1. Background
Misophonia is a condition in which the sympathetic nervous system responds to a particular auditory stimulus leading to negative emotions. Trigger stimuli in misophonia vary from person to person and usually involve a variety of mouth and nose sounds (such as chewing, crunching, slurping, sniffling, and snoring) and a wide range of other sounds (such as typing, ticking the clock, walking, and noises from the walls) (1).
People with misophonia have little tolerance for annoying noises (2, 3), and their reaction to stimuli is often in the form of disgust, anger, irritability, anxiety, and distress (4-6), and physical reactions occur in the form of rising body temperature, sweating, increased heart rate, respiration, and a feeling of tightness in the head and chest (7, 8). The most well-known coping strategy in these patients is avoiding. They actively avoid misophonia stimuli by anticipating unexpected encounters, planning to avoid triggers, and wearing headphones and earplugs (4, 5, 9). As a result of these avoidances, patients may limit their social relationships, reduce their working hours, or quit their jobs (10), which eventually significantly reduces the quality of life in these patients (4).
According to the scant literature, the prevalence of misophonia is estimated to be nearly 6 - 20% among university students (6, 11); however, misophonia has not been introduced in DSM yet. This can mainly be due to the constraints on relevant studies, most of which have been published since 2013.
Given the nature of misophonia, different therapeutic components such as cognitive reconstruction, relaxation, anger management training, exposure, and response prevention have been used as CBT to alleviate symptoms and improve misophonia. The results of CBT-based studies indicate the satisfactory outcomes of this therapy for their participants (10, 12-18). Nonetheless, some patients do not respond to CBT or are resistant to exposure, whereas many therapists do not feel comfortable in the implementation of exposure (19). Schneider and Arch extracted therapeutic components from acceptance and commitment therapy, and dialectical behavior therapy approaches to improve tolerance to distress in a wide range of emotions in misophonia by altering people's relationship to those emotions instead of focusing on mitigating symptoms. They suggested using cognitive defusion instead of focusing on triggers to reduce interest in avoidance among patients and help them live with values to boost their control over life. Moreover, other therapeutic components such as mindfulness and contradictory reaction can help accept difficult emotions experienced in misophonia. These therapeutic components were used in two case studies based on dialectical behavior therapy (DBT) (20) and mindfulness and acceptance component therapy (3). The results indicated improvement in the symptoms and severity of misophonia among the participants.
The literature mainly includes case studies, none of which compares the existing treatments. The availability of several therapeutic options can help therapists know further about the perception and treatment of misophonia. Moreover, analyzing the MACT functionality can broaden both the research areas and the existing behavioral approaches for studying and treating patients with misophonia.
This study was conducted in Iran due to the high prevalence of this disorder and the lack of a treatment method in the country. The study was carried out online due to the COVID-19 pandemic and extensive geography of Iran.
2. Objectives
The current study aimed to analyze and compare online group-mindfulness and acceptance‐based therapy and cognitive-behavioral therapy to determine the best treatment for misophonia.
3. Methods
3.1. Design, Setting, and Trial Registration
This study was a two-group random assignment pretest-posttest design, performed online and in groups for CBT and MACT. After distributing the announcement for the treatment courses via social media sites (Telegram and Instagram), the conditions of the courses were explained to the clients by phone, and the online Misophonia Questionnaire (MQ) was provided to them. Clients with a score of seven or higher on MQ were contacted, and arrangements were made for an individual in-person interview. The therapist conducted these intake sessions at the Tehran Institute of Psychiatry. During intake, the client provided informed consent to receive treatment. Finally, those eligible to participate in the treatment were randomly divided into two groups. All members were asked to answer questionnaires of distress tolerance, quality of life, and a scale evaluating depression, anxiety, and stress. Ten online treatment sessions were performed weekly for each treatment group using Skype. At the end of the course, the questionnaires completed before the treatment were re-provided to the clients online so that their responses could be measured after the treatment. Also, three months later, the questionnaires were completed to follow up the treatment.
The research project was approved by the Iran University of Medical Sciences (ethical code: IR.IUMS.REC.1398.702), and all the participants signed the consent form to participate in the research.
3.2. Inclusion/Exclusion Criteria
Inclusion criteria were an age of at least 18 years, attending ten therapy sessions at the specified time and online, and a score higher than seven on MQ. Individuals with severe suicidal ideation, psychotic disorder, bipolar disorder, substance use (based on the Structured Clinical Interview for DSM-5; SCID-5), and severe physical and organic brain diseases based on the patient's report and family reports were excluded from the study.
3.3. Therapists and Treatment Adherence
The two group sessions were led by a Ph.D. student in clinical psychology (first author) with five years of clinical experience under the weekly supervision of a CBT therapist with 15 years of experience. After obtaining the participants' consent, the therapy sessions were audio-recorded, and an independent assessor reviewed them randomly and assured treatment quality and adherence to the manuals.
3.4. Sample Size and Randomization
We calculated our sample size using G-Power software and by considering an effect size of 1.4 (based on and Zhou et al. (11)), α equal to 0.05, and power of 90%. The calculated final sample size was 16 patients per group, which was increased to 19 to accommodate the 20% of dropout rate. For randomization, the permuted block randomization was used with quadruple blocks. According to the sample size, ten quadruple blocks were generated using the website www.sealedenvelope.com.
