1. Background
Diabetes is a complex metabolic disorder caused by a variety of reasons, leading to chronic hyperglycemia due to insufficient insulin secretion (1). This disease is divided into several categories: type 1 or insulin-dependent diabetes, type 2 diabetes, and gestational diabetes (2, 3). Type 2 diabetes is characterized by high blood sugar levels due to ineffective use of insulin by the body and has a prevalence of about 1.3% to 14.5% in different parts of Iran, highlighting it as one of the most common chronic diseases in the country (4). There are 382 million people with diabetes in the world, of whom nearly 90% have type 2 diabetes (5). Type 2 diabetes is one of the most complex diseases in terms of disease management and the need for self-management. Because it is a lifelong disease, patients need to take special precautions to control blood and prevent short-term and long-term complications (6).
Blood sugar control is directly related to self-care behaviors, meaning the active participation and cooperation of the patient in self-care activities (including taking medications on time and with the correct prescribed dose, adopting an appropriate diet, doing exercise, blood glucose control, and foot care) on a daily and continuous basis (7, 8).
Moreover, studies have shown that self-care activities lead to stable blood sugar levels and improve quality of life, which is another important indicator of health in these patients. According to the World Health Organization, quality of life is described as a person’s personal perception of his life situation according to the culture and value system of society and also its relationship with his goals, expectations, standards, and needs (9, 10). Any decrease in quality of life not only affects patients’ happiness but also influences adherence to medical and treatment recommendations, including self-management activities and medication use (11).
People with diabetes need to integrate therapeutic indicators into their lives in order to achieve optimal blood sugar levels; however, few patients adhere to recommended health behaviors (12, 13). Meanwhile, some studies have examined the impact of social and psychological factors on diabetes (14). Paying attention to psychological variables in diabetic patients can improve tolerance and adherence to treatment, quality of life, and lifestyle (15). In addition to self-care and quality of life, another strong predictor of patient performance and diabetes health promotion is the ability to regulate emotions (16).
The structure of emotion regulation as a multidimensional structure refers to the following: (A) awareness, which is the perception and acceptance of pleasant and unpleasant emotions; and (B) participation in directional activities and prevention of impulsive behaviors when experiencing unpleasant emotions (16, 17). According to the above definition, the purpose of emotion regulation is to emphasize the control of emotion-induced behaviors instead of completely eliminating unpleasant emotions (18).
The effectiveness of acceptance-based psychological therapies in improving the quality of life and physical characteristics of patients with diabetes (19) and its effects on the biomarkers of this disease (20, 21) have been proven in the past. In the present study, we intended to investigate the effects of acceptance-based emotion regulation group therapy on disease control indicators in patients with diabetes.
2. Objectives
According to the above-mentioned and considering the increasing prevalence of diabetes, there is a need to find effective and short-term therapies by combining effective therapeutic elements with existing approaches to control diabetes. The effectiveness of acceptance-based therapies in improving the quality of life and clinical indicators of patients (19) and their effects on the biomarkers of the disease (20) have been previously reported in patients with diabetes. Therefore, the aim of this study was to investigate the effectiveness of acceptance-based emotion regulation group therapy in improving disease control indicators in patients with type 2 diabetes.
