1. Background
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is highly transmissible and causes coronavirus disease 2019 (COVID-19), which is often lethal and has reached a pandemic scale worldwide in 2020 (1). In December 2019, the first case of COVID-19 was reported in Wuhan, China, and the disease rapidly spread to the rest of the world. In January 2020, the World Health Organization declared COVID-19 as a public health emergency threatening all individuals of the world (2). Therefore, the COVID-19 pandemic represents a threatening and potentially traumatic event, as it can lead to the hospitalization of numerous patients and even death.
The COVID-19 is associated with multiple psychiatric problems in several groups, including patients with COVID-19 and patients with psychiatric disorders predating the pandemic, requiring quick and immediate management of mental health (3-5). A few studies describe that psychiatric symptoms and disorders arise during the COVID-19 epidemic due to biological and psychosocial factors (6-8). A wide variety of neuropsychiatric symptoms can appear during COVID-19 infection and might be related to direct damage to neurological tissues or due to environmental issues, cytokine release, respiratory insufficiency, critical illness, and side effects of pharmacological treatment or exacerbation of previous neuropsychiatric illness (9).
Currently, the focus is mainly on preventing COVID-19 infection and discussing issues related to physical health consequences. Therefore, COVID-19 clinics are being established in different places to address the physical health consequences of the pandemic. However, it is important to note that although some infected patients face life-threatening physical consequences, a considerable number of infected patients face negative mental consequences as a result of the outbreak. It seems that mental health providers have not been highly involved in the treatment of those affected by the pandemic, and mental healthcare in these patients does not appear to be adequate (10, 11).
2. Objectives
Since there is limited information on psychiatric assessments in patients with COVID-19, this study aimed to evaluate the extent of psychological care provided to COVID-19 patients admitted to a hospital, the most common reasons for psychiatric counseling, and the results of psychiatric counseling retrospectively. It is hoped that by evaluating psychiatric counseling and identifying the main psychiatric problems in these patients, more comprehensive interventions for patients during hospitalization can be considered, along with more comprehensive psychiatric assessments and interventions for new patients.
3. Methods
3.1. Study Design and Data Collection
Following the approval of the Ethics Committee of Iran University of Medical Sciences, Tehran, Iran, this retrospective observational study was conducted in one of Tehran’s largest referral hospitals for COVID-19 patients (Rasoul-e-Akram hospital). This study examined the electronic medical records of all COVID-19-positive patients admitted to the hospital within April 1 and September 30, 2020 (approximately 2200 cases).
The patients who requested psychiatric consultation while being hospitalized and had a confirmed laboratory diagnosis of COVID-19 (either a positive result for immunoglobulin G/immunoglobulin M antibodies against SARS-CoV-2 in a blood test or identification of SARS-CoV-2 ribonucleic acid with a real-time reverse transcription-polymerase chain reaction of throat swab samples) were chosen and analyzed in this study. Suspected COVID-19 patients were excluded from the study. Demographic data, such as age, gender, marital status, educational level, previous psychiatric and/or medical comorbidities (e.g., hypertension, diabetes, dyslipidemia, heart disease, chronic kidney disease, immunosuppression, cancer, and neurological diseases), substance abuse and smoking habit, and the reason for seeking psychiatric consultation from the physician (i.e., primary psychiatric symptom), were reported. Final psychiatric diagnosis according to the diagnostic and statistical manual of mental disorders, 5th edition (DSM-5), psychiatrist’s recommendations for pharmacological and nonpharmacological interventions in response to counseling, taken actions, and results were documented. Finally, the information collected from 112 patients was examined. Two experienced psychiatrists collaborated to collect the data using a standardized case-report form. Before the formal study, the psychiatrists were trained on how to collect the data from electronic medical records.
3.2. Ethical Statement
This study was approved by the Ethics Committee of the Iran University of Medical Sciences, Tehran, Iran (code: IR.IUMS.REC.1399.594). This was a retrospective and noninterventional study. No experiments were carried out on human subjects. A waiver of written informed consent was obtained since all the data were collected retrospectively and anonymously.
3.3. Statistical Analysis
The characteristics of COVID-19 patients with and without previous psychiatric disease were analyzed and compared using descriptive statics. The chi-square test or Fisher’s exact test was used to compare two groups of COVID-19 patients with and without previous psychiatric illness. The independent-sample t-test and Mann-Whitney u test were used to compare the continuous variables between these two groups of patients according to their normal distribution and deviation distribution (a skewed distribution), respectively. The statistical significance level was set at less than 0.05 (two-sided). Confidence intervals (CI) were calculated if indicated. All data analyses were carried out using SPSS software (version 24.0).
