1. Background
Hospitalization in the neonatal intensive care unit (NICU) may continue for a few days to a few months, depending on the level of neonatal immaturity or medical condition (1). Since NICU admission is a stressful, difficult, and terrifying experience for both infants and parents (2), special attention has been paid to the mothers of NICU-admitted infants in recent years. Many studies have shown that parents of premature or low-birth-weight infants experience higher levels of depression and anxiety and that they are at a higher risk of communication problems, sleep disturbances, family tension, and economic problems (3). The traumatic effects of early childbirth impair mothers’ judgment and thinking abilities, thus augmenting tension and stress of having high-risk infants (4).
In addition to infant prematurity and low birth weight, the physical environment of the ward, noisy equipments, different chemical odors, monitoring devices, ward warning sounds, and ventilators can be intimidating to visitors. It can be also very disturbing for parents to see their infant connected to a hospital device and surrounded by the medical staff; in fact, loss of parental expectations is the greatest source of tension for parents (5). These tensions, if chronic, cause damage and affect mothers' quality of life, as depression may occur following mental trauma (6).
Maternal coping is defined as the mother's efforts to remove or minimize stress and increase her tolerance. Black, quoting Folkman and Lazarus, states that coping and stress are inseparably related (4). Mothers of premature infants often use different mechanisms to overcome their stress and cope with their unbalanced status. On the other hand, coping methods have a close association with social support and mental health of mothers of premature infants. The effective factors for the use of coping styles include social support, awareness about stressful factors, sleep patterns, and personal hygiene (5).
If the mother employs efficient coping styles, she can regulate her emotions, reduce the negative effects of stress and depression due to prematurity, and increase her compatibility and interactions with her infant (7). In this regard, Shaw et al. (2006) in a study on 124 parents of premature infants showed a significant relationship between efficient coping of parents in the NICU and the rate of social support and optimism (7). Use of inefficient styles increased the negative effects of stress and had adverse impacts on the mother’s physical and mental health. It also promoted aggressive behaviors, disturbed the hospital staff, and increased the use of drugs. On the other hand, people with efficient coping strategies were successful in dealing with their problems (7).
Coping skills are not innate skills, but rather acquired over time in response to stress and different experiences (8). Coping requires preparation and mobilization of an individual’s energy and effort, achieved by training to help him/her recognize his/her abilities, have adequate social protection, tolerate severe stress when exposed to different living conditions, and perhaps consider the condition as positive (8).
Currently, there is no organized, targeted intervention to support mothers of premature infants during the difficult phase of neonatal hospitalization. Therefore, we used the Creating Opportunities for Parent Empowerment (COPE) program, designed in 2001 by Melnyk for parents of premature infants. This program was implemented in the first days of hospitalization according to the literature. Early intervention is the key to the success of such programs, since it is very difficult to make changes after a communication disorder develops between parents and infant in the NICU (9).
COPE is an educational-behavioral intervention, designed based on the self-regulation and control theories. According to these theories, compatibility is a self-regulating process, and providing information for people in a stressful situation can increase their understanding, predictive power, and confidence about the event. This program also improves emotional and functional coping, which are 2 major coping functions (9). In this regard, Pirbodaghi et al. (2016) found a significant correlation between religious beliefs and adjustment in mothers of cancer children; in other words, by increasing religious beliefs, maternal compatibility improves (10). Climatic, cultural, and social differences are also effective in the relationship between mother and child. Moreover, challenges of mothers in different communities are not the same, and different factors are influential (11).
The COPE program has not been fully implemented in Iran. Therefore, considering the results of previous studies and the importance of stress coping in improving care for mothers of hospitalized infants, we performed this study at Omolbanin Hospital of Mashhad, Iran to determine the effects of empowering mothers of premature infants on their stress coping strategies.
2. Objectives
In the current study, we aimed to evaluate the effects of an empowerment program on the stress coping strategies of mothers of preterm infants, admitted to the NICU.
3. Materials and Methods
This two-group, blinded, nonrandomized, clinical trial was conducted from May to December 2014. The study population consisted of mothers of premature infants, admitted to Omolbanin Hospital of Mashhad, Iran. The inclusion criteria for the mothers were age ≥ 18 years, literacy, and no experience of premature birth. The inclusion criteria for the infants were as follows: 1) gestational age < 37 weeks; 2) birth weight < 2500 g or > 1000 g; 3) lack of critical conditions, such as intraventricular hemorrhage or intracerebral hemorrhage (grades III and IV); 4) singleton pregnancy; 5) length of hospital stay > 1 week or < 1 month; 6) five-minute Apgar score > 7; and 7) lack of evidence on asphyxia. The exclusion criteria were infant’s discharge before the end of the program and infant’s death.
