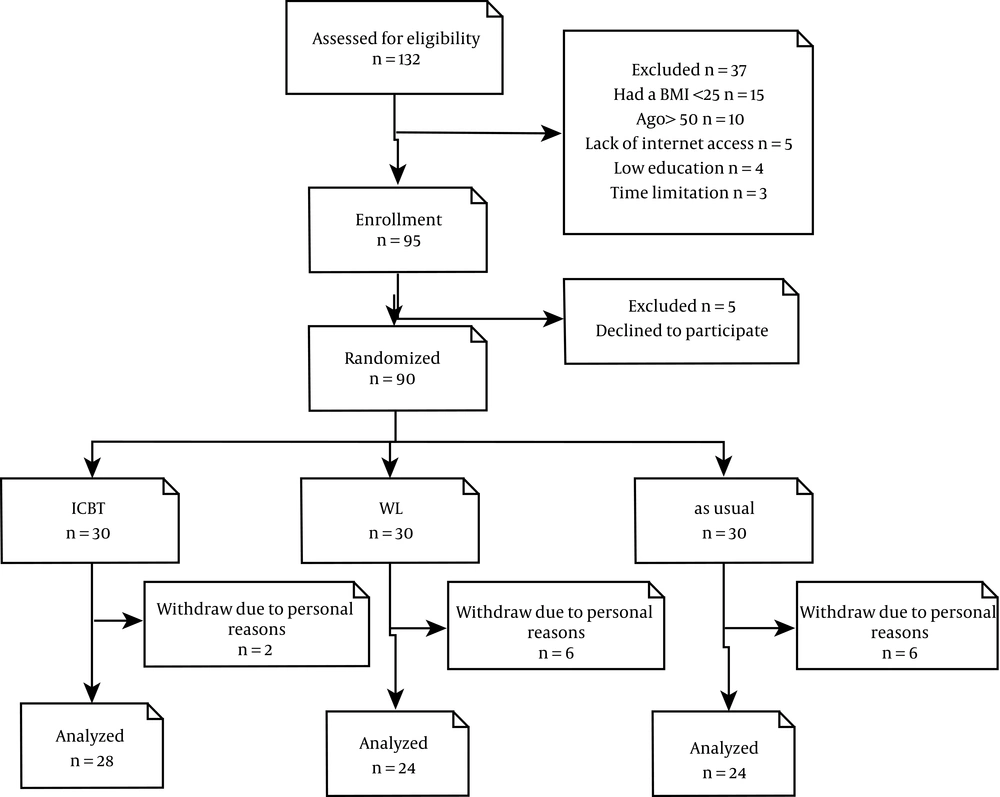
The present study was a randomized controlled trial (IRCT20210306050594N1) conducted among users who were overweight women with BMI ≥ 25 in Neyshabur city in 2019 - 2020. The sample size was calculated to be 90 people with an alpha of 0.05, power of 0.8, and assumed effect size of 0.7, using covariance analysis method with G*Power analysis. The allocation of participants to each of the intervention and control groups was done with simple randomization using a random number table. The data analysts and evaluators were blind to the treatments during the trial. A Ph.D. student in psychology diagnosed the patients based on DSM-V (SCID-V) through structured diagnostic interviews and assessed inclusion and exclusion criteria (Figure 1). Participants were allocated to either of the ICBT experimental group (n = 30), treatment-as-usual (TAU) (n = 30), and waiting list group (n = 30).
Inclusion criteria were BMI ≥ 25, age of 18 to 50, at least a high school diploma, fluency in Persian, internet access, and knowing how to use it. Besides, no menopause or pregnancy, breastfeeding, psychosis, bipolar disorder based on SCID-V (the first meeting was face-to-face), no specific diseases including diabetes, thyroid, cancer, cardiovascular disease, and not taking psychotropic drugs or drugs that affected weight were other inclusion criteria. Exclusion criteria included the absence from more than three sessions and a distorted questionnaire.
Participants were assessed before and after stimulation with the Depression Anxiety Stress Scale (DASS) and BMI. The DASS was developed by Lovibond (1995) to measure anxiety, depression, and stress. Each item is scored based on four options ranging from 0 (does not apply to me at all) to 3 (absolutely applies to me). Three subscales of depression, anxiety, and stress are measured by seven different items based on the Likert scale. The minimum and maximum scores in each subscale are 0 and 21, respectively (25). Asghari Moghaddam et al. (2008) assessed a sample of 420 people in the public Iranian population and calculated Cronbach’s alphas of depression, anxiety, and stress as 0.78, 0.87, and 0.91, respectively. They confirmed the adaptability of DASS to the Iranian population and authorized the use of this instrument in clinical trials that involve psychological interventions (26).
