1. Background
Sleep disorders are considered a significant health issue in older adults. It has been revealed that the incidence of sleep problems increases with age (1-3). Poor sleep is reported in about half of the individuals in old age (4, 5). Getting older is accompanied by the onset of prolonged sleep, disturbances in sleep duration, early morning awakenings, daytime sleepiness, and daytime naps (6).
Type 2 diabetes mellitus (DM) is a prevalent chronic metabolic disorder in late adulthood. It is related to various mental disorders such as depression and multiple physical complications, including neuropathy, retinopathy, nephropathy, and cardiovascular diseases (7, 8). It is estimated that 50 - 70% of patients with DM also suffer from sleep problems, and the incidence of sleep disorders is much more common in diabetic patients than in the general population (9, 10).
There is a reciprocal correlation between DM and sleep disorders. Sleep disturbances in patients with DM can be caused by DM or due to the microvascular and macrovascular complications of the disease (9, 11, 12). Overweight and obesity, as well as their accompanying complications, such as respiratory disturbances, can negatively affect the sleep quality in patients with DM. Diabetic neuropathy, musculoskeletal pain, restless legs syndrome, and polyuria, especially at night, deteriorate the sleep of diabetic patients (13). Furthermore, changes in lifestyle behaviors, particularly dietary patterns and physical activity, cause a higher prevalence of obesity and metabolic syndrome in older adults (14, 15), and these problems can be associated with more inappropriate sleep behaviors and sleep disorders (9). Patients with comorbid DM and poor sleep quality might have worse treatment adherence, self-care activities, diabetes-related glycemic control parameters (9), and poorer quality of life (16, 17).
Comorbidity of depression and diabetes is one of the most important clinical challenges in patients with DM, which each can exacerbate the other. Although the psychological effects of DM can contribute to depressive symptoms in these patients, previous studies suggest that underlying biological and behavioral mechanisms, such as hypothalamic-pituitary-adrenal activity, inflammation, sleep disturbances, inactive lifestyle, and sociocultural risk factors, affect this correlation (18). The inevitable changes in the physical and mental conditions of the elderly can affect the management of both diabetes and depression. Decreased physical capacity, due to declined muscle mass, respiratory capacity, visual and auditory intensity, functional and cognitive abilities, and frailty syndrome, results in increased complexity of the correlation between DM and depression in late adulthood (19).
2. Objectives
Evidence regarding factors that contribute to sleep quality in old age is limited. Hence, this study was conducted to identify the effect of DM on the association between depression and sleep disorders among the elderly in the north of Iran.
3. Methods
This case-control study is a part of the second phase of the Amirkola Health and Ageing Cohort Project (AHAP) (20). All people aged 60 years and more living in Amirkola, north of Iran, were invited to participate in the research. All elderly who completed the physical and laboratory exams related to the AHAP project were recruited following a census approach. Patients with bipolar disorders, psychotic symptoms, mental retardation, dementia, and other severe physical or mental disorders that could prevent participants from observing the study protocol were excluded. The sample size was estimated as 167 subjects per group, based on a 95% confidence interval, 80% statistical test power, and a prevalence of 35% for sleep disorders in the control group and 50% in the case group (9). To ensure the adequacy of the sample size and considering the possible drop out of the patients, the final sample size for each group was determined to be 400 persons, yielding a total of 800 subjects. Participants were divided into two equal groups randomly, based on DM's status. The case group (those suffering from DM) contained 400 subjects, including 200 subjects (100 males and 100 females) without depression and 200 subjects (66 males and 134 females) with depression. The control group (those without DM) contained 400 older adults (200 males and 200 females), of whom 200 had depression and 200 didn’t have. DM was defined as two fasting plasma glucose levels ≥ 126 mg/dL or receiving antidiabetic medications based on medical prescription (21). Noteworthy, fasting was defined as no caloric intake for at least eight hours (21).
Depressive symptoms were assessed using the Persian version of the Geriatric Depression Scale (GDS)-short form. This 15-item scale is developed to evaluate the state of depression in the elderly. Older adults with a score of 0 - 4 were classified as normal, 5 - 8 as mild depression, 9 - 11 as moderate depression, and 12 - 15 as severe depression (22, 23). The validity and reliability of the Persian version of this questionnaire have been confirmed in previous studies (24).
Sleep quality was assessed using the Pittsburgh sleep quality index (PSQI). The PSQI Questionnaire is a 19-item self-rating scale that measures the subjective quality of sleep over the past month. It has seven components: (1) sleep quality; (2) sleep latency; (3) sleep duration; (4) habitual sleep efficiency; (5) sleep disturbance; (6) use of sleeping medications; and (7) daytime dysfunction. The higher the score, the more severe sleep problems (1, 25). An overall score of 5 or higher indicates poor sleep quality (26). The Persian version of this scale has been examined in samples of Iranian adults, and its validity (≥ 0.90) and reliability (0.65) are confirmed (27).
