1. Background
Physical and mental health are two inseparable dimensions of general health that affect each other (1). A comprehensive understanding of mental and physical health is pivotal to comprehending the concept of health in humans (2). Therefore, considering the interaction between body and mind and the need for integrated health in both to achieve general health, recognizing the permanent interaction between these two seems essential (1, 2). Due to the role of general health in the quality of life and life expectancy, further attention needs to be paid to the concepts of health and well-being in society (3).
Despite the influential role of self-perception of fitness (SPF) in health and well-being, limited studies have been conducted on the subject (4). Self-perception of fitness means the individual's views and attitudes toward physical fitness (5). An incorrect SPF may lead to behavioral and lifestyle alterations that consequently modifies the general health (5, 6). Also, in societies where having an ideal body and high physical fitness is a value for social acceptance, a correct SPF is particularly important (7, 8). The results of studies have shown that most people have incorrect SPF, which would lead to physical and psychological problems such as depression, anxiety, aggression, and drug abuse (9, 10). Physical fitness, an important segment of health and well-being, is defined as the intrinsic and acquired characteristics and abilities associated with performing physical activities (11, 12). Self-perception of fitness is a multidimensional phenomenon divided into physical, emotional, cognitive, and social components (5, 12). Based on the results of studies, physical fitness modifies self-estimation due to its effect on the feeling of strength and competency (10, 13).
Coronavirus disease 2019 (COVID-19) has become a pandemic following the identification of the first case in December 2019, leading to global preventive measures (14), which are accompanied by changes in behavioral patterns and cessation of daily physical activity habits (15). Although these measures are vital to reduce the prevalence of COVID-19, short-term and long-term consequences in physical and mental health are expected (16). These situations may be associated with the disruption of life routines such as reduced physical activity and fitness and increased stress and anxiety (16), which may lead to incorrect self-estimation of the physical fitness level and attenuation of the immune system (17). According to studies, adequate physical activity level (PAL) during the COVID-19 outbreak, on the one hand, reduces the risk of non-communicable diseases and viral/bacterial infections (18, 19) and, on the other hand, leads to a more accurate SPF (20). Unfortunately, reduced PAL induced by COVID-19 may affect physical fitness, quality of life, and general health, leading to false SPF (21, 22).
2. Objectives
Although the positive effects of physical activity on the immune system and a right SPF on general health and well-being have been studied in detail, to date, no studies have examined the PAL among COVID-19-recovered individuals (CRI). Therefore, this study aimed to investigate the relationship between PAL and SPF in CRI (men and women).
3. Methods
3.1. Participants and Study Design
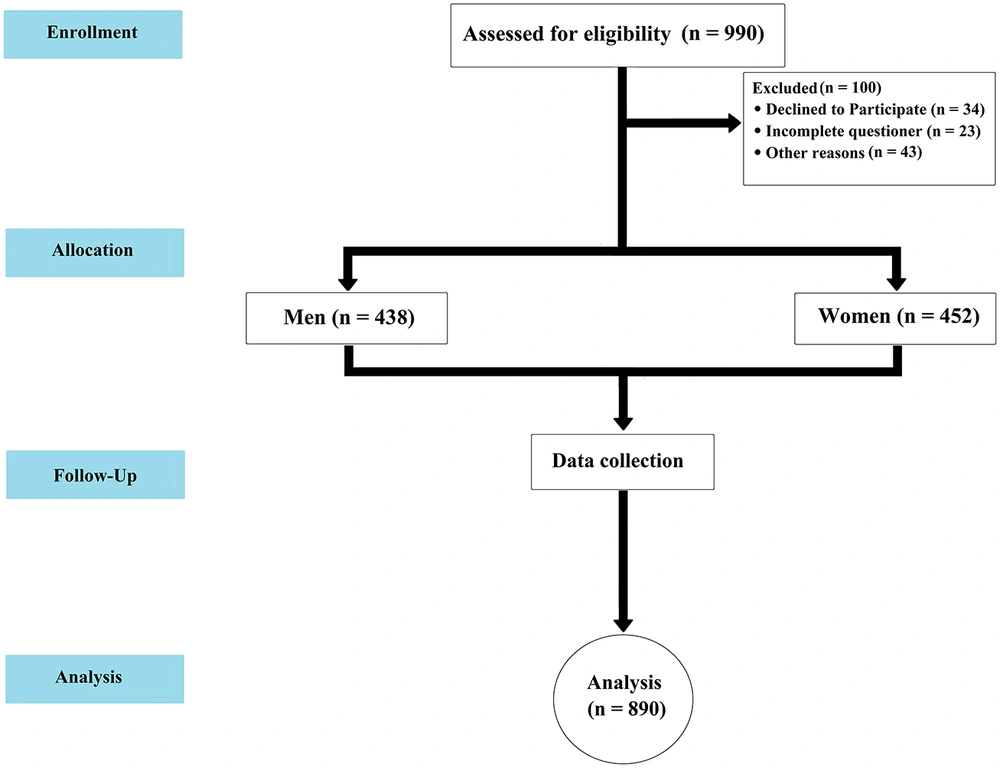
According to the latest statistics of Kermanshah University of Medical Sciences, until early February 2021, a total of 7,000 COVID-19 cases were tested positive at the COVID-19 testing centers. Then, according to Morgan's sample size table, a total of 990 CRI (men and women) living in Kermanshah city were randomly selected. A multistage cluster sampling method was used to select participants. Kermanshah city was divided into five regions: North, south, east, west, and center. The sample size was estimated at 168 CRI from each testing center in each region (a total of 840 individuals). A plus of 30 CRI was considered for each region to prevent the possible loss of sample; thus, a total of 990 CRI (198 from each region) were randomly selected for the study. The selection method was based on the blocks of each area, and the individuals were studied based on the random division of the blocks. After the final investigation, 100 subjects were excluded from the study due to incomplete answers to the questions, and thus, 890 subjects (438 men and 452 women) were analyzed (Figure 1).