3. Methods
3.1. Study Setting and Selection Criteria
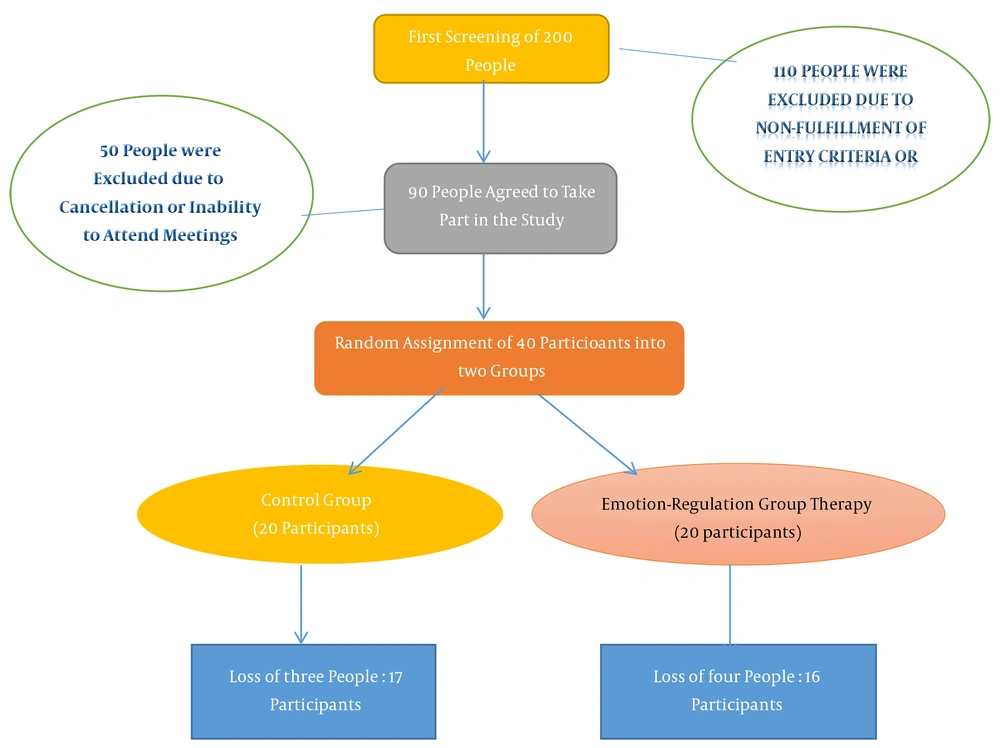
The present interventional study included the pre-test, post-test, and follow-up phases, as well as a control group, and used a simple randomized sample population. The study was conducted between November 2019 and July 2020. The Ethics Committee of Iran University of Medical Sciences (code: ID: IR.IUMS.REC.1398.760) approved this study. The study population consisted of 198 patients with type-2 DM registered in the Iranian Diabetes Association. The sample size was calculated by Power Analysis (G*Power). The total number of patients for both groups was regarded as 40, considering a probability of losses during the study.
Inclusion criteria were the diagnosis of type 2 diabetes by an endocrinologist, an age range of 35 to 65 years (since type 2 diabetes is generally diagnosed in adulthood, and the fact that the age range of 35 to 65 years, according to endocrinologists, is the most common period at which patients visit endocrinologists), treatment under the supervision of an endocrinologist, and having a medical record in the Iranian Diabetes Association. The exclusion criterion was the diagnosis of either type 1 diabetes, gestational diabetes, or severe psychiatric disorder. Among those who were willing to participate in the study (with written consent), forty patients were selected and randomized to two groups of 20: The intervention (receiving diabetes medications and acceptance-based emotion regulation group therapy) and control (receiving diabetes medications) groups. It should be stated that four patients in the intervention group and three patients in the control group discontinued during the study. In order to comply with ethical principles, before the intervention, the patients were assured of confidentiality and asked to sign an informed consent to participate in the research (Figure 1). In the implementation and data collection stages, the subjects’ information was kept confidential. Data were collected and then analyzed using SPSS 21 software.
In this study, acceptance-based emotion regulation group therapy was considered as the independent variable, and self-care, quality of life, and glycosylated hemoglobin (HbA1c) were dependent variables.
3.2. Intervention
The pre-test and post-test stages were performed in the first and last group therapy sessions, respectively. Also, the follow-up stage was performed after six months of the last group therapy session, during which the participants completed the questionnaires of this stage and underwent the blood sugar measurement test. All interviews and briefings were conducted by one of the researchers before starting group therapy sessions and were not repeated in other stages of the study.