The data collection tool was a questionnaire, consisting of the demographic and background variables, such as cause of preterm delivery, mode of delivery, infant’s gender, and infant’s weight. To collect information related to stress coping strategies, the brief COPE questionnaire, designed by Carver in 1997, was used to determine the coping styles (problem-focused, emotion-focused, and insufficient) at times of stress.
The brief COPE is a self-report tool, consisting of 28 questions, rated on a 4-point Likert scale, ranging from never (1) to always (4). It assesses 3 main styles of coping, including problem-focused, emotion-focused, and insufficient coping; each group of 2 questions is a subset of a subscale. This tool includes a total of 14 subscales. The problem-focused style consists of 6 questions and 3 subscales (counter coping, planned coping, and instrumental support), with scores ranging from 6 to 24. The emotion-focused style consists of 10 questions and 5 subscales (acceptance, psychological support, humor, positive reassessment, and religious effort), with scores ranging from 10 to 40, and the avoidance style consists of 12 questions and 6 subscales (withdrawal behaviors, emotional withdrawal, self-blame, expression of emotions, drug abuse, and denial), with scores ranging from 12 to 48 (12).
The dominant style of each individual was determined by collecting the scores. Those who obtained the same scores in 2 styles used a combination of both strategies. The content validity was measured to determine the validity of the coping questionnaire. The questionnaire was presented to the members of the Faculty of Nursing and Midwifery; after reviews, the required changes were applied. The internal consistency was also measured to assess the reliability of the questionnaire. The questionnaire was presented to 15 mothers, and then, Cronbach’s alpha coefficient was measured (r, 0.80 for the total coping strategy questionnaire).
The sample size was calculated in a pilot study, and the mean comparison formula (95% confidence level; test power, 80%; S1, 6.5; S2, 7.85; M1, 22.23; M2, 17.24) was used:
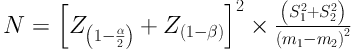
The sample size for each group was calculated to be 32. Considering an attrition rate of 10% per group, 3 more cases were added to each group, and the total sample size was measured to be 35 per group (70 in total). Sampling was carried out at the hospital after obtaining permission from the Ethics Committee of Mashhad University of Medical Sciences, as well as the officials of Omolbanin Hospital. After attending the ward, in order to collect data, the infants who met the inclusion criteria were first determined, and then, the medical records of their mothers were evaluated. If the mother also met the inclusion criteria, the research method was described to her. If she consented to participate in the study, the demographic questionnaire was completed by the researcher through an interview.
To prevent data interaction between the intervention and control groups, the researcher first performed sampling in the control group. Sampling was terminated for 3 weeks, and mothers from the control group were discharged from the hospital. Then, sampling was performed in the intervention group. The information required from the parents was provided in the written format. Also, at each stage, the mothers listened to an audio file (MP3) related to the corresponding stage in the absence of the researcher for about 15 minutes; the information was provided as a booklet for mothers if they wished to use it.
This study was performed in 4 stages: first stage, 1 - 2 days after the infant’s hospitalization; second stage, 2 - 4 days after the first stage; third stage, 1 - 4 days before the infant’s discharge; and fourth stage, 1 week after the infant’s discharge. To assess the stress coping strategies, the mothers completed the questionnaires once 2 - 4 days after the infant’s admission and once before discharge. On the other hand, routine support was applied for the control group, while assessment of coping strategies was similar to the intervention group. The research assistant, who was blind to the objectives and methodology of the study, interacted with the mothers. Data analysis was performed using SPSS version 16. P-value < 0.05 was considered as the significance level.
