1. Introduction
Obsessive-compulsive disorder (OCD) is one of the most prevalent and debilitating psychiatric disorders (1). The symptoms of OCD are extremely broad and varied. Scrupulosity is a type of this disorder in which there is an obsessional fear of thinking and behaving against religious beliefs and God’s commandments (2).
The OCD treatment guidelines and research have introduced cognitive-behavioral therapy (CBT) with an emphasis on exposure and response prevention (ERP) as the psychological intervention of choice for OCD, including the scrupulosity type (2, 3). However, the nature of treatments received by OCD patients does not fulfill the minimum requirements for CBT treatment, and many sessions do not include exposure, with an emphasis on homework (4). In addition, it has been shown that 18% - 30% of patients received treatment with exposure techniques (in 2 years) (4). Furthermore, treatment barriers, including the patients’ feeling of shame, fear of being labeled, and the lack of access to mental health professionals, can contribute to not seeking appropriate treatments (5). According to these findings and due to the discrepancy between the prevalence of this disorder and the number of individuals receiving treatment, mental health services are still inappropriate and insufficient despite abundant knowledge about OCD treatment (4).
Technology-based interventions can greatly decrease the limitations mentioned above. For instance, we hope different evidence-based treatments become remotely available to patients using these treatments (6). In addition, technology-based interventions, especially those using applications, provide objective feedback for the client about contribution to problems and also a response to treatment and raise ERP treatment success and the quality of CBT with an emphasis on ERP (7). The effect of technology-based interventions on OCD has also been examined. These studies have pointed out the limitations of the literature and the need for further examining the efficacy of these types of interventions for OCD treatment (8). However, there have been no studies on the impact of technology-based interventions on scrupulous patients. According to our previous investigations, only limited research has confirmed the influence of CBT on reducing the symptoms of scrupulosity patients (9, 10).
Farhood et al. demonstrated that although CBT reduced obsessive symptoms in both groups of patients with contamination and religious obsessions, the scrupulosity group was less responsive than the contamination group (11). The logic of the present study can be summarized as “Scrupulosity is a common type of OCD which has been commonly reported to have a high prevalence in religious countries”. The prevalence of scrupulosity is reported to be 50% - 90% in Iran (12). These individuals have a weak prognosis and, compared to other types of OCD, are considered resistant patients (13). Therefore, we need to pursue treatments with higher efficacy for these patients. One of the critical problems in treating OCD is that because these patients get anxious only in their homes or other living areas, many do not respond to ERP in therapy (14). Compulsions of scrupulosity patients are also mainly observed in specific areas of their lives. Consequently, a method for augmenting treatment response and reducing the resistance of these patients could be designing treatments in which ERP is performed in their real living space in the presence of a therapist.
In this study, we tried to design a type of technology-based treatment to improve the quality of treatment. To this end, this case is reported as the treatment procedure of a Muslim client with scrupulosity in the Iranian population using remote therapy via the internet. The therapist was present via video call in all sessions, and a treatment application was also applied. The results of this case report can lay the ground for future research on scrupulosity.
2. Case Presentation
The patient was a 37-year-old married woman with a bachelor’s degree in Persian literature and a housewife. She sought treatment from the clinic because of mostly religious obsessions. First, the patient was assessed by the psychiatrist and received an OCD diagnosis based on DSM-5 criteria. According to the psychiatrist, the patient’s obsessions were of scrupulosity. Afterwards, the patient was referred to a psychologist for therapy. The patient was evaluated utilizing the Structured Clinical Interview of Axis I Disorders, and the patient filled out the study’s questionnaires for 6 weeks.
The reason for choosing this patient to be examined in this research was that based on the diagnosis of the psychiatrist and psychologist, she fulfilled all the OCD criteria. She was a religious person living in the religious society of Iran, and her obsessions and compulsions had a religious theme. Finally, the patient gave full consent to participate in the treatment-research sessions held as technology-based psychotherapy.
