1. Background
Inference based approach (IBA) was introduced by O'Connor and Robillard (1) in order to conceptualize obsessive-compulsive disorder (OCD) more thoroughly. The main component of this approach is a kind of reasoning style called “inferential confusion” (IC). According to IBA, pathological doubts are at the core of obsessions formed through IC. Investing in remote possibilities as well as the distrust of the senses are two main components of IC leading one to construct a mental narrative about the possible state of affairs (2). In other words, people with OCD mix the probability with reality and then act as if the probability is true (1). According to this approach, it is assumed that patients with OCD feel anxious due to the fact that they have an imperfect test of reality. If they manage to integrate sensory information properly, they experience no anxiety (3).
According to IBA, OCD is an imagination disorder characterized by pathological doubt (4). Imagination also has an important role in delusional disorders (DD), in which beliefs deviate from reality (5). Delusions are defined as false beliefs despite evidence to the contrary (6). Research findings have shown that the experience of delusions lies on a continuum. Claridge et al. (7) used the term schizotypy to define non-clinical delusional types of belief.
Several studies have detected a potential connection between schizotypal and obsessive-compulsive symptoms (OCS) in OCD patients (8-11) and non-clinical samples of students (12, 13). However, no clear explanation has been offered for the relationship between schizotypy and OCS. According to the IBA, IC is one of the structural similarities recognized between OCS and schizotypy. IBA suggests that many schizotypal symptoms can be explained at the end of the IC process spectrum, where reality and imagination are confused. At that point, the individual is, to some extent, far away from the reality and may have perceptual experiences that are dissociative by nature (14, 15). Proponents of IBA believe that IC might have an underlying role in the occurrence of DD and OCD and suggest that both disorders are belief disorders (16).
Aardema et al. (15) investigated the relationship between IC, OCS, and schizotypy in a normal sample and discovered significant relationships between both IC and schizotypal symptoms scores with scores of OCS. After controlling neuroticism, moreover, they found that the relationship of IC with schizotypal symptoms and OCS remained significant. Their findings from multiple regression analysis indicated that both IC and schizotypal symptoms were capable of predicting a significant variance of OCS after controlling neuroticism.
O'Connor and Aardema (17) argue that low imaginative absorption threshold and an excessive dependence on inductive reasoning may play a role in occurrence of inferential confusion. Evidence from research findings shows that dissociative experiences are among the factors that can predispose individuals to the inferential confusion. For example, research findings have determined that dissociation can disrupt information processing (18) and reduce an individual's confidence in their ability to monitor reality (19). As a result, it reduces his/her confidence in the sensory information. Also, dissociative absorption may immerse the individual in the fantasy world and, therefore, distance him/her from the reality of the here and now. This, in turn, reduces his/her attention to the facts and makes him/her prone to investing in unlikely possibilities (5, 20). Also, research evidence has supported the role of a tendency to absorb and immersion into fantasies in the development of OCD symptoms (17) and delusional disorders (5). According to this common component, therefore, the relationship between OCS and schizotypal traits can be explained to some extent. Furthermore, dissociation has been recognized as one of the imaginary processes involved in OCS (21) and schizotypal traits (22). On the other hand, there are likely conceptual similarities between IC and dissociation (16).
Aardema and Wu (5) showed that immersive tendencies, imaginative process, and schizotypal personality traits were associated with OCS. They also indicated that IC and absorption were the most consistent predictors of OCS after controlling NA. Paradisis et al. (21), by investigating a clinical sample, revealed that IC, dissociation, and schizotypal personality traits were interrelated. Moreover, IC and dissociation were the strongest predictors of OCS, which was consistent with the findings from the study by Aardema and Wu (5). This finding was also confirmed after controlling the negative mood states and obsessive beliefs.