4. Results
The variables in this study included age, education, number of children, occupation, income, insurance status, infant’s gender, mode of delivery, cause of premature delivery, father’s occupation, and level of education. No significant difference was observed between the groups in terms of demographic variables (Table 1). The mean age of the mothers in the groups was 27 years. Most samples were housewives and had insurance coverage. The level of education was mostly below high-school diploma, and the income level of the family was below 1 million Iranian Tomans. The mean age of the studied infants was 32 weeks, and the mean birth weight was 1850 g.
| Variables | Maximum Frequency | Intervention Group N (%) | Control Group N (%) | P-Value |
|---|---|---|---|---|
| Mother’s education | Elementary and secondary school | 22 | 18 | 0.67 |
| Mother’s occupation | Housewife | 33 | 31 | 1.0 |
| Father’s education | Elementary and secondary school | 20 | 19 | 0.63 |
| Father’s occupation | Self-employment | 23 | 21 | 0.61 |
| Number of children | 1 | 21 | 21 | 0.92 |
| Family income | < 600 000 | 17 | 16 | 0.87 |
| Insurance status | With insurance | 31 | 29 | 0.49 |
| Cause of preterm birth | Respiratory distress | 28 | 27 | 0.95 |
| Mode of delivery | Vaginal delivery | 18 | 23 | 0.22 |
| Infant’s gender | Male | 18 | 23 | 0.22 |
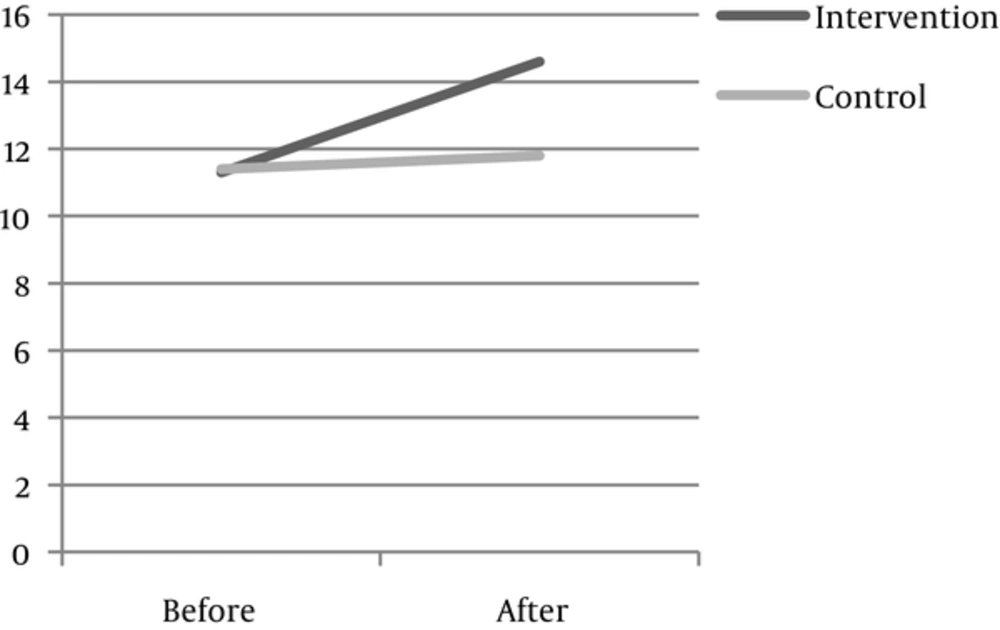
Comparison of the mean scores of problem-focused coping before the implementation of the empowerment program did not show a significant difference between the intervention and control groups (P = 0.83). However, the mean score of problem-focused coping increased in the intervention group after the program. The statistical tests showed a significant difference in the mean score of problem-focused coping in the intervention group before and after the program (P < 0.001), while no significant difference was reported in the control group (P = 0.67) (Table 2).