Inclusion criteria included an age of 20 - 70 years, a positive COVID-19 test, finishing the recovery period of COVID-19 (21 days after the COVID-19 test), and complete improvement (having no sign or symptoms) based on the self-report. The subjects were informed of the study, confidentiality of information, and the purpose of the study. This study was approved by the Ethics Committee of Razi University of Kermanshah (IR.RAZI.REC.1399.064).
3.2. Tools
The data collection tool consisted of three self-report sections.
3.2.1. Demographic Information
The first section consisted of four questions about demographic information, including age, sex, height, and weight.
3.2.2. Physical Activity Level
The PAL was assessed using the short form of the International Physical Activity Questionnaire (IPAQ-SF) (23). This questionnaire consisted of seven questions organized into four sections: Intense PA, moderate PA, walking, and sitting (24). The intensity and duration of PA were questioned for a week, and activities lasting more than 10 minutes were recorded (23, 24). Intense PA included heavyweight training, prolonged aerobic exercise, intense cycling, and running. Moderate PA included lightweight training, regular steady-state cycling, and tennis. Walking activities included walking at home and work, leisure time walking, and planned walking. Sitting included the amount of time spent sitting at home, work, leisure, reading, watching TV, and meeting friends (25, 26). The validity and reliability of the questionnaire have been confirmed for the Iranian population (27). Based on the scoring method of the IPAQ, the individual's PAL during the past week was calculated in terms of MET minutes/week. Walking intensity gained 3.3 METs, moderate PA gained 4 METs, and intense PA gained 8 METs. Then, walking, moderate PA, and intense PA were measured in MET minutes/day during the past week to calculate the total amount of PAL (28). The PAL scores below 600 were categorized as low, 600-3,000 as moderate, and above 3,000 as high.
3.2.3. Self-perception of Fitness
A translation of SPF questionnaire by Delignières et al. (1994) was used to assess SPF (29). The validity and reliability of the questionnaire have been confirmed for the Iranian population by Hosseini et al. (2012) (10). This questionnaire includes one to 13 scored answers about SPF factors, including fitness, strength, cardiorespiratory endurance, flexibility, and body composition. A score of 1 indicates the lack of perception of the attribute, a score of 7 indicates a normal perception of the attribute, and a score of 13 indicates a high perception of the attribute. The fitness factor represented a general perception without additional explanation, whereas the other four factors were qualified with a short description. The SPF was calculated by summing up the scores of SPF factors (fitness, strength, cardiorespiratory endurance, flexibility, and body composition) divided by five to obtain the mean score. The SPF scores < 7 were categorized as low, 7 - 10 as moderate, and > 10 as high.
3.3. Statistical Analysis
After confirming the normality of data distribution by the Kolmogorov-Smirnov test, the independent t-test was used to compare the mean of variables between men and women, and the Pearson correlation coefficient test was used to evaluate the relationship between variables using SPSS version 24 software at a significance level of P < 0.05.