Before our study, the important role of dissociative, schizotypal, and imaginative processes in occurrence of OCS had been highlighted in the literature; however, no precise explanation had been offered for the role of imaginative processes in the relationship between OCS and schizotypy. Furthermore, previous studies had mainly focused on calculating the correlation or regression coefficients between these variables. Therefore, combining these components to form a single model may have provided a better understanding of the relationship between these variables. Since part of the relationship between these variables may have been due to the negative affect (NA), moreover, an attempt was needed to make in order to partially control it by incorporating this variable into the model. It should be noted that the novelty of the present study lies in the fact that it is a preliminary step toward identifying the factors affecting the vulnerability of individuals into IC as a reasoning style and, in this regard, proposing a model about the effect of dissociative experiences on the relationship between OCS and schizotypal personality traits by considering the mediating role of IC and moderating role of NA.
2. Objectives
This study mainly aimed to investigate the relationships among the following variables: (1) dissociative experiences and obsessive-compulsive symptoms; (2) dissociative experiences and schizotypal traits; (3) dissociative experiences and inferential confusion; (4) inferential confusion and obsessive-compulsive symptoms; (5) inferential confusion and schizotypal traits; (6) obsessive-compulsive symptoms and schizotypal traits. Furthermore, it aimed to answer the question of whether or not the negative affect played a moderating role in the given relationships? And if the inferential confusion mediated the relationship between dissociative experiences with obsessive-compulsive symptoms and schizotypal traits?
3. Methods
3.1. Participants
In this cross-sectional study, 341 B.A. and M.D. students (183 female and 158 male) spending their first semester of 2017 - 18 academic year were selected. The participants were in the 18 - 29 age range (M = 20.05, SD = 1.96). The sample size was determined based on the opinions from experts in the field of structural equation modeling (SEM). There are different views on the sample size in SEM. The minimum sample sizes proposed by Kline (23) and Loehlin and Beaujean (24) are 200 and 100, respectively; however, Hooman (25) and Loehlin and Beaujean (24) considered 300 and 200 as more appropriate sample sizes. The students were selected by adopting cluster sampling method through random selection of faculties and classes and by considering the number of students in each faculty – the sample size ratio of Shahed University’s central campus. Distributing questionnaires and collecting data were performed by the main researcher. The objectives of the research, the confidentiality, and anonymity of questionnaires, as well as how to complete them were all briefly explained to the students by the researcher attending the selected classes. Then the questionnaires were distributed among the students, and those willing to participate in the research were asked to complete them. Thus, ethical standards such as ensuring the confidentiality of participants' information, obtaining an informed consent, and granting permission to withdraw from the research were all followed. Informed satisfaction as well as having no serious physical and psychiatric disorders were the inclusion criteria, whereas dissatisfaction and having serious physical and psychiatric disorders were the exclusion criteria.
3.2. Measures
3.2.1. Dissociative Experiences Scale (DES-II)
This questionnaire includes 28 items that are rated on an 11-point scale of 0% to 100%, from ‘never happens to me’ to ‘always happens to me’, increased by increments of 10. DES-II can be used to assess dissociative experiences in clinical and non-clinical groups (26). The mean score of 28 items constitutes the total score to achieve a score ranging from 0 to 100. Absorption and imaginative involvement (AB), amnesia (AM), and depersonalization/derealization (DEP/DER) are three subscales of DES-II. It has shown very good or excellent internal consistency (0.85 ≤ α ≤ 0.93) (26) and strong correlations with other dissociation measures (27). Kianpoor et al. (28) reported good internal consistency (α = 0.96) and test-retest reliability (r = 0.96, P < 0.001) for the Persian version of DES-II.
3.2.2. Obsessive-Compulsive Inventory-Revised (OCI-R)
The OCI-R (29) is a short form of OCI (30) which has 18 items and 6 subscales (obsessing, washing, mental neutralizing, checking/doubting, hoarding, and ordering). The items are scored on a scale of 0 to 4. The internal consistency and test- retest reliability of OCI-R were determined by Hajcak et al. (31) in a non-clinical sample. They reported an excellent internal consistency (0.88) for OCI-R total scale and moderate to good internal consistency for subscales ranging from 0.61 - 0.84. The test-retest reliability for a 4-week interval was obtained 0.70 for total score, and the ones for subscales were reported to range from 0.54 to 0.77, indicating good to excellent test-test reliability.