The individual was preoccupied with religious obsessional thoughts, followed by obsessive behaviors. Most obsessive behaviors occurred in her own home and her parents’ house. The patient was susceptible to her home space and had divided the house into two sections “pure” (clean) and “impure” (unclean). Most of the patient’s thoughts revolved around the thought that “she might contaminate parts of the house which could lead to her and her husband’s prayer and other religious rituals not being accepted by God and commit a sin involuntarily then be punished by God”.
Some of the obsessive behaviors that the client did both in her own house and her parents’ house were avoiding touching certain parts of her own and her parents’ house (e.g., rugs and sofas), washing hands excessively after using the bathroom, avoiding touching outside clothes because of the probability of them being unclean, spend a long time to perform her abolitions because of having doubts about whether she had completed them correctly or not, and call a religious authority to ask for reassurance.
The patient’s obsessive behaviors existed at a lower degree since adolescence but exacerbated after the death of one of her family members about 8 years ago. She had been using Fluvoxamine for the past year. Treatment was carried out online weekly, and the therapist contacted the patient at her own house via video call. The treatment application, which had previously been designed by the first and second researchers, was also used as an assistive treatment tool between sessions. Homework reminders were sent daily, and the patient sent completed homework to the therapist and received feedback through the application installed on the patient’s phone. The application had an educational and hierarchical section where the patient’s educational information and specific hierarchy would be uploaded. Moreover, the application included a “questionnaires” section in which the patient could complete all the research questionnaires weekly. The treatment sessions were conducted online and with the help of the treatment application based on the Abramowitz model (15) for treating patients with religious obsessions. The sessions lasted 60 and 90 minutes. The patient was at her home for all the sessions, with several sessions of exposure in her parents’ house, and was in contact with the therapist via video call.
Session 1: In the first session, scrupulosity disorder, obsessions, and compulsions were explained to the patient, and a thorough list of her obsessions and compulsions were identified. Based on that, specific and realistic goals were designed with the help of the patient. In addition, the patient’s cognitive-behavioral case conceptualization was also completed based on Abramowitz’s cognitive-behavioral model for scrupulosity (15). The patient became aware of the role of uncertainty intolerance, anxiety, and compulsions in perpetuating the disorder and also the role of her dysfunctional appraisal of normal intrusive thoughts.
Session 2: The goal of this session was to explain the rationale for treatment and increase the patient’s motivation to be involved in the treatment. The cognitive-behavioral model was introduced with an emphasis on exposure and response prevention. In order to raise the patient’s motivation for change, the pros and cons of “change vs. staying in the same position” were mentioned.
Sessions 3 and 4: Psychoeducation with Socratic questioning. These sessions aimed to cognitively challenge the rigid beliefs of the patient regarding committing sins and divine punishment. The patient’s view of sin compared to the view of most religions on sin was examined. Furthermore, the patient was made aware through critical thinking that her definition of faith differed from genuine faith. The definition of faith is to submit to God’s word, while the patient was submitting to her own rules by performing rigid, obsessive acts. These sessions challenged the incongruity between religious rules and obligations, including impurity and purification with the client’s compulsions.
Session 5: From the fifth session onward, all sessions took 90 min. The hierarchy of ERP sessions was identified, and the first exposure session with the anxiety and doubt degree of 5 began. Exposure was performed with the door knob of the toilet and the rug next to the toilet. The therapist was virtually present for 90 min and tried to encourage her to perform exposure and help her not get distracted. During all the weeks of treatment, the application reminded the patient to do homework via text messages, and exposure outcomes and the duration of uncertainty tolerance were sent to the therapist. The therapist would then send encouraging text messages to the patient in case of successful completion of homework.
Sessions 6 and 7: According to the hierarchy, the patient spent these two sessions at her parents’ house and, with the therapist’s help, was exposed to sofas. The door handles of her parents’ house and sat in the parts of the house that she had avoided sitting on for a long time because they were considered contaminated (impure).
Session 8 to 11: In these sessions, the patient was exposed to touching outdoor clothes with wet hands considered “impure” and then touching parts of the house considered clean by the patient. Moreover, performing abolitions inside the toilet and having doubts about whether or not she had completed them correctly, not repeating them, and deciding to pray were practiced. Praying in part of the house which the patient regarded as “impure”, going to the toilet with prayer clothes, immediately praying with those clothes on, and going to the toilet, touching the toilet’s wall, and then touching different parts of the house were also performed.