4. Results
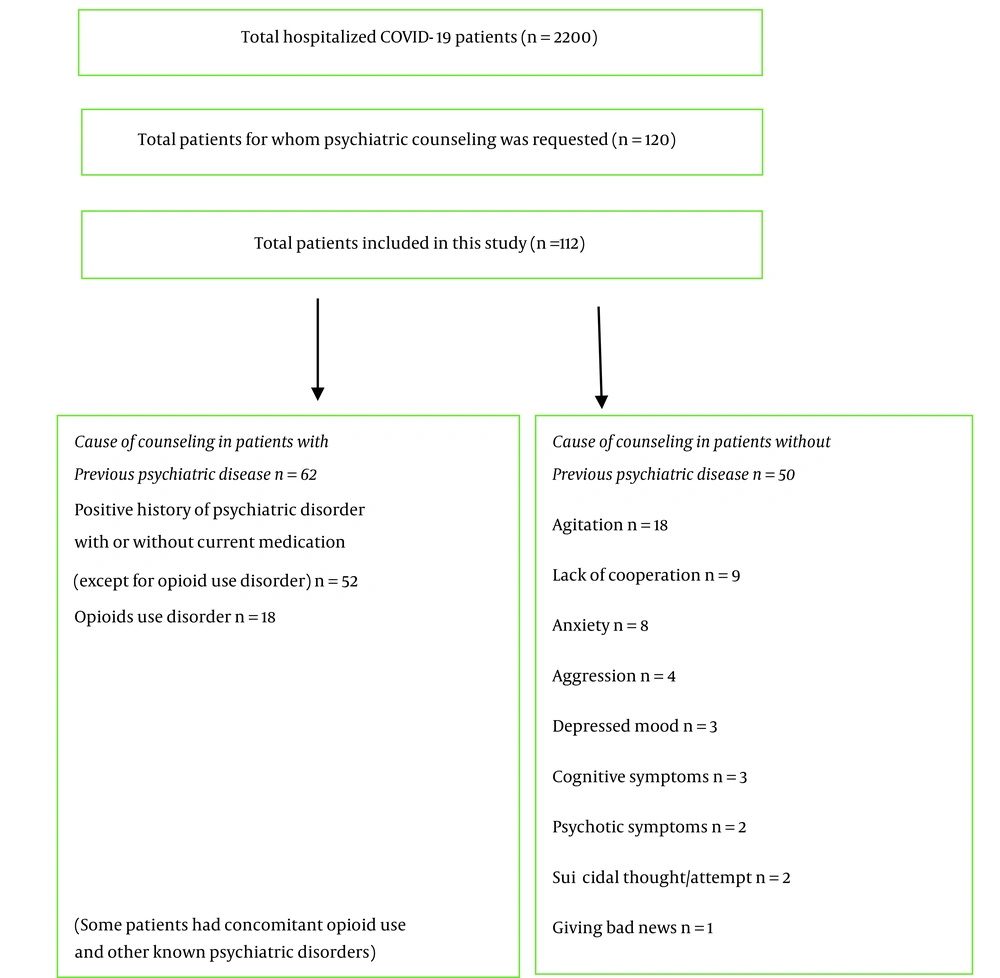
After a detailed review of medical records of 2200 COVID-19 patients during that period, 120 patients were identified for whom psychiatric consultation was requested. In other words, psychiatric consultation was requested for 5.45% of admitted patients with COVID-19. Eight patients were removed due to uncertain COVID-19 infection and/or incomplete data. Finally, 112 cases were included in the study, among whom psychiatric consultation was requested for 62 patients due to a positive history of psychiatric diseases, including substance use disorders, and for 50 patients due to new-onset psychiatric symptoms during hospitalization without any known psychiatric illness.
According to the DSM-5, occasional consumption of substances, including alcohol or tobacco smoking, was not considered a psychiatric disorder. In the current study, the most common reason for requesting consultation was a positive history of psychiatric disorder. Opioid use disorder and agitation were ranked second (Figure 1). The most common diagnosis in patients with a positive history of a psychiatric disease was bipolar disorders (33.9%), followed by opioid use disorder (29%). Adjustment disorder (54%) and delirium (26%) were the most common diagnoses in patients without a history of psychiatric disease. It should be noted that the mean age of patients with a positive history of psychiatric disorders was significantly lower than other patients (54.95 years in comparison to 63.02 years). Furthermore, the prevalence of medical comorbidities, such as hypertension, heart diseases, dyslipidemia, and kidney diseases, in the patients without a history of mental illness was higher than in the other group (Table 1). The study results showed that the mortality rate was higher in patients with a positive history of psychiatric issues; nevertheless, there was no statistically significant difference in mortality between psychiatric illnesses (Table 1). Figure 1 depicts the distribution of the reasons for counseling requests and primary psychiatric symptoms. Tables 1 and 2 show the characteristics of patients and final diagnosis and interventions, respectively.