Height and weight were measured while participants wore lightweight clothing. The BMI (kg/m2) was calculated by dividing weight in kilograms by height in meters squared using a calculator. The World Health Organization suggestions for Asian populations were used to categorize individuals into five BMI groups: (1) < 18.5 kg/m2 (underweight), (2) 18.5 - 22.9 kg/m2 (normal), (3) 23.0 - 24.9 kg/m2 (overweight), (4) 25.0 - 29.9 kg/m2 (class I obese), and (5) ≥ 30 kg/m2 (class II obese) (27).
The ICBT intervention group underwent this therapy. The TAU group underwent a specific diet under the supervision of a nutritionist in a weekly manner. The WL group did not receive any treatment. The ICBT sessions were designed based on Judith Beck’s CBT for weight loss plan in 42 two-hour sessions (28). The ICBT was implemented by a Ph.D. student in clinical psychology who had completed a CBT training course at the Tehran Psychiatric Institute. The project was carried out during the COVID-19 pandemic. Two WhatsApp groups were created with the name of weight loss (30 people in the ICBT group and 30 people in the WL group). An audio file of the content of each session and relative assignments was recorded by the therapist and shared with the ICBT group. A summary of ICBT sessions included familiarity with the logic of treatment, familiarity with challenging thoughts and challenges with them, familiarity with the ABC pattern, setting goals, starting a diet, examining destructive thoughts related to dieting and responding to them, overcoming the remaining destructive challenges and thoughts, adjusting and developing new skills, how to stop losing weight and stabilizing new weight, and evaluating and summarizing. Online meetings were held every day, and participants were able to chat in this group during the day. Online meetings also included online chats, audio, and video calls by taking into account the content of each therapy session. The participants undertook their tasks and shared them in the group. They also interacted with other members of the group, supported each other, and gave feedback. The session ended with an assignment and feedback assessment. The goal of each session was to replace inefficient people with efficient people.
4. Results
Initially, eight Ph.D. people in psychology were asked to determine whether the proposed model for ICBT has content validity. The average opinions of the experts in all dimensions, including the content of training sessions, structure, adequacy, duration, and length of sessions, comprehensiveness, and applicability of the protocol for virtual implementation, were between 4.25 - 3.75, which shows a positive evaluation in all dimensions.
Table 1 shows the demographic characteristics of the participants. The highest percentage of participants had 18 to 30 years of age (38.2%). The majority of the participants were married (67%) and had an academic degree (35%). The chi-square statistics for variables of age, education, and marriage were greater than 0.05 in comparing the three groups. Therefore, the three groups did not significantly differ in terms of age, education, and marriage.
| Variables | Frequency in Each Group | No. (%) | Chi-Square | P | ||
|---|---|---|---|---|---|---|
| ICBT | WL | TAU | ||||
| Age | 4.97 | 0.52 | ||||
| 18 to 30 | 7 | 11 | 11 | 29 (38.2) | ||
| 31 to 40 | 11 | 7 | 4 | 22 (28.9) | ||
| 41 to 50 | 10 | 6 | 9 | 25 (32.9) | ||
| Education | 6.59 | 0.58 | ||||
| Middle school | 2 | 5 | 2 | 9 (11.8) | ||
| Diploma | 12 | 11 | 9 | 32 (42.1) | ||
| College education | 14 | 8 | 13 | 35 (46.1) | ||
| Marital status | 2.33 | 0.31 | ||||
| Married | 23 | 21 | 23 | 67 (86.8) | ||
| Single | 5 | 3 | 1 | 19 (11.8) | ||
Demographic Characteristics (Age, Education, Marital Status) of Participants
Table 2 shows a decrease in BMI scores in the ICBT and TAU groups in the posttest compared to the pretest, while this decrease was not seen in the WL group. There was also a decrease in the mean scores of stress, anxiety, and depression in the ICBT group, but this decrease was not significant.