There was a follow-up 3 months after the end of treatment.
One of the potential sources of bias in this research was the small sample size because of the case study method. There was a concern that this sample would not represent the population of patients with scrupulosity. To minimize this limitation, the case was chosen with consideration, the clinical diagnosis of scrupulosity was confirmed by the psychiatrist and psychologist, and we tried to choose a participant as a sample whose complaints were among the common complaints of patients with scrupulosity. In order to minimize information bias, we tried to reduce the interval between the measurements of variables. The participant had to fill out the questionnaires at the interval between sessions. To decrease bias in the results, an individual other than the therapist examined the questionnaires and charts. In addition, at the end of therapy and follow-up, a psychiatrist also evaluated the positive changes in the patient’s symptoms.
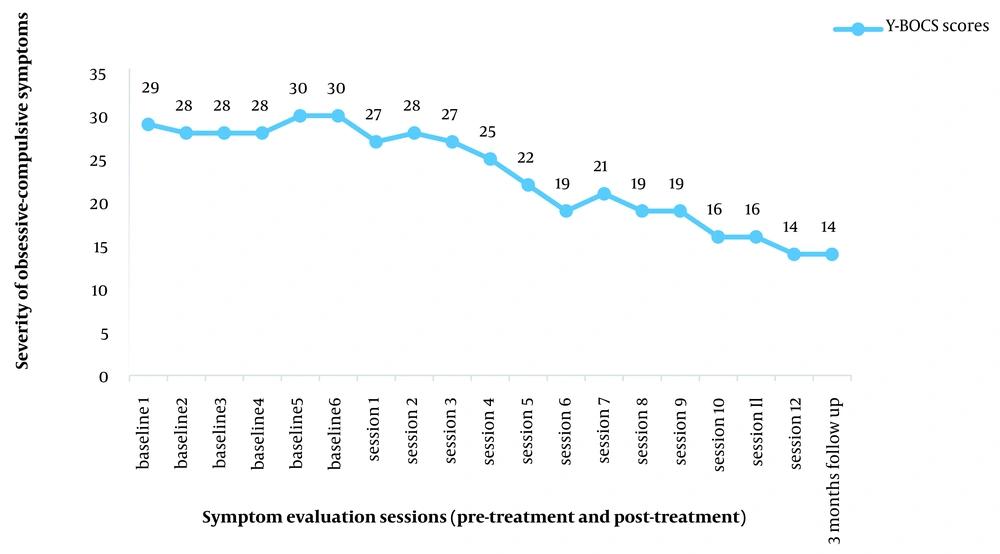
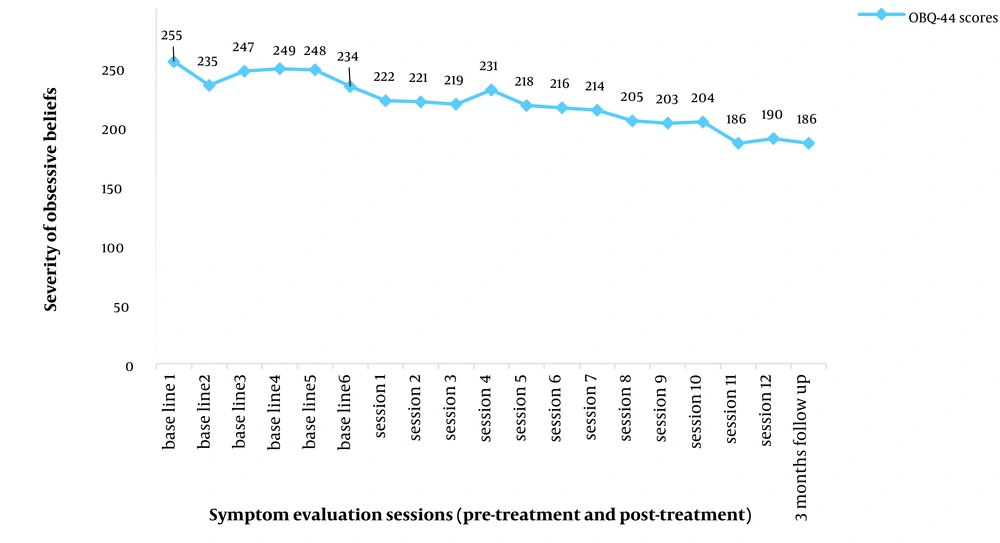
Results showed that the client’s scores on the Y-BOCS scale declined from pre-treatment to post-treatment, and the scores revealed that the symptoms decreased from severe to low (< 16 low in Y-BOCS). The results remained the same from post-treatment to follow-up. The scores of obsessive beliefs dropped from 255 on the baseline to 190 in post-test and 186 in follow-up, indicative of a decrease in obsessive beliefs during treatment. Moreover, BAI scores diminished from the severe range (26 - 63 in pre-treatment) to medium (16 - 25 medium anxiety levels in BAI) in post-treatment. This drastic change from severe to medium from pre-test to post-test was also found in depression scores (15 - 24 medium range in BDI). Both scores of anxiety and depression had a slight increase from post-treatment to follow-up. Furthermore, the quality of life scores rose from 47 at baseline to 78 in post-test, which changed to 75 at follow-up. Diagrams of obsessive-compulsive symptoms and obsessive beliefs are shown in Figures 1 and 2.
3. Discussion
The present study aimed to administer CBT with an emphasis on remote exposure and in-vivo exposure in the real living space of a patient with scrupulosity type OCD. The resultant outcomes indicated a decrease in obsessive symptoms and obsessive beliefs, as well as a medium decline in depressive and anxiety symptoms and an increase in the patient’s quality of life with scrupulosity.