| Variables | Patients with a Positive History of Psychiatric Illness (n = 62) | Patients Without Previous Psychiatric Illness (n = 50) |
|---|---|---|
| Age (y) | 54.95 ± 16.51 b | 63.02 ± 17.46 b |
| Gender | ||
| Male | 40 (64.5) | 31 (62) |
| Female | 22 (35.5) | 19 (38) |
| Marital status | ||
| Single | 14 (22.6) | 1 (2) |
| Married | 34 (54.8) | 37 (74) |
| Divorced/widowed | 14 (22.6) | 12 (24) |
| Educational level | ||
| Illiterate | 12 (19.4) | 13 (26) |
| Under diploma | 29 (46.8) | 18 (36) |
| Diploma/associate degree | 17 (27.4) | 13 (26) |
| Bachelor’s degree and higher | 4 (6.5) | 6 (12) |
| Employment | ||
| Housewife | 18 (29.0) | 17 (34) |
| Unemployed | 19 (30.6) | 12 (24) |
| Freelance | 11 (17.7) | 11 (22) |
| Employee | 2 (3.2) | 5 (10) |
| Retired | 12 (19.4) | 5 (10) |
| Alcohol and/or substance abuse | ||
| Tobacco smoking b | 26 (41.9) | 10 (20) |
| Alcohol use/abuse | 6 (9.7) | 2 (4) |
| Opioid use disorder | 18 (29) | - |
| Stimulant/Inhalant use disorder | 7 (11.3) | - |
| Comorbidities | ||
| Hypertension b | 17 (27.4) | 29 (58) |
| Diabetes mellitus | 15 (24.2) | 19 (38) |
| Dyslipidemia b | 9 (14.5) | 19 (38) |
| Heart disease b | 6 (9.7) | 15 (30) |
| Chronic kidney disease b | 3 (4.8) | 7 (14) |
| Malignancy | 3 (4.8) | 1 (2) |
| Neurological disease | 10 (16.1) | 9 (18) |
| Rheumatologic disease | 1 (1.6) | 2 (4) |
| Pulmonary disease | 1 (1.6) | 1 (2) |
| Thyroid disease | 4 (6.5) | 4 (8) |
| Previous psychiatric illness status at the time of hospitalization | ||
| Active | 35 (56.5) | - |
| Partial remission | 19 (30.6) | - |
| Complete remission | 8 (12.9) | - |
| Positive history of psychiatric admission | 31 (50) | - |
| Transfer from psychiatric service to COVID-19 ward | 5 (8.1) | - |
| ICU admission | 16 (25.8) | 20 (40) |
| Outcome | ||
| Death | 17 (27.4) b | 9 (18) b |
| Discharge | 39 (62.9) b | 41 (82) b |
| Transfer to psychiatric service | 6 (9.7) b | - |
Abbreviations: COVID-19, coronavirus disease 2019; ICU, intensive care unit
a Values are expressed as mean ± SD or No. (%).
b P < 0.05
| Variables | Patients with a Positive History of Psychiatric Disease (n = 62) | Patients Without a Previous Psychiatric Disease (n = 50) |
|---|---|---|
| Diagnosis | ||
| Bipolar disorders | 21 (33.9) | - |
| Adjustment disorder | - | 27 (54) |
| Opioid use disorder | 18 (29) | - |
| Psychotic disorders | 11 (17.7) | 1 (2) |
| Depressive disorders | 9 (14.5) | 3 (6) |
| Delirium | 7 (11.3) | 13 (26) |
| Anxiety disorders | - | 3 (6) |
| Stimulant/inhalant use disorder | 7 (11.3) | - |
| Ruling out psychiatric disorders | - | 3 (6) |
| Cluster B personality disorder | 5 (8.1) | - |
| Others b (some patients had multiple simultaneous diagnoses) | 8 (12.9) | - |
| Pharmacological intervention | ||
| No need for pharmacotherapy | 3 (4.8) | 10 (20) |
| Antipsychotics | 39 (62.9) | 23 (46) |
| Mood stabilizer | 27 (43.5) | - |
| SSRIs | 16 (25.8) | 8 (16) |
| Benzodiazepines | 15 (24.2) | 18 (36) |
| Methadone | 14 (22.6) | - |
| Anticonvulsants | - | 1 (2) |
| TCAs | 1 (1.6) | - |
| Antihistamines | 1 (1.6) | 2 (4) |
| Others | 2 (3.2) | - |
| Nonpharmacological intervention | 11 patients (17.7%) received nonpharmacological interventions (e.g., psychoeducation and supportive psychotherapy) | 42 patients (84%) received nonpharmacological interventions (e.g., psychoeducation and supportive psychotherapy) |
Abbreviations: SSRIs, selective serotonin reuptake inhibitors; TCAs, tricyclic antidepressants
a Values are expressed as No. (%).
b Obsessive-compulsive disorder, anxiety disorders, posttraumatic stress disorder and intellectual disability
5. Discussion
This new study was conducted to determine the most common reasons for psychiatric counseling, evaluate psychiatric counseling performed for COVID-19 patients, and compare the common psychiatric symptoms, psychiatric diagnoses, and outcomes among COVID-19 patients who received psychiatric counseling between patients with and without previous psychiatric diseases.