| Variables | Pretest | Posttest |
|---|---|---|
| BMI | ||
| ICBT | 30.78 ± 1.42 | 29.70 ± 1.36 |
| WL | 30.27 ± 1.11 | 30.82 ± 1.15 |
| TAU | 31.17 ± 0.84 | 30.39 ± 0.86 |
| Stress | ||
| ICBT | 18.35 ± 0.92 | 17.64 ± 1.00 |
| WL | 16.45 ± 0.74 | 16.54 ± 0.98 |
| TAU | 18.25 ± 1.04 | 18.75 ± 1.09 |
| Anxiety | ||
| ICBT | 14.03 ± 0.92 | 13.75 ± 0.97 |
| WL | 11.87 ± 0.78 | 12.54 ± 0.75 |
| TAU | 14.08 ± 1.17 | 14.70 ± 1.11 |
| Depression | ||
| ICBT | 15.60 ± 1.05 | 15.46 ± 1.11 |
| WL | 13.12 ± 0.91 | 13.87 ± 1.02 |
| TAU | 16.70 ± 1.33 | 16.25 ± 1.31 |
Descriptive Information (Mean and Standard Error) of BMI, Stress, Anxiety, and Depression in ICBT, WL, and TAU a
The assumptions of the equality of variance (Levene’s test), data normality, and homogeneity of regression slopes were accepted (P > 0.05). The ANCOVA results showed a significant difference in the BMI scores at the posttest between the ICBT group and the TAU and WL groups after adjustment for pretest scores [F (72, 2) = 15.54, P < 0.0005; Partialη2 = 0.30]. However, the difference was not significant in the variables of stress [F (72, 2) = 0.47, P = 0.63; Partialη2 = 0.01], anxiety [F (72, 2) = 0.49, P = 0.61; Partialη2 = 0.01], and depression [F (72, 2) = 0.06, P = 0.93; Partialη2 = 0.002] (Table 3).
| Variables/Sources | Sum of Squares | df | Mean Square | F | P | PES |
|---|---|---|---|---|---|---|
| BMI | 15.547 | 0.00 | 0.30 | |||
| PRE BMI | 1576.662 | 1 | 1576.662 | |||
| Group | 37.908 | 2 | 18.954 | |||
| Error | 87.778 | 72 | ||||
| Stress | 0.47 | 0.63 | 0.01 | |||
| PRE Stress | 717.09 | 1 | 717.09 | |||
| Group | 15.63 | 2 | 7.81 | |||
| Error | 1208.79 | 72 | ||||
| Anxiety | 0.49 | 0.61 | 0.01 | |||
| PRE Anxiety | 846.76 | 1 | 846.76 | |||
| Group | 12.137 | 2 | 6.06 | |||
| Error | 891.87 | 72 | ||||
| Depression | 0.06 | 0.93 | 0.002 | |||
| PRE Depression | 1334.98 | 1 | 1334.98 | |||
| Group | 1.90 | 2 | 0.95 | |||
| Error | 1061.38 | 72 |
ANCOVA for BMI, Stress, Anxiety, and Depression
Table 4 shows the adjusted means of the BMI variable, and the effect of the auxiliary random variable is statistically eliminated. The mean BMI was 29.98 in the ICBT group, 31.64 in the WL group, and 30.32 in the TAU group, which indicated a decrease in BMI in the ICBT intervention group after treatment.
| Groups | Mean ± SE | 95% Confidence Interval | |
|---|---|---|---|
| Lower Bound | Upper Bound | ||
| BMI | |||
| ICBT | 29.987 ± 0.209 | 29.569 | 30.404 |
| WL | 31.645 ± 0.227 | 31.193 | 32.096 |
| TAU | 30.324 ± 0.225 | 29.874 | 30.773 |
Adjusted Mean Scores for BMI Variable
5. Discussion
The results of the analysis of covariance showed that there was a statistically significant difference between ICBT, TAU, and WL groups (P < 0.001). Bonferroni post hoc test showed that ICBT, like TAU, significantly reduced BMI compared to WL. Consistent with this study, Abrahamsson et al. showed that CBT via a mobile video app is well accessible to patients, despite some technological issues, and that all participants in this study previously had little access to mental health services and high satisfaction with this form of therapy (19). Zerwas et al. showed that the online format of CBT via chat groups was an effective treatment for bulimia nervosa although the course of recovery might be slower than in face-to-face therapy (29). These results are not consistent with the findings of the study by Jacobi et al., who assessed web-based psychological services in women with bulimia nervosa. The results of this study showed no significant difference between the intervention and waiting list groups (24).
The effectiveness of ICBT in reducing the BMI of individuals is highlighted in the monitoring of patients (an important aspect of CBT) that leads to weight loss during CBT. The patients are taught to supervise their food intake, emotions, feelings, overeating behaviors, and interpersonal problems (28). Group members interact with the therapist to assess and identify barriers and concerns relevant to weight loss and modify their eating behaviors in CBT. Emphasis on modifying and changing overeating thoughts and behaviors of obese people and the importance of objectives and behavioral tasks motivate the people to follow a healthy diet by engaging in physical exercise to lose weight (30). People also use cognitive restructuring techniques to explore and challenge their spontaneous thoughts versus fundamental beliefs. They learn to use problem-solving strategies to solve their diets and interpersonal problems (28). The format of counseling sessions, its goals, use of various cognitive-behavioral techniques, and daily assessment of assignment in 42 therapy sessions enhanced the effectiveness of CBT. This issue justifies the effectiveness of ICBT in reducing BMI.
