1. Context
In December 2019, several pneumonia cases of unknown origin were identified in Wuhan, China, and this highly contagious disease quickly became a pandemic (1-4). The World Health Organization (WHO) and other public health officials have taken steps to prevent the spread of COVID-19, but the disease has caused a great deal of stress throughout the world (5). The COVID-19 outbreak has caused many problems worldwide, including mental health problems in most people. Many people and health care providers have experienced psychological problems such as anxiety, depression, stress, alcoholism, and other disorders (6, 7). At first, the outbreak caused mental health problems in public in China and medical workers in Wuhan (8). Countries such as China, Singapore, and Australia emphasized the psychological effects of COVID-19, acknowledging that the fear of COVID-19 could harm society more than the disease itself (9). For this reason, the demand for remote psychologist services increased (10).
In addition to the newly emerged mental patients, previous patients receiving psychological services before the outbreak also need to receive such services in new ways in this period (11). Also, during the outbreak, providing face-to-face psychotherapy services increases the risk of disease transmission (12). Therefore, health services should be provided with approaches that minimize the need for face-to-face visits and physical presence. This issue led to the increased use of digital health alternatives such as smartphone apps and other online assistance tools (13).
In the medical field, new technologies can help treat and control diseases (14). Experiences of health care providers during the COVID-19 crisis prove that disease management is not feasible by relying on traditional methods, and new approaches are required for optimal management (15). Therefore, it is imperative to benefit from health information technologies to improve the quality of care and reduce costs, especially during the COVID-19 outbreak (16, 17). Digital technologies can be used to reduce face-to-face visits and the observance of social distance (18, 19). The experiences with similar diseases, such as MERS and SARS, confirm these benefits (20).
Telemedicine is the most successful technique to manage and handle COVID-19 emergency cases (21). Research shows that telephone support and telecommunication programs in this situation seem promising for patients with mental disorders (22). Remote, online, and virtual health counseling services exemplify the use of telemedicine to solve mental problems (7, 9, 23). In general, telemental health can be defined as the use of information and communication technology, like videoconferencing, to deliver mental health care remotely, including evaluation, medication management, and psychotherapy (24).
Psychiatric services should not be disrupted due to the COVID-19 quarantine, limitation, and lockdown. Telemental health reduces the risk of infection for health care providers and helps continue treatment. This technology is also beneficial when there is a shortage of specialists or long distances (24, 25). There is a need for new approaches for effective remote care with physician-patient solid interaction. In this regard, a review study can provide complete and clear insights into the role of telepsychiatry in providing psychiatric services. This study tried to provide complete and precise insights into the critical perspectives of selected articles and different aspects of previous research in this area. The purpose of this study was to review the role of information technology, especially telemental health, in the management of psychological problems during the COVID-19 pandemic.
2. Evidence Acquisition
2.1. Study Design
This rapid review used the preferred reporting items for review methodology according to the principles of PRISMA proposed by Moher et al. (26). It provides an effective method for creating a significant synthesis of current evidence.
2.2. Research Questions
The present review responds to the following research questions:
RQ 1: Which countries have designed the telepsychology approaches during the COVID-19 pandemic?
RQ 2: What techniques have been used to develop this technology?
RQ 3: What are the primary purposes of using telepsychology during the COVID-19 pandemic?
RQ 4: What methods have been used for developing telepsychology?
RQ 5: What results have been achieved after applying this technology?
2.3. Data Sources
In the first phase, a search was conducted in titles and abstracts of related studies published in major online medical databases, including PubMed, EMBASE, Scopus, Web of Science, and ScienceDirect. The initial search showed a wide range of available evidence on the role of health information technology in the psychological problems during the COVID-19 outbreak. In addition to keywords, Medical Subject Headings (MeSH) were used to select the correct search terms. Those containing COVID-19, coronavirus, novel coronavirus, 2019-nCoV coronavirus, SARS-CoV-2, SARS2, physiological disorders Tele *, and Boolean operators (AND, OR, and NOT) were used to combine the terms. Shortly before writing the present article, an additional search was done to update the previous results.