In the current research, it seemed that the presence of a therapist in all virtual sessions and exposure situations significantly helped the participant to face spaces at home that she used to avoid previously. The patient could not face these spaces alone because she had avoided these situations for years. More importantly, she considered being exposed to specific situations in her parent’s house impossible, and the therapist’s presence in online sessions helped her face various triggering situations. Past research has shown that the therapist’s support, encouragement, and guidance in treatment sessions via the internet lead to greater treatment efficacy (16). Abramowtiz and Jacoby evaluated the effect of a therapist’s presence on the course of OCD treatment (17). They demonstrated that exposure under the supervision of a therapist compared to exposure controlled by the patient himself/herself led to better treatment outcomes. The therapist’s presence in the exposure sessions results in more concentration on triggers, maximizing the effects of exposure. In addition, research has shown that for ERP to be effective in the most severe cases, exposure must be in various situations (17).
It seems that by reducing the obsessive symptoms and beliefs, the depressive symptoms of our case decreased to some extent. The reduction in depressive symptoms can be attributed to removing limitations resulting from OCD symptoms. With the improvement of symptoms, the patient could attend housework and religious activities, which according to Bandura’s theory (18), enhance self-efficacy and, in turn, improves the participant’s mood. The increase in the quality of life scores also confirms this issue. However, because CBT is a structured treatment and the therapy process was exclusively focused on the patient’s OCD, and depressive symptoms were not directly targeted as the primary goal of treatment, the reduction in depressive symptoms was in the average range. The average reduction in anxiety symptoms can be attributed to provoking anxiety in exposure sessions.
One of the limitations of the present study was the small sample size which limits the possibility of data generalization. It seems that the results of this study can be generalized, with caution, to the population of patients with scrupulosity who have similar symptoms to the case under study. Another limitation of this research was its short-term follow-up. In addition, it was possible that the participant would not fill out the questionnaires carefully, or there could be a tendency to over- or under-report symptoms because self-report questionnaires were used.
One of the strengths of this study is that we tried to have a step-by-step, deep, and comprehensive view of a patient’s treatment process with scrupulosity by considering the new model of CBT in a real setting and comparing the patient’s treatment progress with baseline. This treatment model for scrupulosity has not been reported in other studies. According to the high prevalence of scrupulosity in the Iranian population, this treatment model can be helpful for these individuals and raise the treatment success. Finally, we recommend that future researchers repeat this treatment model in more patients with scrupulosity and different cultures.