| Stages | N | Groups | P-Value (Student T Test) | |
|---|---|---|---|---|
| Intervention | Control | |||
| Mean ± SD | Mean ± SD | |||
| Before intervention | 35 | 11.3 ± 3.4 | 11.4 ± 3.2 | P = 0.83 |
| After intervention | 35 | 14.60 ± 4.8 | 11.8 ± 4.9 | P = 0.02 |
| P-value (paired t test) | P = 0.64 | P = 0.001 | ||
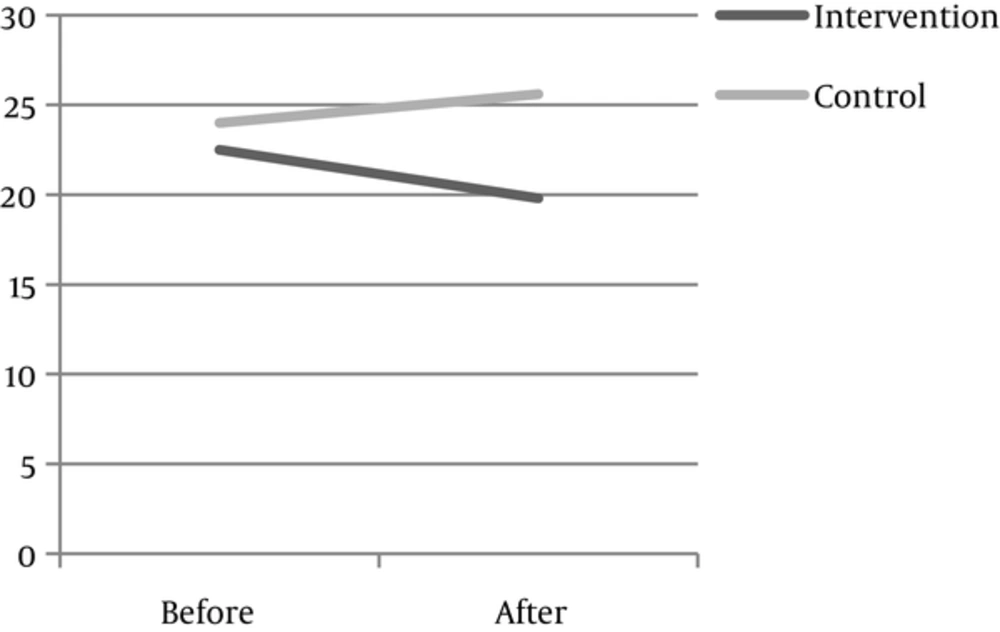
According to Table 3, comparison of the mean score of emotion-focused coping before the empowerment program did not show a significant difference between the intervention and control groups (P = 0.78). However, the mean score of emotion-focused coping decreased in the intervention group after the program, and showed a significant difference with the mean score of emotion-focused coping before the program (P = 0.01). The mean score of emotion-focused coping increased in the control group after the intervention; however, the difference was not significant (P = 0.19).
| Stages | N | Groups | P-Value (Student T Test) | |
|---|---|---|---|---|
| Intervention | Control | |||
| Mean ± SD | Mean ± SD | |||
| Before intervention | 35 | 22.5 ± 9.0 | 23.9 ± 8.6 | P = 0.78 |
| After intervention | 35 | 19.8 ± 7.0 | 25.6 ± 8.8 | P = 0.003 |
| P-value (paired t test) | P = 0.01 | P = 0.19 | ||
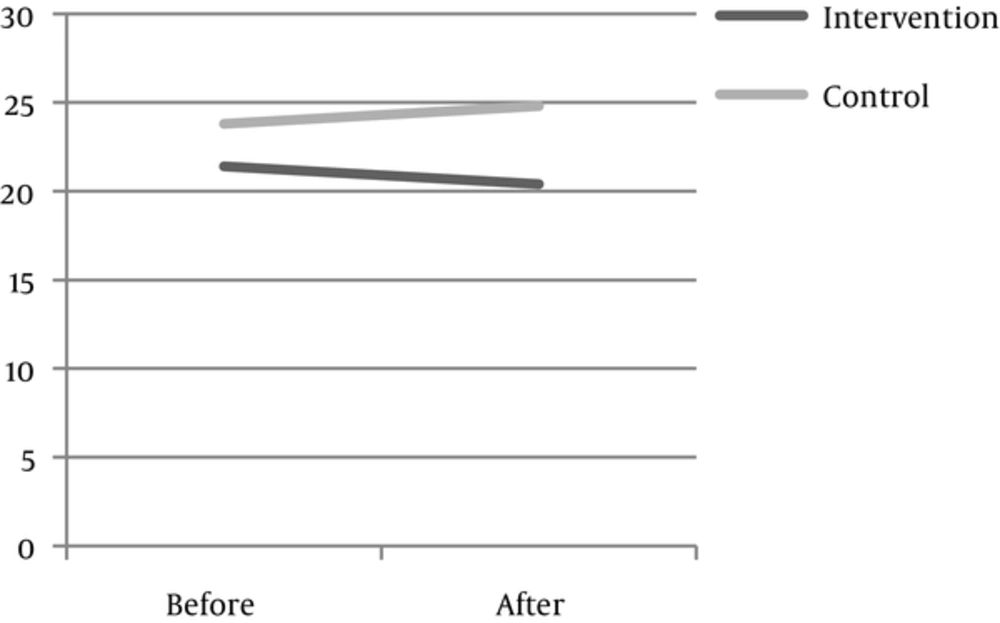
According to Table 4, comparison of the mean score of insufficient coping before the empowerment program did not show a significant difference between the intervention and control groups (P = 0.19). However, the mean score of insufficient coping decreased in the intervention group after the program and showed a significant difference with the mean score of insufficient coping before the intervention (P = 0.004). On the other hand, the mean score of insufficient coping increased in the control group after the intervention, and the difference was significant (P = 0.008).