2.4. Search Strategy
The search was conducted between June and July. The time limitation for article searching was 2019 onward. We used two search strategies to come to better conclusions and gain correct results. For example, the first search strategy in the PubMed database was executed as follows:
(COVID-19 [title/abstract] OR COVID-19 [title/abstract] OR Coronavirus[title/abstract] OR Novel coronavirus[title/abstract] OR 2019-nCoV[title/abstract] OR SARS-CoV- 2[title/abstract] OR SARS2 [title/abstract]) AND (Telemedicine[title/abstract] OR Tele-medicine[title/abstract] OR Telehealth[title/abstract] OR Tele-health[title/abstract] OR Telecare[title/abstract] OR Mobile health[title/abstract] OR mHealth[title/abstract] OR Electronic health[title/abstract] OR eHealth[title/abstract]) OR Information Technology[title/abstract]) AND (Psychiatric Disease[title/abstract] OR Behavioral disorder[title/abstract] OR Mental Disorder[title/abstract] OR Psychiatric Illness[title/abstract] OR Psychiatric Diagnosis[title/abstract], OR Psychotherapy [title/abstract]).
The second search strategy in the PubMed database was executed as follows:
(COVID-19[title/abstract] OR COVID-19[title/abstract] OR Coronavirus[title/abstract] OR Novel coronavirus[title/abstract] OR 2019-nCoV[title/abstract] OR SARS-CoV- 2[title/abstract] OR SARS2[title/abstract]) AND (Telemental[title/abstract] OR Telebehavioral[title/abstract] OR Telepsychology[title/abstract] OR Telepsychiatric[title/abstract] OR Telepsychiatry[title/abstract] OR Telepsychotherapy[title/abstract])
In addition to completing the search and finding the papers and reports not found in the initial search, resources related to selected articles were reviewed. Furthermore, Google databases, Google Scholar, and significant health websites were examined carefully and manually. These websites were the World Health Organization (WHO, https://www.who.int), Centers for Disease Control and Prevention (https://www.cdc.gov), and National Institutes of Health and Clinical Excellence (https://www.nice.org.uk).
2.5. Inclusion Criteria
The criterion for the inclusion of articles in the present study included studies explicitly examining health information technology tools practically and interventionally to prevent, diagnose, treat, control, and manage mental disorders caused by the COVID-19 outbreak. This study also included patients receiving psychiatric services before COVID-19, as these patients also need to continue such services through information technology tools. All the selected documents were written in English and published in peer-reviewed journals. All the studies applying any information technology tools as an intervention in each aspect of health care (such as diagnosis, treatment, training, and counseling services for patients with mental disorders) were included in this study.