Acceptance-based emotion regulation group therapy was performed in 14 sessions per week, and each session lasted for two hours once a week. The therapy combined the aspects of acceptance and commitment therapy (22), dialectical therapy (23), and emotion-centered therapy (24). In the first week, the function of self-harming behaviors was discussed. In the second to sixth weeks, emotional awareness was identified and boosted. In the seventh and eighth weeks, the results of emotional avoidance became clear to the clients, and the clients realized that not accepting and avoiding emotions would create and intensify unpleasant emotions. In the ninth and tenth weeks, the emphasis was on strategies to avoid emotions in order to reduce the intensity and duration of emotional responses. In the tenth week, strategies for controlling impulsive behaviors were developed. Finally, in the eleventh to fourteenth weeks, the emphasis was on identifying and creating life values for purposeful orientation, and the clients were encouraged to be engaged in value-oriented behaviors.
3.3. Statistical Analysis
Descriptive statistics (frequency, mean, percentage, and standard deviation) and mixed-design ANOVA were used to describe and analyze the data.
3.4. Data Collection
3.4.1. Diabetes Self-care Summary Questionnaire
The 25-item self-report index of self-care activities is one of the most reliable tools available to assess the self-care activities of diabetic patients, assessing the status of the diet, exercise, blood sugar testing, foot care, and smoking in patients. The results of a meta-analysis showed that this scale had a good validity and reliability (25), and its Cronbach’s alpha coefficients in an Iranian population were 0.95, 0.95, 0.84, and 0.74 for the whole scale and weekly, monthly, and annual subscales, respectively, indicating the acceptable internal consistency of this scale (26).
3.4.2. Diabetes Dependent Quality of Life Scale
This 19-item scale is designed to measure the quality of life of people with diabetes and shows how much each aspect of diabetes has affected the patient’s life. This scale has a good validity and reliability. Vickery reported the internal consistency and reliability coefficients of 19 scales of this questionnaire, administered to 179 patients with diabetes, to be between 0.75 and 0.96, reflecting the optimal reliability of this questionnaire (27). In this research, the Persian version of the scale was utilized. Moreover, Ghaem et al. (28) reported the internal consistency and reliability of the scales of this questionnaire to be between 0.65 and 0.94 and the total reliability to be 0.96, using Cronbach’s alpha coefficient.
3.4.3. HbA1c Assay
Glycosylated hemoglobin is a blood test that shows a person’s average blood sugar over the past two to three months, and its level directly depends on blood glucose concentration. The normal range of HbA1c in healthy individuals is 4% to 6%, and the American Diabetes Association (2014) has set a value below 7% for proper management of diabetes, with a high HbA1c level indicating poor blood sugar control (29).
3.4.4. Structured Clinical Interview DSM-V for Mental Disorders
The DSM-V Structured Clinical Interview for Mental disorders (SCID-I) is a semi-structured interview reviewed in 2014 to assess mood disorders, psychotic disorders, anxiety disorders, substance abuse disorders, obsessive-compulsive disorders, and other related disorders, as well as eating disorders, physical symptom disorders, a number of sleep disturbances (such as insomnia and hypersomnia), external disorders, and other disorders related to trauma and stressors. In a recent study, the reliability of the scale for six disorders was reported to be optimal (range: 0.76 to 0.1), and for other disorders, the range was between 0.57 and 0.65 (30).
4. Results
Demographic and clinical characteristics of 33 patients with type 2 diabetes have been reported in Table 1. The results of descriptive statistics showed that there was no significant difference between the experimental and control groups in terms of demographic and clinical indicators. All of the continuous variables measured in this study were normally distributed. Moreover, Table 2 summarizes the descriptive statistics of the pre-, post-, and follow-up tests in the two groups.