As for the Persian version of OCI-R, Ghassemzadeh et al. (32) reported high test-retest reliability (r = 0.75 for total scale, and 0.62 ≤ r ≤ 0.76 for subscales). Also, Alpha coefficient was reported to be 0.85 for total score, and the ones for subscales were detected to range from 0.77 to 0.86, demonstrating extremely high internal consistency.
3.2.3. Schizotypal Personality Questionnaire-Brief (SPQ-B)
This questionnaire consists of 22 items and 3 subscales: (1) the cognitive-perceptual dysfunction factor; (2) the interpersonal deficits factor; and (3) the disorganization factor (33). Scoring is dichotomous with yes/no answers. Therefore, the highest possible score is 22, and the lowest score is zero; and as the scores increase, the levels of schizotypal symptoms also increase. It has been discovered that SPQ-B has good psychometric properties. As for the subscales, Alpha coefficients (0.72 ≤ α ≤ 0.80) and test–retest reliability coefficients (0.86 ≤ r ≤ 0.95) have been reported to be good. Calculating the correlation coefficient between scores of SPQ-B and DSM-III-R based clinical interview for schizotypal traits has confirmed its criterion validity (33).
Mohammadzadeh (34) reported good internal consistency for total score (α = 0.83) and subscales (0.66 ≤ α ≤ 0.70) of the Persian version of SPQ-B. In addition, the test-retest reliability for total score was 0.94, and the ones for subscales were reported to range from 0.83 to 0.90. All of these coefficients were significant and showed high test-retest reliability.
3.2.4. Inferential Confusion Questionnaire-Expanded Version (ICQ-EV)
ICQ-EV is a self-report questionnaire for measuring IC and contains 30 items (35). Items are scored on a scale from strongly disagree (1) to strongly agree (6). Internal consistencies using Cronbach’s alpha have been reported to be 0.97 and 0.96 in clinical and non-clinical samples, respectively. Twelve-week interval test-retest reliability coefficient was 0.90 (P < 0.001) in OCD group. Furthermore, strong correlations observed between ICQ-EV and OCD symptoms independent of other cognitive domains and general distress have confirmed the convergent validity (35).
The psychometric properties of ICQ-EV Persian version were demonstrated by Ghorbali et al. (36). Their findings supported the internal consistency (α = 0.95) and test-retest reliability (r = 0.9, P < 0.001). Convergent and divergent validity of this scale were satisfactory.
3.2.5. Positive & Negative Affect Scales (PANAS)
This questionnaire contains 20 items and has two scales designed to measure positive and negative affect. Each one of the scales consist of 10 words, and the respondents answer them based on a 5-point Likert scale from 1 to 5. Both subscales have shown good internal consistency (α = 0.88 for positive affect and α = 0.87 for negative affect). The test-retest reliability for a 2-month interval were determined to be 0.68 for and 0.71 for PA and NA, respectively, indicating satisfactory test-retest reliability. The PANAS questionnaire has shown adequate indicators of convergent and discriminant validity (37).
The psychometric properties of PANAS Persian version were demonstrated by Bakhshipour and Dezhkam (38). The scales have been detected to be internally consistent considerably. Moreover, factorial and construct validity of this scale have been found satisfactory (38). In this study, only the sub-scale of negative emotion was used.
It should be noted that all of the scales adopted in this study showed internal consistency values between 0.77 and 0.93.