| Stages | N | Groups | P-Value (Student T Test) | |
|---|---|---|---|---|
| Intervention | Control | |||
| Mean ± SD | Mean ± SD | |||
| Before intervention | 35 | 21.4 ± 7.6 | 23.8 ± 7.6 | P = 0.19 |
| After intervention | 35 | 20.4 ± 6.5 | 24.8 ± 7.2 | P = 0.01 |
| P-value (paired t test) | P = 0.004 | P = 0.008 | ||
5. Discussion
The present study showed that the empowerment program for mothers of premature infants increased the use of problem-focused coping. The results of the present study are consistent with the study by Shaw et al. (2013), entitled “Parental coping in the neonatal intensive care unit”, which found a significant relationship between education and stress coping strategies; individuals who received more training used problem-focused strategies more frequently than emotion-focused or insufficient strategies (7). The repeated training sessions are similar to the present research, which can influence stress coping strategies in mothers. This study showed that the coping program for mothers of premature infants could improve their coping strategies.
The results of a study by Howell et al., (2015) on the effects of support sources on the compatibility and stress of parents of premature infants at the time of NICU admission (13) are consistent with the present findings. The results of their study suggest that family-centered interventions, besides mental and psychological support, can be helpful in efficient coping and stress alleviation among parents of premature infants. This study is similar to the present research in terms of grouping, but is different from the present study regarding the type of intervention.
The results of a study by Galeano and Carvajal (2016), entitled “The effect of empowerment program on strategies of stress coping, quality of life, and compatibility with parental role in HIV-infected mothers”, are consistent with the present findings. In this study, mothers received training about neonatal care, parental role, and stress management for 6 weeks. The results showed that the intervention group had a significantly increased level of efficient coping (problem-focused coping), quality of life, and consistency with the parental role in comparison with the controls (14); the stress coping strategies were assessed using the Jalinus questionnaire. One of the common aspects of this study with our research is repeated training, which can be effective in the use of problem-focused coping in mothers. The results of their study (2000) are consistent with the present study, showing a reduction in emotion-focused coping in the intervention group; however, the difference between the groups was not significant (14).
Moreover, Peek et al. (2010) in a review study, entitled “Coping interventions for parents of children newly diagnosed with cancer: An evidence review with implications for clinical practice and future research”, showed that medical and nursing teams should start social and psychosocial interventions within 2 to 16 weeks after diagnosis to improve stress coping in parents of children (15).
In the present study, the mean score of emotion-focused coping decreased in the intervention group after the empowerment program; the difference was statistically significant (P < 0.001), while no significant difference was found in the control group (P = 0.19). Therefore, implementation of empowerment programs for mothers of premature infants can lead to the reduced application of emotion-focused coping strategies. The results of the study by Shaw et al. (2013) are in line with the results of the present research and indicate that training can reduce the use of emotion-focused coping strategies (7).
Melnyk et al. (2006) in a study on the effects of an empowerment program on the mental health of mothers of premature infants, stated that implementation of the empowerment program was effective in the mood and emotional coping of mothers of premature infants (16). The similarities of these studies in terms of demographic characteristics and training content presented to mothers might account for the consistency in the results. The findings reported by Pineil et al. (2000) are also similar to the present study and show that social and family support for parents of premature infants can reduce the stress caused by the birth of premature infants and decrease insufficient coping (13).
On the other hand, the results of a study by Mendelson et al. (2013) are different from the results of the present study. This study on the effects of preventive interventions on depression, mood, and coping strategies in the perinatal period showed that use of insufficient coping increased in the intervention group, contrary to our expectations (17). Additionally, Al-Gamal et al. (2017), in a study on the stress and coping strategies of Saudi nursing students during clinical education, showed that use of effective coping strategies in nursing students could promote the quality of care for the patients (18).
One limitation of this study is that it was conducted in a single hospital, the conditions of which might have affected the results. Therefore, further studies are recommended in other hospitals.
5.1. Conclusion
The results of the present study showed that the intervention group, who participated in the empowerment program, used more problem-focused coping and less emotion-focused or insufficient coping strategies. Considering the effectiveness of this program in improving stress-coping strategies for premature birth, implementation of such programs as standard care is suggested to improve stress coping strategies.