| Socio-Demographic Characteristics | Intervention Group | Control Group |
|---|---|---|
| Age, mean (SD) | 52.15 (3.20) | 53.55 (3.19) |
| Marital status | ||
| Married | 13 (81) | |
| Widowed divorced | 3 (19) | 16 (98) |
| Education status | ||
| Uneducated | 0 (0) | 0 (0) |
| High school | 3 (19) | 5 (29) |
| College and above | 13 (81) | 12 (61) |
| Working status | ||
| Yes | 6 (37) | 6 (35) |
| Retired | 10 (63) | 11 (65) |
| Diabetes diagnostic duration, mean (SD) | 9.84 (4.12) | 8.16 (4.88) |
aValues are expressed as No. (%) unless otherwise indicated.
| Factor | Emotion Regulation, Mean (SD) | Control, Mean (SD) |
|---|---|---|
| HbA1c | ||
| Pre-test | 7.89 (2.14) | 8.36 (1.96) |
| Post-test | 6.80 (1.65) | 8.67 (2.19) |
| Follow | 6.90 (1.78) | 9.66 (2.32) |
| Self-care | ||
| Pre-test | 65.03 (12/23) | 62.25 (12.04) |
| Post-test | 73.64 (12/49) | 68.43 (11.55) |
| Follow | 83.07 (12.77) | 66.78 (11.13) |
| Quality of life | ||
| Pre-test | -9.28 (2.01) | -8.50 (1.13) |
| Post-test | 1.78 (1.66) | -10.30 (1.53) |
| Follow | 0.27 (1.43) | -8.50 (1.32) |
Mixed-design ANOVA was used to assess the effectiveness of the therapy in improving disease control indicators in patients with type 2 diabetes by comparing the study outcomes between the control and intervention groups (Table 3).
| Variable | Df | Mean Square | F/P | Partial π2 | ||
|---|---|---|---|---|---|---|
| Time | Group | Time × Group | ||||
| HbA1c | 3.19 | 5.76 | 3.19 (0.04) | 9.00 (0.006) | 17.52 (0.0001) | 0.40 |
| Self-care | 1 | 330.041 | 4.95 (0.01) | 8.44 (0.009) | 2.50 (0.09) | 0.20 |
| Quality of life | 1 | 412.57 | 2.63 (0.04) | 2.81 (0.02) | 2.35 (0.13) | 0.23 |
In order to investigate the assumptions required to perform statistical tests, the normality of the distribution was investigated using the Shapiro-Wilk test. The results of the test showed that the obtained values regarding the distribution of the variables were not significant at the level of P ≤ 0.05, indicating their normal distribution. The difference of variance-covariance matrix in different tests was investigated using the Mauchly test. The amount of the chi-square obtained was significant at the level of P ≤ 0.05, and due to the heterogeneity of the matrix, corrected coefficients were used. The Levin test for equality of variances (P > 0.05) showed that the variances of the two groups were equal. The results of analyzing the intra- and inter-group effects have been shown in Table 3.
According to Table 3, the impact of the group × time interaction on HbA1c (P = 0.0001, F = 17.52), self-care activity (P = 0.09, F = 2.50), and quality of life (P = 0.13, F = 2.35) was statistically significant. As a result, it can be stated that the intervention led to a difference between the experimental and control groups. In addition, the ETA coefficient obtained showed that the intervention could predict 0.40, 0.20, and 0.23 of changes in HbA1c, self-care activities, and quality of life, respectively. Then two-way comparisons for between- and within-group differences were performed using the Bonferroni test.
Table 4 demonstrates that the mean difference between the pre-test and post-test phases in the experimental group was significant for HbA1c (P = 0.001), quality of life (P = 0.0001), and self-care (P = 0.001). However, the mean difference between the post-test and follow-up phases was not significant for HbA1c (P = 0.17) and quality of life (P = 0.27) in the experimental group, indicating the stability of the therapeutic effect for up to six months after the intervention.