2.6. Exclusion Criteria
Studies with incomplete information, unavailable full texts, not well-defined performance methods, one-page studies, review studies, letters, editorials, commentaries, short communications, correspondences, opinion papers, and articles not reporting original data were excluded.
2.7. Study Selection and Data Extraction
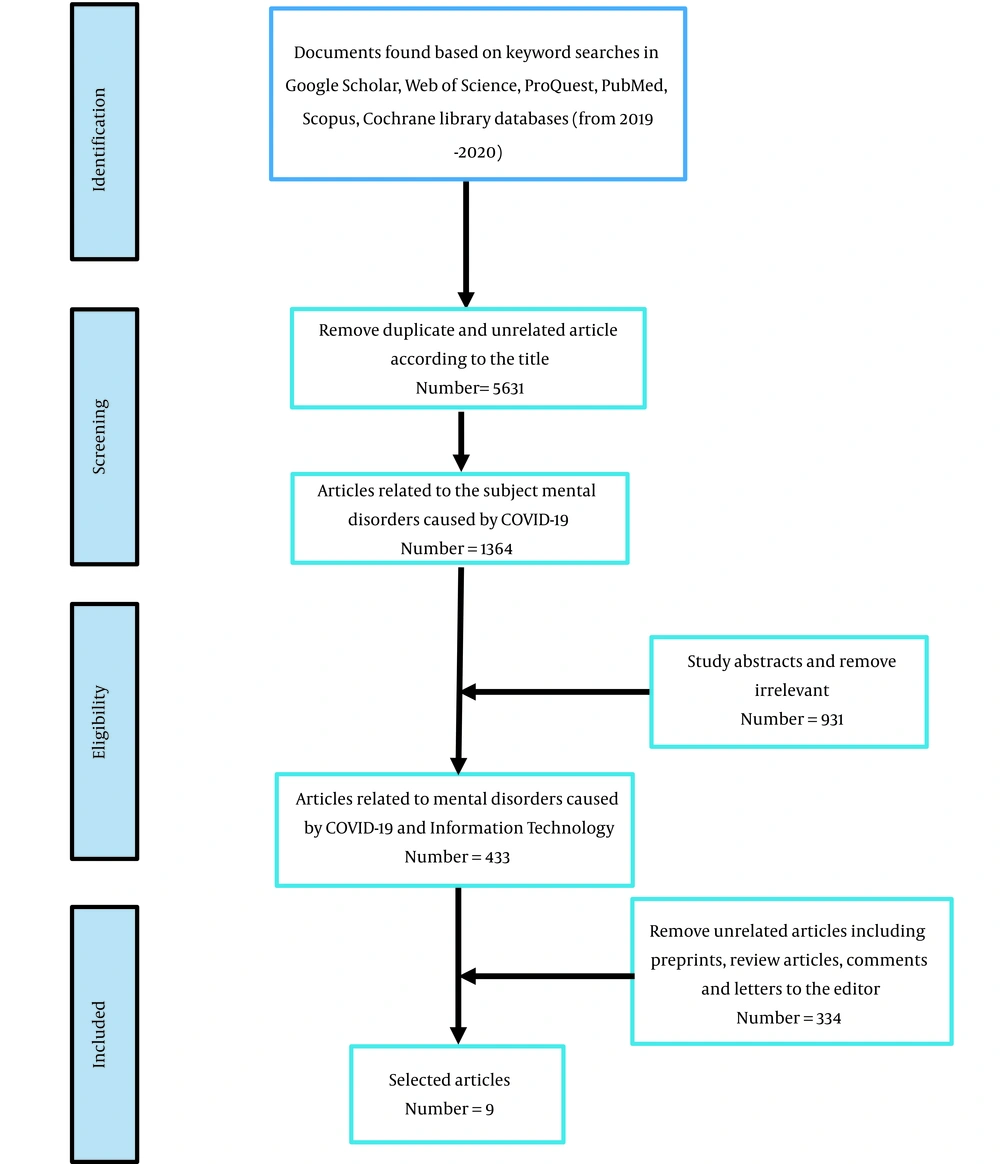
In the first step of the search, the results were entered in Excel software, and all duplicate articles were removed. Then, all the three authors separately screened the studies in the first stage based on inclusion and exclusion criteria in the title and abstract. Afterward, to ensure the correctness of the included documents and complete the items of the data extraction form, we carefully examined the full texts of the selected studies. The required data were extracted from all selected articles with eligibility criteria at this stage. Extracted data included the first author's name, care setting, purpose, applicable technology, method, intervention, and results. Finally, nine articles were selected for data extraction. A summary of the search strategy is provided in Figure 1.
During the numerous meetings held by the authors, the composition and expression of the study results were performed by the narrative synthesis method. This method had three stages, including developing a preliminary synthesis, exploring the relationships within and between studies, and determining the robustness of the synthesis. Lastly, the data of the selected studies were qualitatively described and presented. We extracted the following characteristics of studies during narrative synthesis:
- The purpose of the intervention, e.g., developing a telepsychotherapy program for patients, families, children, and service providers and implementing home-based telemental services during the COVID-19 pandemic
- The type of intervention, e.g., videoconferencing, web-based educational modules, or mobile applications
- Study methods and intervention duration
- The result of the intervention, e.g., behavior improvement and mitigation of emotional side effects of COVID-19
3. Results
The details of the research are available in Figure 1. After removing duplicate items and screening titles and abstracts, full-text articles were studied. Finally, the necessary information was extracted from nine articles. The seven variables of the selected papers are presented in Table 1. The results showed that seven studies were conducted in the United States, and only one study was conducted in each of the countries Iran, France, and Spain.