4. Results
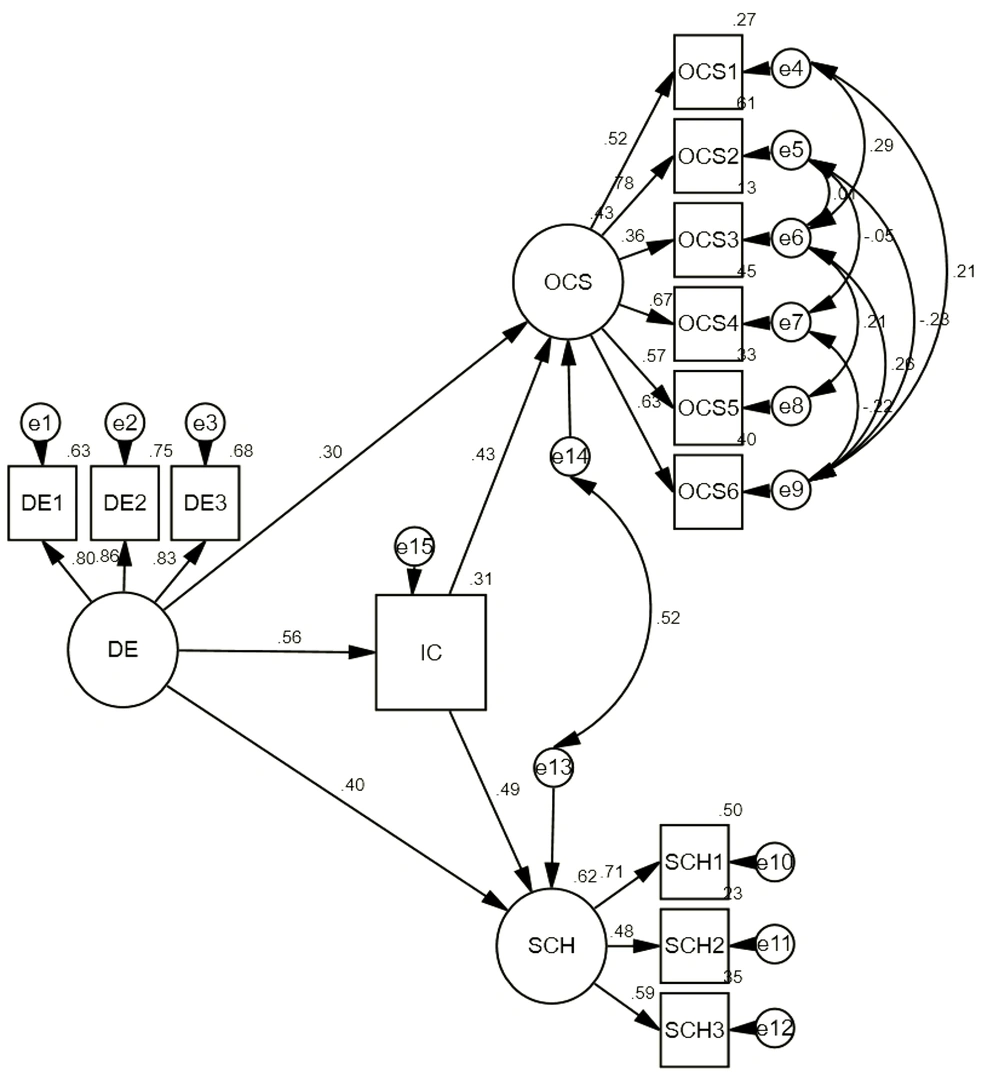
Data were analyzed using IBM SPSS-22 and Amos-18. The mean and standard deviation for each study measure and correlation coefficients between variables are shown in Table 1. Results showed that all of the correlation coefficients were significantly positive. The proposed model adopting dissociative experiences as a predictive variable, IC as a mediating variable, and OCS and schizotypal personality traits as dependent variables was examined. According to assumptions underlying SEM, all questionnaire scores were checked for missing data, outliers, and normality before performing the analysis. The results of the SEM investigation indicated that the proposed model had goodness of fit, and all Goodness-of-Fit indexes were good: χ2/df = 1.85 (< 3) and RMSEA = 0.05 [CI (90%) = 0.03 - 0.06]. GFI, AGFI, and CFI were 0.95, 0.92, and 0.97, respectively, and all of them were above 0.9. The final model and standard path coefficients are displayed in Figure 1. All the coefficients were statistically significant (P < 0.001). Therefore, it was argued that dissociative experiences may have affected the OCS and schizotypal personality traits directly and indirectly (through IC).
Abbreviation: SD, standard deviation.
a P < 0.001.