4. Results
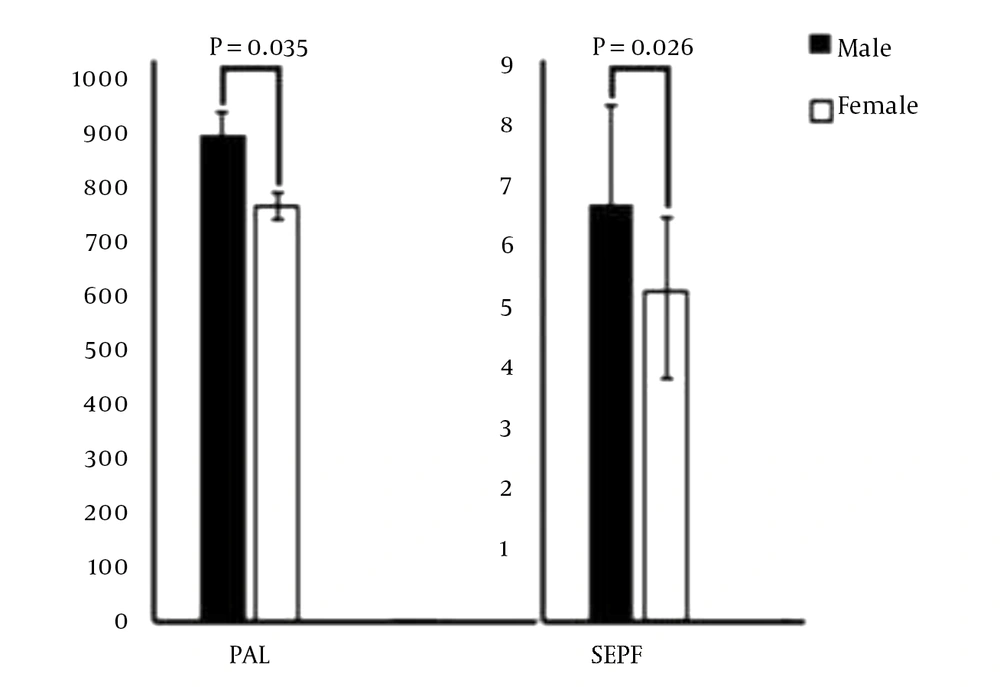
This study enrolled 890 CRI (438 men and 452 women). The mean and standard deviation of age, height, weight, body mass index, PAL, and SPF are presented in Table 1.
| Variables | Men (n = 438) | Women (n = 452) |
|---|---|---|
| Age (y) | 43.10 ± 12.11 | 41.20 ± 9.08 |
| Height (cm) | 177.02 ± 8.06 | 167.01 ± 6.04 |
| Weight (kg) | 83.01 ± 12.02 | 78.04 ± 11.03 |
| BMI (kg/m2) | 26.49 ± 3.03 | 27.96 ± 4.09 |
| PAL (MET) | 876.11 ± 40.23 | 739.08 ± 27.02 |
| SPF | 6.64 ± 1.62 | 5.27 ± 1.39 |
The present study results showed a significant positive relationship between high and moderate PAL and SPF in CRI (both men and women). In contrast, there was a significant inverse relationship between low PAL and SPF in CRI (both men and women) (Table 2).
aSignificant relationship of PAL with SPF; the value is calculated using the Pearson’s Correlation Coefficient test.
The results of the independent t-test showed a significant difference in PAL and SPF between men and women. Men had significantly higher PAL (P = 0.035) and more accurate SPF (P = 0.026) than women (Figure 2).
5. Discussion
This study aimed to investigate the relationship between PAL and SPF among CRI (men and women). The present study results showed that CRI (both men and women) had insufficient PAL and incorrect SPF. Also, the present study results showed that subjects with moderate and high PAL were able to accurately estimate their physical fitness, while men and women with low PAL were not able to estimate their physical fitness accurately. However, our knowledge of the effect of sufficient PAL on the correct SPF in CRI is limited. In line with the present study, the results of previous studies on healthy individuals showed that PAL would affect the accuracy of SPF (5, 30). For example, Rentzsch et al. (2016) and Jensen et al. (2018) indicated a positive relationship between the SPF and PAL (31, 32).
Also, the present study results showed that men had higher PAL than women, which is probably one of the reasons for more desired SPF in men than in women. The results showed a significant positive relationship between high and moderate PAL and SPF in CRI (both men and women). Consistent with these results, there is strong evidence supporting that 2 - 2.5 h of exercise per week is sufficient to reduce the risk of chronic diseases (33, 34). Numerous epidemiological studies have shown that exercise improves SPF and creates a sense of wellbeing (34, 35). According to previous studies, regular exercise could help maintain self-confidence, control anxiety and depression, and correct SPF (27, 36). Moderate PAL causes a correct perception of physical fitness, possibly by inducing physiological changes and reducing stress due to the quarantine and preventive measures during COVID-19.
Also, previous studies have shown that participating in exercise, and physical activity regardless of type (aerobic, resistance, and combined) leads to an accurate SPF (4, 33). In general, via generating correct feedback, a correct SPF might lead to an adequate PAL. For example, the studies of Marsh and Redmayne (1993) (34) and Monroe et al. (2010) (35) showed a significant direct relationship between the overall PAL score and the overall SPF score (4, 11). Sonstroem also states that participating in physical activities by increasing physical abilities and physical fitness can affect the individual's perception of physical abilities and competencies, increasing self-satisfaction, health-promoting behaviors (improved healthy behaviors such as sleep and nutrition) (36), and the tendency to participate in physical activities (5, 37). However, the outbreak of COVID-19 and the fear of becoming ill have led to increased stress and anxiety, reduced mental health, and misestimating physical fitness in CRI.
5.1. Limitations
One of the limitations of this study was the low motivation of officials and subjects to participate in the research. In addition, according to the principle of individual differences, the psychological characteristics of individuals might have affected the research results. Therefore, more precise control of these factors is recommended in future research.
5.2. Conclusions
Based on the present study results, the wrong SPF in CRI with low PAL might be one of the reasons for being insufficiently active. Based on the importance of adequate PAL, a proper understanding of PAL could be considered the first step of a regular physical activity schedule to enhance the correct SPF.