The patients' age, gender, marital status, level of education, satisfaction with monthly household income, history of medications that might affect the sleep, such as benzodiazepines, antihistamines, stimulants (eg, methylphenidate), antidepressant, and antipsychotic medications, and, also, antidiabetic agents, including metformin and glibenclamide, were assessed through face-to-face interviews with the elderly or their proxies. The satisfaction of the person with the monthly household income was ranked into three categories as low, medium, and high, based on the patient's self-report.
Data analysis was administered using SPSS-18 by chi-square, ANOVA, Tukey post hoc test, and logistic regression analysis. Statistical significance was considered when the P-value < 0.05.
All participants were informed about the study protocol using a written informed consent form. Participants were informed that they could withdraw from the study at any time and their withdrawal would not deprive them of related educational and medical services. The research purpose and methodology were subjected to scrutiny by the Ethics Committee of Babol University of Medical Sciences (reference ID: IR.MUBABOL.HRI.REC.1397.030).
4. Results
Totally, 800 older adults were examined in this research, of whom 502 (62.8%) were illiterate, 262 (32.8%) had an educational level up to a high school diploma, and 36 (4.5%) had a university degree. Also, 641 (80.1%) were married and 159 (19.9%) were not married. Most of the participants (n = 553, 69.1%) reported a low satisfaction level with monthly household income, 235 individuals (29.4%) had medium satisfaction, and 12 (1.5%) had high satisfaction.
The categorization of participants, separated by the study group, based on depressive symptoms and distribution of PSQI scores in the four mentioned groups is provided in Table 1. The results showed that in both case and control groups, people with depression had lower sleep quality (P < 0.001). The mean age was 68.27 ± 5.85; 69.97 ± 6.76; 73.27 ± 8.59, and 72.26 ± 9.14 years in older people with diabetes ± depressive symptoms (DM+Dep±) and without diabetes ± depressive symptoms (DM-Dep±), respectively.
| Groups | PSQI Score | Total | |
|---|---|---|---|
| ≤ 5 | > 5 | ||
| With diabetes mellitus | |||
| With depression | 88 (21.7) | 112 (28.4) | 200 (25.0) |
| Without depression | 118 (29.1) | 82 (20.8) | 200 (25.0) |
| Without diabetes mellitus | |||
| With depression | 78 (19.2) | 122 (31.0) | 200 (25.0) |
| Without depression | 122 (30.0) | 78 (19.8) | 200 (25.0) |
Sleep Quality in the Case and Control Groups Based on Depression a
Mean PSQI scores in these four groups are presented in Table 2. There was a significant difference between the four groups concerning the PSQI score (P < 0.001). Tukey post hoc test revealed a significant difference in PSQI score between (DM+Dep+) and (DM-Dep+) patients with other groups (P < 0.05).
| Groups | PSQI Score | P-Value (ANOVA) | ||
|---|---|---|---|---|