Next, multi-group analysis was performed to investigate the moderating role of negative affect. To this end, the sample was divided into three groups with high, moderate, and low negative affect based on the standard deviation of this variable. Then, the fitness of the proposed model was examined in each one of the three groups. As shown in Table 2, the proposed model had Goodness-of-Fit in all three groups. The difference between the chi-square value in constrained and unconstrained model was then investigate. Adopting this method facilitated comparing the degree of the proposed model’s equality in the three groups. When the factor loadings, variances, and covariances in the model were equal in different groups, the model was assumed to be constrained. To create a constrained model in AMOS software, an equal parameter was specified for groups with a label. Thus, any unlabeled parameter was freely estimated. As a result, unlabeled parameters were freely estimated and may have had different values in groups (39). The results showed that the improvement of chi-square from the original unconstrained model (200.57) to the constrained model (255.17) was significant (54.60 > 48.28) due to the chi-square distribution table (χ2 = 48.28, df = 28, P = 0.01). Therefore, the moderating role of negative affect was confirmed. Then, further investigation was performed in order to determine the different path coefficients in the three groups. According to Byrne (39, 40), the coefficients important for the researcher were assumed to be equal in all three groups first by forming different constrained models, and then the chi-square index in each one of these constrained models was compared with the unconstrained model. The results of the comparisons are shown in Table 3. As shown, the chi-square difference between model A and the original unconstrained model was statistically significant (∆χ2 = 21.22, ∆df = 12, P = 0.04). These findings suggested that at least one of the paths in the model was not equal in different groups. As indicated in Table 3, findings revealed that only the chi-square difference between constrained model E and the unconstrained model (model 1) was statistically significant (∆χ2 = 7.82, P = 0.02) among all models. This finding implied that only the IC path on OCS, among the paths in the model, was moderate by NA. As shown in Table 4, the standard regression coefficient of this path was reduced by increasing the NA, but this path was still significant in all three groups.
| Groups | Indexes | ||||||
|---|---|---|---|---|---|---|---|
| χ2 | df | χ2/df | GFI | AGFI | CFI | RMSEA (90% CI) | |
| Low negative affect | 45.32 | 52 | 0.87 | 0.90 | 0.89 | 1.00 | 0.0001 (0.0001 - 0.06) |
| Moderate negative affect | 86.29 | 52 | 1.65 | 0.94 | 0.9 | 0.96 | 0.05 (0.03 - 0.07) |
| High negative affect | 68.44 | 52 | 1.31 | 0.90 | 0.91 | 0.92 | 0.06 (0.0001 - 0.06) |
| Models | Comparison | χ2 | df | Δχ2 | Δdf | P-Value |
|---|---|---|---|---|---|---|
| 1. Original unconstrained model: No equality constraints imposed | - | 200.57 | 156 | - | - | - |
| 2. A model: All of the following paths constrained equal: DE on OCS; DE on IC; DE on SCH; IC on OCS; IC onSCH; OCS & SCH covariance | A versus 1 | 221.79 | 168 | 21.22 | 12 | 0.04 |
| 3. B model: The path of DE on OCS constrained equal | B versus 1 | 203.76 | 158 | 3.19 | 2 | NS |
| 4. C model: The path of DE on IC constrained equal | C versus 1 | 204.87 | 158 | 4.01 | 2 | NS |
| 5. D model: The path of DE on SCH constrained equal | D versus 1 | 204.39 | 158 | 3.82 | 2 | NS |
| 6. E model: The path of IC on OCS constrained equal | E versus 1 | 208.39 | 158 | 7.82 | 2 | 0.02 |
| 7. F model: The path of IC on SCH constrained equal | F versus 1 | 204.52 | 158 | 3.95 | 2 | NS |
| 8. G model: The covariance between OCS & SCH constrained equal | G versus 1 | 204.59 | 158 | 4.02 | 2 | NS |
Abbreviation: NS, not significant.
| Groups | B a | SE | β b | P-Value |
|---|---|---|---|---|
| Low negative affect | 0.01 | 0.004 | 0.48 | < 0.001 |
| Moderate negative affect | 0.01 | 0.004 | 0.30 | < 0.001 |
| High negative affect | 0.01 | 0.004 | 0.23 | < 0.001 |
Abbreviation: SE, standard error.
a Unstandardized regression coefficient.
b Standardized regression coefficient.