Obese people are ashamed of face-to-face meetings due to their physical appearance, which hinders psychological intervention (12). They are constantly afraid of negative evaluations. However, ICBT is an online psychological intervention that does not need the physical presence of the patients who might be afraid of negative evaluations. The patient can anonymously benefit from psychological services. This is a unique feature of this form of therapy (15). Besides, CBT also allows overweight and obese people to modify their eating behaviors and teach their minds to make a mental image of a thin person of themselves. This approach also helps people to choose a desirable diet and stabilize their weight by adopting mental and emotional strategies (28). The high impact of ICBT interventions can be due to therapists' feedback during the treatment process. In this study, in comparison with the research on internet treatment programs, the therapist was present with the patient every day. Therefore, it seems that this type of treatment has the most therapeutic effect among internet-based therapies. In this study, using WhatsApp cyberspace, the therapist increased the likelihood of clients doing homework by sending daily reminders and monitoring the execution of assignments daily. In addition, the ability of the therapist to share the homework results in the group and receive feedback from the therapists and other people in the group was one of the factors that increased the likelihood of homework. This issue also justifies the effectiveness of ICBT in reducing BMI.
The results of the analysis of covariance of stress, anxiety, and depression after the intervention in the three groups showed that there was no statistically significant difference between the ICBT, TAU, and WL groups. However, due to the low observed power in stress, anxiety, and depression changes, the test is not accurate enough to detect significant differences, and the data should be interpreted with caution. These findings are not consistent with the findings of the study by Ebert et al., who showed the effectiveness of computer- and internet-based CBT in treating anxiety and depression symptoms in young people. They argued that computer- and internet-based CBT is a promising tool when the feasibility of evidence-based face-to-face CBT is questionable (20). Tham and Chong reported the effectiveness of ICBT in reducing stress, anxiety, and depression (21). Waite et al. also did not find promising results concerning the effectiveness of ICBT in the intervention group compared to the waiting list group (22). Wright et al. also showed the ineffectiveness of this form of therapy in children with anxiety (31). Evidence on the relationship of anxiety and depression with obesity was not promising. A positive relationship was found between anxiety/depression and being overweight. Another study in China showed a higher prevalence of depressive and anxiety symptoms in children and adolescents with overweight and obesity (23). Another study showed that young adults who met the criteria for a depressive/anxiety disorder were almost 2.5 times as likely to be obese (32). However, no significant relationship was found between anxiety/depressive symptoms and obesity. The logistic regression analysis showed that anxiety and depression variables could not predict obesity and overweight (33).
The ICBT intervention could not significantly reduce anxiety and depression because of the COVID-19 pandemic in this study. Yang et al. also reported an increase in psychological disorders due to the COVID-19 pandemic, especially a dramatic increase in the incidence of anxiety, depression, and mental disorders in the general population (34). The daily pursuit of news on the COVID-19 pandemic increases the risk of depression and anxiety in people (35). These are similar to the clinical symptoms of anxiety and depression. Concerns about the risk of illness, future employment status, the income of the people and their families, and prolonged self-quarantining also increase the risk of psychological symptoms, including despair and hopelessness (36). It was recommended to follow a healthy diet during the pandemic, which often people misinterpreted as no control over their weight. It was rumored that obesity boosts the immune system; nevertheless, Milner and Beck showed that obesity weakens the immune system (37). A rigid dichotomy between obesity and normal weight during the pandemic increased the risk of anxiety and stress, although people controlled their weight. The COVID-19 pandemic has also increased the incidence of anxiety worldwide. Fear of death justifies human behaviors during the crisis (38). Besides, ICBT was found to be ineffective in reducing stress, anxiety, and depression because of the persistence of these symptoms that cannot be treated with short-term therapy (six weeks). A few sessions were devoted to stress, anxiety, and depression, which necessitate the inclusion of more sessions to address these issues. There is also the possibility of incoherent implementation of ICBT in six months due to the online format of the therapy. This issue justifies the ineffectiveness of ICBT in reducing stress, anxiety, and depression.
5.1. Conclusions
The results showed that both ICBT and TAU significantly reduced body mass index with women with BMI ≥ 25, but there was no overall significant difference between in three groups in decreasing stress, anxiety and depression. Thus, the results in these cases should be interpreted with caution. Also, since internet-based cognitive-behavioral therapy is as effective as diet method, counselors, clinical psychologists and therapists can use ICBT method as an affordable, low-cost, practical and effective method for people with obesity.
5.2. Limitations
One of the limitations of this study was the use of self-report tool of the questionnaire, the sample size was limited to Neishabour city and its implementation coincided with the outbreak of Corona virus. In the participant selection phase, a number of individuals withdrew from the study despite their desire to participate in treatment due to concerns about using or connecting to the internet. It was not possible to control some variables, including the motivation of participants in recovery and active role in the group. Also, low test power in variables of stress, anxiety and depression, which in cases of results should be interpreted with caution.