| Mean ± SD | 95% Confidence Interval for Mean | Range | ||
| With diabetes mellitus | < 0.001 | |||
| With depression (n = 200) | 6.61 ± 3.43 B | 6.13 - 7.9 | 1 - 16 | |
| Without depression (n = 200) | 5.51 ± 3.14 A | 5.07 - 5.94 | 1 - 16 | |
| Without diabetes mellitus | ||||
| With depression (n = 200) | 6.75 ± 3.52 B | 6.26 - 7.24 | 1 - 16 | |
| Without depression (n = 200) | 4.98 ± 3.06 A | 4.55 - 5.41 | 1 - 15 | |
| Total (n = 800) | 5.96 ± 3.37 | 5.73 - 6.20 | 1 - 16 | |
Distribution of Age and PSQI Score in Older Adults with and Without Diabetes Mellitus and Depression a
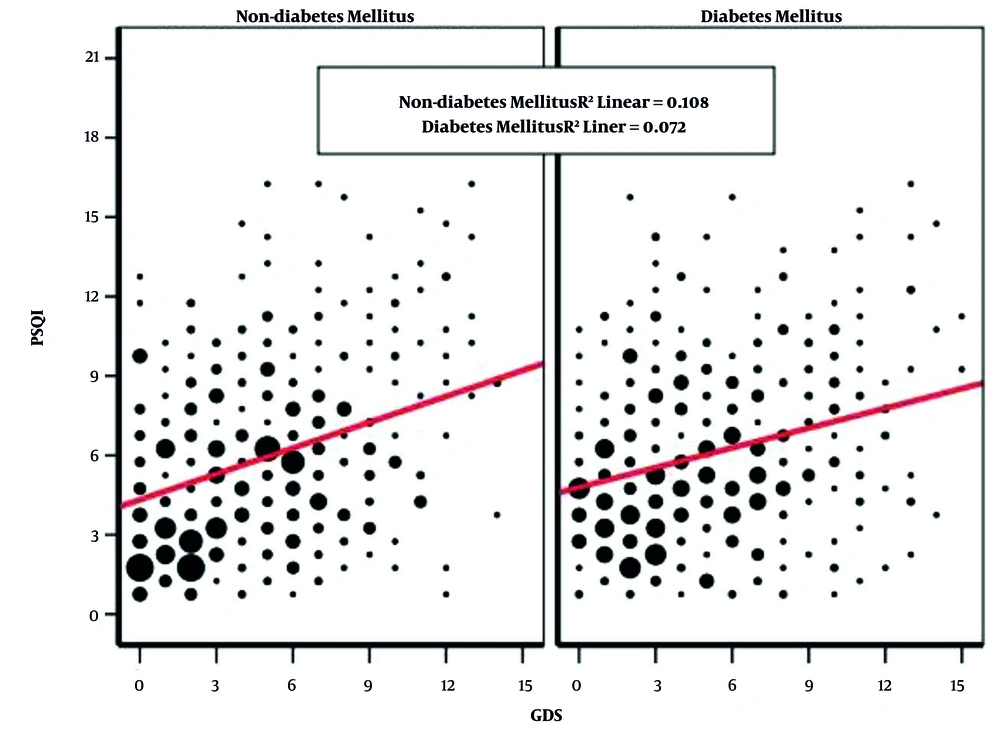
The correlation between PSQI and GDS scores in patients with and without diabetes is provided in Figure 1.
The results of the logistic regression analysis are presented in Table 3. This table shows the significant effect of female gender (OR = 2.36; 95% CI: 1.70 - 3.27) and depression (OR = 1.85; 95% CI: 1.37 - 2.51) on sleep quality of older adults (P < 0.001). Other characteristics, including age (P = 0.061), not to be married (P = 0.994), to have an academic level of education (P = 0.676), high satisfaction with monthly income (0.320), and diabetes mellitus (P = 0.170) had no significant effect on sleep quality of older adults.
| Characteristics | Crude Odds Ratio (95% CI) | P-Value | Adjusted Odds Ratio (95% CI) | P-Value |
|---|---|---|---|---|
| Age | 1.01 (0.99 - 1.03) | 0.202 | 1.02 (0.99 - 1.04) | 0.061 |
| Female gender | 2.33 (1.75 - 3.09) | < 0.001 | 2.36 (1.70 - 3.27) | < 0.001 |
| Not to be married | 0.71 (0.50 - 1.01) | 0.063 | 0.99 (0.66 - 1.48) | 0.994 |
| To have academic educational level | 1.57 (0.76 - 3.22) | 0.224 | 1.18 (0.55 - 2.54) | 0.676 |
| High satisfaction with monthly household income | 2.21 (0.66 - 7.41) | 0.201 | 1.90 (0.54 - 6.72) | 0.320 |
| Diabetes mellitus | 0.94 (0.71 - 1.24) | 0.724 | 0.71 (0.43 - 1.16) | 0.170 |
| Depression | 2.11 (1.59 - 2.80) | < 0.001 | 1.85 (1.37 - 2.51) | < 0.001 |
The Effect of Sociodemographic Characteristics, Diabetes Mellitus and Depression on Sleep Quality of Older Adults
5. Discussion
This study revealed the significant effect of depression on the sleep quality of older adults, regardless of the diabetes diagnosis. Our findings regarding the direct interaction of depressive symptoms with sleep quality are similar to another research conducted on 360 Iranian elderly that reported direct effect of depression on sleep quality of older adults (28). Also, a large population-based study on 8,888 adults in rural regions of China represented a similar direct interaction of depressive symptoms with sleep quality (29). A previous meta-analysis reported a significant correlation between older adults' poor sleep quality and depressive symptoms (30). Sleep disturbances and depression have a bidirectional association. It has been estimated that more than 90% of patients with depression might have a sleep disorder; conversely, sleep disorders can also cause depression (31).