5. Discussion
This study aimed to examine the fitness of the proposed model about the effect of dissociative experiences on the relationship between OCS and schizotypal personality traits by considering the mediating role of IC and controlling the NA in a non-clinical sample. As predicted, the results of the SEM investigation indicated that the proposed model had goodness of fit. Therefore, the mediating role of IC in the effect of dissociative experiences on the relationship between OCS and schizotypal personality traits was confirmed. Findings related to the moderating role of NA showed that among all paths in the model, only the IC path to OCS was moderate by NA.
Findings showed that dissociation, schizotypy, IC, and OCS were significantly interrelated. These results were consistent with the findings from previous studies (5, 14-16, 21, 27). IBA attempts to describe the relationship between OCD and schizotypy. According to the IBA model, the tendency to distrust sensory-based information and inference based on purely subjective information is a common feature between these two disorders. This idea is supported by the fact that previous studies have failed to find a significant difference between the two groups of people with delusional disorder and OCD regarding the IC scores (41). Research has also shown that there is a relationship between IC and cognitive-perceptual distortions and delusional thinking that are symptoms of schizotypy (41). Seemingly, people with OCD have no difficulty in perceiving reality. Thus, the conceptualization of the relationship between OCS and perceptual deficits is somewhat unclear. O’Connor et al. (42) have suggested that the perceptual disturbances in patients with OCD can be explained by IC. One of the main components of IC-based thinking is distancing from reality and dependence on imagination, which causes certain disturbances in the perception of reality (42). As discussed earlier, dissociation is one of the related types of imaginary process associated with OCD symptoms and schizotypal personality traits. Dissociation disrupts the integrated functions of perception, consciousness, identity, and memory (6). This lack of proper integration of information into reasoning is also seen in the IC process. Also, IC and dissociation both involve elements of engaging with one’s imagination (43). Dissociation can immerse the individuals experiencing IC in imagination and keep them away from the realities that exist here and now. Thus, one is confused between an imaginary probability and a real probability and, ultimately, acts on that imaginary probability (20).
Results from investigating the moderating role of NA showed that there was a relationship between IC and OCS in different levels of NA (low, moderate, and high). As the NA increased, however, the power of this relationship reduced. This may indicate that when negative affect exceeds what is commonly associated with OCS, the distance from obsessive-compulsive spectrum disorders becomes greater, and we become more prone to the mood and anxiety disorders that have a nature different from that of obsessive-compulsive spectrum disorders. In fact, when mood and anxiety disorders overcome obsessive-compulsive disorders, it is no longer surprising that the relationship between IC and OCS is weakened. In line with this finding, Aardema et al. (41) have shown that IC is more common in people with OCD than those with other anxiety disorders.
This study faced some limitations. First, the current study was a cross-sectional study and, therefore, longitudinal studies were needed to investigate the causal relationships between the variables. Second, this study was performed on a non-clinical student sample and, therefore, its results were not generalizable. Third, adopting self-report measures to assess all variables was another limitation of this study. Therefore, it was suggested that this study should be repeated on a group of clinical individuals experiencing symptoms of OCD and schizotypy at the same time in order to gather more research evidence to support the obtained findings. Moreover, it was recommended that other complementary methods (e.g., using clinical interviews and other questionnaires) should be adopted to collect data, and that experimental designs should be applied to infer the causal role of dissociation and inferential confusion in OCD and schizotypy.
5.1. Conclusions
According to the findings from the examined model, the notion of inferential confusion as a trans-diagnostic construct in explaining the underlying reasoning processes behind both obsessive-compulsive spectrum disorders and delusional disorders, as well as the potential role of dissociation in inferential confusion, were confirmed. Moreover, our study results supported the classification of obsessive-compulsive disorder as a belief disorder. Our findings may have developed the basic knowledge about obsessive compulsive disorder and its relation with schizophrenia spectrum disorders and, subsequently, helped the therapists design a more effective therapeutic program for these patients.