| Author | Setting | Purpose | Technology | Method | Intervention | Result |
|---|---|---|---|---|---|---|
| James Riegler et al. (27) | University of Cincinnati- United States | Developing a telepsychotherapy; parenting skills program for military veterans | Online parenting pro-tips (OPPT) and combined web-based educational modules | Study type: cross-sectional; N= 22 veterans with a child between the ages of 3 and 9 years | Six-session intervention including; session 1: Introduction to online parenting pro-tips; session 2: Positive parenting; session 3: Lead your child; session 4: Behavior management; session 5: Time-out procedure; session 6: Positive parenting skills in daily life and house rules | Meaningful reductions in veteran depression, parenting stress, family dysfunctio, and improvements in child behavior |
| Ramtekkar et al. (28) | Nationwide Children’s Hospital- United States | Developing telebehavioral health (TBH) services | HIPAA-compliant version of the Zoom video platform | Video visits and consolation with the phone; The trend was increasing in video visits over time. | Over 50,000 TBH visits within six weeks | NA |
| Geoffroy et al. (29) | Paris- France | Developing psychological support system for all hospital workers in Paris during the COVID-19 outbreak | Psychological support system- telephone call | Study type: cross-sectional; Population: all hospital workers in 39 hospitals (1,300 doctors, 3,600 residents, and more than 52,000 nursing, paramedical, and socio-educational staff) | Six steps for developing the system were made in only three days; call numbers: In 26 days of hotline activity, they received 149 calls; call duration: Minimum 1 to maximum 15 calls per day with a mean of 5.73 calls/day | Primarily women (86%) called the hotline. The mean age of callers was 32.7 years. The average call duration was 18.5 min. Reasons for calling were anxiety symptoms (n = 73, 49%), requesting hotline information (n = 31, 20.8%), worries about COVID-19 (n = 23, 15.44%), exhaustion (n = 17, 11.41%), trauma reactivation (n = 10, 6.11%), insomnia (n = 9, 6.0%), anger (n = 8, 5.37%), depressive (n = 6, 4.02%) and psychotic symptoms (n = 3, 2.01%). |
| Lau et al. (30) | United States | Using NYC health + hospitals (NYC H+H) for television and conducting behavioral health encounters | NYC health + hospitals (NYC H + H) | Transforming the existing system using virtual care platforms to serve the new patient. One team focused on delivering mental health and addiction services. | The 30,000 behavioral health encounters via telephone and video in one month; novel virtual buprenorphine clinic for increasing access to medication-assisted treatment; the clinic was available through a phone hotline. | The mitigation in emotional side effects of COVID-19 |
| Sullivan et al. (31) | Cleveland Clinic | Providing mental health services through telehealth and virtual visits for frontline providers and clinical work with patients | Telepsychology | Running virtual counseling sessions and documentation of sessions; an additional smart phrase was added regarding the COVID-19 crisis and telemedicine to the documentation. | Developing a protocol for a virtual visit during COVID-19; Connect to the patient via facetime, Google Duo, Skype, and Telephone (only for follow-up visits) | NA |
| Zarghami et al. (32) | Fasa University Hospital (Iran) | Telepsychiatric Evaluation of SARS-CoV-2 Patients | Telepsychiatry | Interviews with patients by a psychiatrist through video chat; duration: one month (March–April 2020); N = 82 patients with COVID-19 (32 inpatients and 50 outpatients) | Completion of Patient Health Questionnaire-9 (PHQ-9), Generalized Anxiety Disorder Assessment (GAD-7), and Perceived Stress Scale-14 (PSS 14) for each patient; after the initial survey, supportive psychotherapy, pharmacotherapy, and follow-up visits were prescribed for the patients. | The disorders were: Insomnia in 24 patients, adjustment disorder in 13 patients, and mental disorders in 33 patients. Telepsychiatry is efficient in the early stages of mental problems during the COVID-19 pandemic to screen psychosomatic comorbidities. |
| Douglas et al. (33) | United States | Proposed strategies for integration of measurement-based care into telemental health services | Telemental Health Measurement-based Care (tMBC): Laptop with a 12-in. screen; a text-based notes application; Zoom videoconferencing software with an option for HIPAA-compliant telehealth and Mirah, an MBC platform | In running the system, the following were considered: 1- Introducing tMBC to clients 2- Sending links by text message (SMS) or e-mail for clients to complete measures 3- Setting up your screen(s) 4- Sharing feedback with clients 5- Billing and reimbursement for MBC | tMBC measures were: Brief symptom rating scales; individualized items; monitoring the risks; treatment process measures | NA |
| Goodman-Casanova et al. (34) | Spain | Providing television-based and telephone-based health social support to patients with mild cognitive impairment or mild dementia | TV-AssistDem (Television-based Assistive Integrated Service to support European adults living with mild dementia or mild cognitive impairment) | Clinical trial: 93 participants were divided into two intervention and control groups. The intervention group received more memory exercises with TV-AssistDem than the control group. The age of participants was > 60 years. | Health information and counseling about COVID-19 were presented by health professionals. | The physical and mental health and well-being improved in the intervention group. |
| Sharma et al. (35) | United States | Implementing a home-based TMH (HB-TMH) service during the COVID-19 pandemic | Home-based TMH (HB-TMH) service | Converting the outpatient clinic to a Virtual Telemental Health (TMH) clinic | The Department of Psychiatry and Behavioral Medicine provided at-home phone appointments by clinicians in clinics. The four components contributing to HB-TMH implementation included training, technology, administrative support, and patient needs and relevance for TMH. | After three and four weeks of implementation, 67% and 90% of all appointments were conducted at home, respectivel. By week six (April 3, 2020), reliable HB-TMH appointments were implemented. |
Extracted Variables from Included Studies in This Review
The results illustrated that Telehealth approaches are practical to increase participants' mental health and well-being with various mental problems. Telemental health and telepsychiatry have been implemented successfully in various mental health conditions and clinical settings.