In our research, older people with or without diabetes were more likely to present poor sleep if they had depressive symptoms, and diabetes mellitus did not show a direct significant statistical effect on sleep quality. In a study on 944 DM patients, Zhang et al. recommended pathophysiologic and behavioral mechanisms for the interaction of sleep quality, depressive symptoms, and glucose control in these patients. Poor sleep quality and depression are associated with dysregulation of the fronto-limbic system and reduced hippocampal volume, which might lead to dysregulation of the hypothalamic-pituitary-adrenal axis and the autonomic nervous system. This problem can increase the secretion of glucocorticoids, alter glucose transport, and activate immunoinflammatory modulators. Subsequently, an increased level of blood glucose might be observed. In addition, patients with depression and poor sleep quality might have insufficient diabetes self-care, poor diet, and persistent poor glycemic control (31). This issue can justify the greater effect of depressive symptoms on the sleep quality of participants rather than diabetes itself.
In this research, older women had lower sleep quality than men, especially if they had depressive symptoms, and the female gender showed a significant direct impact on sleep quality. Similar results are reported in a study conducted in China (32). Scientific evidence suggests that women are more likely to report aging-related sleep complaints. Besides, it is estimated that older women tend to experience more persistent depressive symptoms over time (32, 33). As women have a longer life expectancy than men, they are expected to experience more age-related problems, such as depression, sleep disorders, and diabetes. In addition, the complex interaction cycle among women can compromise the complications of each disorder.
With logistic regression analysis, when all the examined factors were simultaneously entered in the final model, age did not show a significant statistical effect on sleep quality of older adults. Although it is expected for older people to experience different changes in the quality and duration of sleep because of changes in the brain, sleep-related neurotransmitters, the body’s internal clock, and changes in production of hormones, such as melatonin and glucocorticoides, it seems that other variables such as gender, and depressive symptoms had higher effect than age on quality of sleep (34). In addition, the relationship between physical health, lifestyle behaviors and medication and sleep might have changed the association of age with sleep quality of the study population (32).
No significant association was found between marital status and sleep quality. Contrary to our results, a population-based study among individuals aged 65 years and over living in China reported that divorce, widowhood, and living alone affect the sleep quality of older adults (32). Another research in China revealed no significant association between marriage/cohabiting and the sleep quality of the elderly (34). Such differences can be attributed to the characteristics of study populations.
Higher satisfaction with monthly household income did not increase the risk of poor sleep quality. Contrary to this finding, a study on adult people of Southwest Ethiopia noted monthly income as a risk factor for poor sleep quality (35). Also, a study in the rural population of China showed a significant association between annual family income and sleep quality (29). Another study on adults over 50 years in Korea represented household income as an effective factor in life satisfaction and subjective well-being in late adulthood (36). The significant effect of depression on the sleep quality of the study participants can justify the non-significant association between satisfaction with monthly income and sleep quality.
The results showed that the PSQI score of 49.2% of people with DM was in the range of poor sleep quality, and the mean PSQI score was 6.61 and 5.51 in diabetic patients with and without depression, respectively. A previous study conducted on adult patients (with an age range of 30 and 80 years) with DM in Myanmar reported that 48.4% of participants had a PSQI score of > 5, and the mean PSQI score was 5.97 (10). Differences in results can be attributed to the baseline sociodemographic characteristics of the study populations and other variables that have been considered in the research protocol in addition to sleep quality; for example, comorbid physical and/or mental disorders, medications, and sleep-related environment and behaviors.
Zhao et al. reported an additive, rather than a multiplicative, interaction of poor sleep quality and depression in affecting the DM patients' quality of life; due to co-exist of both factors, the interactive effects of the two factors was greater than the sum of the two factors (37). Brandolim Becker et al. demonstrated that adequate sleep duration in old age (six to nine hours per day) facilitated better cognitive functioning, lower rates of mental and physical illnesses, and enhanced quality of life. Furthermore, sleep quality was reported as an intervening variable between depression and quality of life (38). This should trigger healthcare providers to pay more attention to early identification and proper management of both depression and sleep disorders in diabetic patients.
The individuals who participated in this research were community-dwelling older adults, and we examined DM, depression, and sleep quality, simultaneously. These can be considered as the main strength of this study. However, not considering confounding variables, such as blood glucose control indices and the effect of the medications taken by the patient, can be mentioned as the limitations of this study. For future studies, a structured interview to explore depressive disorders, assessment of individuals' sleep behaviors, and matching different factors that might affect the sleep quality of older adults, such as smoking, alcohol, and caffeine consumption, are recommended.
5.1. Conclusions
Our findings represented that older people with or without DM are more likely to present poor sleep if they suffer from depressive symptoms. In addition, DM did not show a significant direct effect on sleep quality.