| Intervention | Control | |||
|---|---|---|---|---|
| Mean Difference | P-Value | Mean Difference | P-Value | |
| Pre-test and Post-test | ||||
| HbA1c | -1.09 | 0.001 | 0.31 | 0.11 |
| Self-care | 8.16 | 0.001 | 6.17 | 0.07 |
| Quality of life | 11.06 | 0.0001 | -1.45 | 0.28 |
| Pre-test and Follow up | ||||
| HbA1c | -0.99 | 0.001 | 1.30 | 0.001 |
| Self-care | 18.04 | 0.0001 | 4.53 | 0.15 |
| Quality of life | 9.55 | 0.001 | 0.35 | 0.051 |
| Post-test and Follow up | ||||
| HbA1c | 0.10 | 0.17 | 0.99 | 0.001 |
| Self-care | 9.43 | 0.0001 | -1.65 | 0.32 |
| Quality of life | -1.51 | 0.27 | 1.80 | 0.44 |
5. Discussion
The aim of the present study was to evaluate the effectiveness of acceptance-based emotion regulation group therapy in improving disease control indices in patients with type 2 diabetes, a disease that is highly prevalent in Iran (a prevalence of about 1.3 to 14.5%). Our results showed that the intervention in the experimental group led to a significant decrease in HbA1c level and a significant increase in self-care and quality of life. The findings of the present study are consistent with those of the studies of Blackledge and Hayes (30), Yao et al. (31), and Izgu et al. (32).
When a patient faces negative emotions, the metabolic system becomes out of balance, which in turn disrupts blood sugar regulation. During negative emotions, the secretion of adrenaline, light adrenaline, and other stress-related hormones increases from adrenal glands, and these hormones affect the liver by converting liver carbohydrate storage into glucose (sugar) to provide energy, leading to a rise in blood sugar level. Therefore, emotion regulation can lead to a decrease in blood sugar level (33, 34).
According to studies, incompatibility with the disease and the lack of self-care behaviors have been usually associated with an avoidance-emotion-regulation style and non-expression of unpleasant emotions. Based on available evidence, avoiding emotions are associated with inconsistent consequences, and accepting and expressing them can encourage appropriate self-care behaviors (35). Avoiding the disease and related emotions is very common in diabetics and can be a factor in not following self-care behaviors (36). Furthermore, it can lead to the patient’s failure in following health care behaviors and adhering to treatment. Thus, accepting and expressing unpleasant emotions to achieve therapeutic goals can be adaptive and lead to increased self-care activities (34). This finding is consistent with the results of Ramesh et al. (37), who argued that adaptive emotion regulation strategies had a positive relationship with self-care behaviors.
In terms of the effectiveness of the acceptance component in controlling diabetes’ indices, it can be claimed that increasing acceptance in people with diabetes makes them more concerned about themselves and their health, so they try to take their medicines and insulin on time, better follow the diet recommended, do more physical activities, and measure blood sugar daily, which together improve the body’s metabolism and positively affect blood sugar, self-care behaviors, and finally quality of life (38, 39). As a result, it can be stated that the findings of this study are consistent with the studies of Hadlandsmyth et al. (40) and Gregg et al. (41), who showed the effectiveness of acceptance and commitment therapies on the self-care of patients with type 2 diabetes. Furthermore, studies showed that mindful eating techniques, which were introduced to develop an individual’s understanding of the diet and nutrition and to increase patients’ mindful awareness with regard to eating, were effective in achieving favorable results (42).
Therefore, emotion regulation education, by reducing unpleasant emotions and subsequent behaviors such as self-blame, blaming others, mental rumination, and boosting pleasurable emotions and subsequent behaviors such as acceptance, re-planning, and positive re-evaluation, can change this interactive relationship for the benefit of the patient and in a positive direction, for example, to improve diabetes control indicators.
5.1. Conclusions
Patients with type 2 diabetes are prone to a variety of psychological disorders (43). Based on previous studies, recognizing emotions and accepting unpleasant emotions, as well as accepting the status of the disease, can increase psychological well-being and quality of life in patients with diabetes). Since the techniques and skills of emotion regulation target the problems related to emotion regulation, this strategy can improve self-care in these patients.