In the current study, psychiatric counseling was requested for only 5.45% of admitted COVID-19 patients, more than half of which were related to cases already known to have psychiatric illnesses. According to previous studies, numerous COVID-19 patients have psychological symptoms and issues, and COVID-19 is frequently correlated with neuropsychiatric diagnosis during the acute phase of the disease (12, 13). A cross-sectional study conducted on 199 COVID-19 patients admitted to Sari hospitals in Iran to examine posttraumatic stress disorder (PTSD) symptoms through the PTSD Checklist for DSM-5 showed that the prevalence of PTSD was 19.1% (14). Another cross-sectional study that evaluated the prevalence and severity of depression, anxiety, stress (based on the Depression Anxiety Stress Scale-21), and stress perception (based on Perceived Stress Scale 4) among 106 inpatients with COVID-19 infection in Alborz, Iran, revealed that 97.2% of patients had some degree of depression and 85.8% of the patients had severe depression. All patients (100%) had anxiety, and 97.1% had some degree of stress. Moreover, 73.6% of patients had high levels of perceived stress (12). Therefore, the low percentage of psychiatric counseling in this study might indicate neglect of psychological issues in these patients.
Agitation, lack of cooperation with care providers, and anxiety were the most common psychiatric symptoms in patients with new-onset psychiatric symptoms, leading to requesting psychiatric counseling, and adjustment disorder was the most common psychiatric diagnosis in this group. Since 6% of patients with agitation and lack of cooperation did not receive a formal diagnosis during a psychiatric evaluation, and 20% of patients did not need pharmacotherapy, their symptoms were justified by a lack of awareness and information about their disease’s condition. In the present pandemic, this issue could justify the importance of psychoeducation and psychological care for these patients.
One retrospective cohort study of 62354 COVID-19 patients in the USA revealed that a psychiatric diagnosis in the previous year was associated with a higher incidence of COVID-19 diagnosis (relative risk = 1.65, 95% CI 1.59 - 1.71; P < 0.0001), and the risk was independent of known physical health risk factors for COVID-19 (15). Only 12% of patients with a prior documented psychiatric condition were in complete remission in the current study, which might suggest a higher incidence of COVID-19 in uncontrolled psychiatric patients, and psychiatric diagnosis might be an independent risk factor for COVID-19 (15, 16).
In the current study, despite the higher mean age and higher prevalence of comorbidities, such as hypertension, heart diseases, dyslipidemia, and kidney diseases, in the population without a history of mental illness than in the other group, the mortality rate was higher in patients with a positive history of psychiatric issues. This result is consistent with the results of one cohort study conducted on 1685 hospitalized COVID-19 patients in the northeast region of the United States, indicating that after controlling for demographic characteristics, medical comorbidities, and hospital location, the risk of mortality remained significantly greater among patients with a psychiatric disorder than those with no psychiatric diagnosis (hazard ratio = 1.5; 95% CI, 1.1 - 1.9; P = 0.003) (17). Unlike another study that showed that COVID-19 mortality was higher in patients with schizophrenia than in patients with other psychiatric disorders (18), in the current study, there was no statistically significant difference in mortality between psychiatric illnesses.
Although the present study provides important data on the psychological problems of hospitalized COVID-19 patients, there are still several limitations. Since the data were collected retrospectively, there might be selection bias and some missing crucial details. Furthermore, since the study was a descriptive one, it could not be concluded that the patients’ psychological symptoms were triggered by the SARS-CoV-2 infection or by other factors, such as cross-immunity, inflammatory reactions, or side effects of treatments. Finally, the data were collected from only one hospital, and the small sample size might limit the generalization of the results. Since this study was carried out in a hospital, the prevalence of psychological issues among COVID-19 patients in the community could differ, and any findings should be interpreted accordingly.
5.1. Conclusions
Despite the high prevalence of psychiatric problems in patients with COVID-19, in the current study, psychiatric counseling was limited to a small number of patients, including those with a positive history of psychiatric illnesses and prominent psychiatric symptoms. It is suggested that first-line physicians be aware of possible psychiatric complications since the global emergency is expected to last. All COVID-19 patients should be assessed mentally, according to the recommendations of this study. It is also recommended that psychiatrists be included in COVID-19 response teams on a regular basis to ensure the adequate early detection and treatment of psychiatric manifestations, thereby improving psychiatric outcomes. Accordingly, it is required to further investigate the mechanisms of mental injuries and their long-term effects.