This review showed that in some cases, existing infrastructure was upgraded and used to provide mental health services (30). New systems and protocols were developed to deliver these services in other cases. In Zarghami's study, telepsychiatry was used to assess the mental health of COVID-19 patients. The findings of this study confirmed the effectiveness of telepsychiatry in the early stages of mental problems in the psychological assessment of patients and stressed the importance of continued treatment (32).
Some studies provided telepsychiatry to people whose mental problems developed during COVID-19 (32). Another study showed the telepsychological service provided to patients with mental illness and problems before the epidemic (34). Most articles signified the influential role of telehealth in screening and reducing social contacts. Besides, this technology played a significant role in providing services related to mental health.
4. Discussion
This review surveyed the role of telemental services in the prevention, treatment, and control of mental and behavioral disorders during the COVID-19 outbreak. The results and implications of several telemental tools for the management of COVID-19 were described.
Since the outbreak of the COVID-19 epidemic, various solutions have been proposed to control it, but the best solution is to keep social distance (36). The COVID-19 pandemic has caused significant changes in information technology (IT). During this epidemic, the role of telemedicine in disease management became more prominent (37).
Telehealth manages a wide range of diseases during the COVID-19 epidemic. Studies indicated that technologies such as videoconferencing for clinical counseling have been highly satisfactory for providers and patients. While maintaining the quality of services, these technologies reduce the costs (38). Telemedicine has also been used to follow-up patients such as patients with diabetes, liver disease, and MS during COVID-19 (39, 40). This technology has been implemented to provide care for patients with liver disease who could not receive direct services in the COVID-19 era (41). Moreover, during this epidemic, telemedicine provides an excellent opportunity for providing care to patients with diabetes (42).
Along with the COVID-19 outbreak and the increasing number of deaths and physical problems in the patients, many people in the community, as well as health care providers, experienced psychological problems like anxiety, depression, and stress (7). The providers, physicians, and patients experience fear of disease or transmission to others, social isolation, negative news, feeling lonely, and uncertainty (43). These conditions harm their quality of life, social relationships, and job performance (44). The results of many studies have confirmed psychological problems in people and the need to provide psychotherapy services (45). Along with the outbreak of COVID-19 in China, one of the most critical issues was reducing psychological crises among medical workers, patients, and other affected people. One solution was creating an online platform for psychotherapy services (46). It seems that in the early stages of mental problems during COVID-19, telepsychiatry is efficient for providing psychotherapeutic interventions (32).
The National Health Commission of China has published multiple instructions, guidelines, and educational articles/videos by expert teams for delivering mental health services (16). During the COVID-19 epidemic, online psychological counseling services (e.g., WeChat-based resources) and psychological self-help intervention systems are widely implemented in China, which provides free 24-hour services seven days a week (7).
The effectiveness of telehealth has been proven in providing psychological services in disasters (47). Telehealth technologies are ideal for managing infectious diseases, maintaining social distance, reducing individual contact, and ultimately decreasing virus transmission (48). Telehealth allows remote care or evaluation (triage) for infected or suspected COVID-19 patients. With this technology, it is also possible to provide the necessary care for other patients with physical and mental problems (49).
4.1. Conclusions
COVID-19 has many psychological impacts on individuals. Therefore, there is a need to provide psychological services for the community. Such services can be provided through telemental health care by health professionals. Telepsychiatry has increased significantly during the COVID-19 epidemic. This study approves the usability of telepsychiatry in improving health care provider practices during the current pandemic.
There are some limitations to using this technology; for instance, some people do not access the Internet or smartphones. Some factors to be considered in implementing this technology are as follows:
- Allocating sufficient funds and resources to the implementation of telemental systems
-Preparing the necessary technical, human, and cultural infrastructure for system implementation
- Providing the necessary training to users at different levels
- Verifying the clinician readiness and competency for the use of the system
- Determining the reimbursement process in these systems and providing solutions or reimbursement challenges and restrictions
- Evaluating information quality continuously
- Respecting information confidentiality, patient privacy, and legal issues
- Observing social justice and providing public access to services