3.5. Interventions
OG-MACT was adapted from a case study presented by Schneider and Arch (3). In this treatment, the conceptualization of sessions was done based on the ACT approach to change the client's view of thoughts and feelings, and then changing these perspectives was facilitated by introducing DBT components. In addition, since patients with misophonia have problems with attention flexibility, the therapeutic technique of attention training in the Wells metacognitive therapy approach (21), which includes three main components of selective attention, rapid change of attention, and divided attention, was added to this protocol by the study’s authors. At the same time, due to group meetings, all the exercises were reconstructed for group performance. The content of each session is summarized in Table 1.
| OG-CBT | OG-MACT | |
|---|---|---|
| 1 | Introducing group members; Psychoeducation about misophonia; Educating the OG-CBT model and cognitive distortions; Discussing group rules | Introducing group members; Psychoeducation on misophonia; Educating the OG-MACT model; Discussing group rules |
| 2 | Identifying negative thoughts, assumptions, and core beliefs; Identifying cognitive restructuring through cognitive techniques | Demonstrate the role of attention inflexibility in misophonia and educating attention training; Tracking trigger situations, related thoughts, and distress |
| 3 | Reviewing coping strategies; Training problem solving and effective communication | Introducing ACT values; Emphasizing the unworkability of control-oriented strategies |
| 4 | Demonstrating the role of relaxation; Guiding patients doing relaxation; Training stress management | Introducing cognitive defusion as a way of changing our relationship with thoughts |
| 5 | Introducing the rationale and goals for exposure and response prevention; Developing SUDS hierarchy and prepping for first exposure exercises | Introducing willingness; Educating the exercise of "Acceptance in real-time," helping to be willing and stay in contact with avoided events |
| 6 | Conducting exposures; Exposure was done first imaginatively, then as video watching, and finally as live | Conducting DBT-style chain analyses |
| 7 | Conducting exposures | Conducting DBT-style chain analyses; Demonstrating the role of relaxation; Training "opposite action," move of physically relaxing instead of tensing |
| 8 | Conducting exposures | Introduced the notion of mindfulness; Training acceptance-based mindfulness of anger and disgust exercise |
| 9 | Conducting exposures | Introduced the DBT component of; non-judgmental ness; Re-describing the situation objectively (just the facts) |
| 10 | Maintenance and relapse prevention | Maintenance and relapse prevention |
Abbreviations: OG-CBT, online group-cognitive Behavior therapy; OG-MACT, online group mindfulness‐ and acceptance‐based therapy; ACT, acceptance and commitment therapy; DBT, dialectical behavior therapy.
OG-CBT was adapted from Singer's (22) treatment protocol, and treatment components were adjusted and performed based on group sessions. During this treatment, the participants' cognitive distortions related to annoying noises were first examined, and cognitive challenges were addressed with their cognitive distortions. In the following sessions, problem-solving techniques, effective communication, stress management, and relaxation were taught. Finally, the technique of dealing with annoying noises was taught and performed. The content of each session is summarized in Table 1.
3.6. Measures
3.6.1. Demographic Characteristics Questionnaire
Researchers designed this questionnaire to assess participants' demographic characteristics such as age, gender, marital status, education, occupation, income, age at the beginning of treatment, similar problems in other family members, and previous treatments for misophonia.
3.6.2. Misophonia Questionnaire
Misophonia Questionnaire (MQ) (6) is an 18-item self-report questionnaire that uses multiple methods to assess misophonia symptoms, resulting in emotions and behaviors and the overall severity of sound sensitivities. A score greater than or equal to seven indicates 'moderate sound sensitivity,' which interferes with daily life and thus is treated as a cut-off for clinically significant symptoms. The reliability and validity of this interview have been confirmed in Iran by Mehrabizadeh Honarmand and Roushani (23). Internal consistency was acceptable in this study (α = 0.71).
3.6.3. Distress Tolerance Scale
Distress Tolerance Scale (DTS) (24) is a self-assessment index of a person's capacity to withstand negative emotional states. A study on Iranians (25) reported that the whole scale had high internal consistency reliability (25). Also, internal consistency in this study was good (α = 0.83).
3.6.4. Depression Anxiety Stress Scale-21
Depression Anxiety Stress Scale (DASS-21) (26) is a set of three self-assessment subscales designed to measure negative emotional states of depression, anxiety, and stress. The Persian version of this scale has been standardized on a sample of the general population, students, and patients with chronic pain (27). In this study, all the subscales had acceptable internal consistency, and the internal consistency of the total scale was good (α = 0.89).
3.6.5. World Health Organization Quality of Life Questionnaire
The World Health Organization Quality of Life Questionnaire (WHOQOL-BREF) was presented by the World Health Organization in 1996 and includes 26 items to measure four areas of physical health, psychological, social relationships, and environment (28). Iranian researchers have considered the internal consistency of the instrument to be acceptable (α = 0.77) (29). The internal consistency of this instrument was estimated to be excellent in the present study (α = 0.91).
3.7. Data Analysis
SPSS-22 software was used to analyze the data. Descriptive statistics, including frequency, mean and standard deviation, were calculated for demographic and clinical variables. Group homogeneity was compared in terms of demographic characteristics and initial clinical features through chi-square and t-test. The effects of independent variables (OG-CBT and OG-MACT) on dependent variables (misophonia, anxiety tolerance, quality of life and depression, anxiety, and stress) and therapeutic changes were evaluated pre-test and post-test and in the follow-up period in each of the experimental groups using repeated-measures analysis of variance. Jacobson and Truax's (30) method was used to calculate the clinical significance of the primary outcome variable (symptoms of misophonia). This was calculated using the pre-treatment standard deviation (7.4) and a test-retest reliability coefficient of 0.71, as reported in the validation study and according to the mean and standard deviation of the healthy group (M = 23.2, SD = 13.00) based on Mehrabizadeh Honarmand and Roushani (23).
4. Results
4.1. Baseline Characteristics
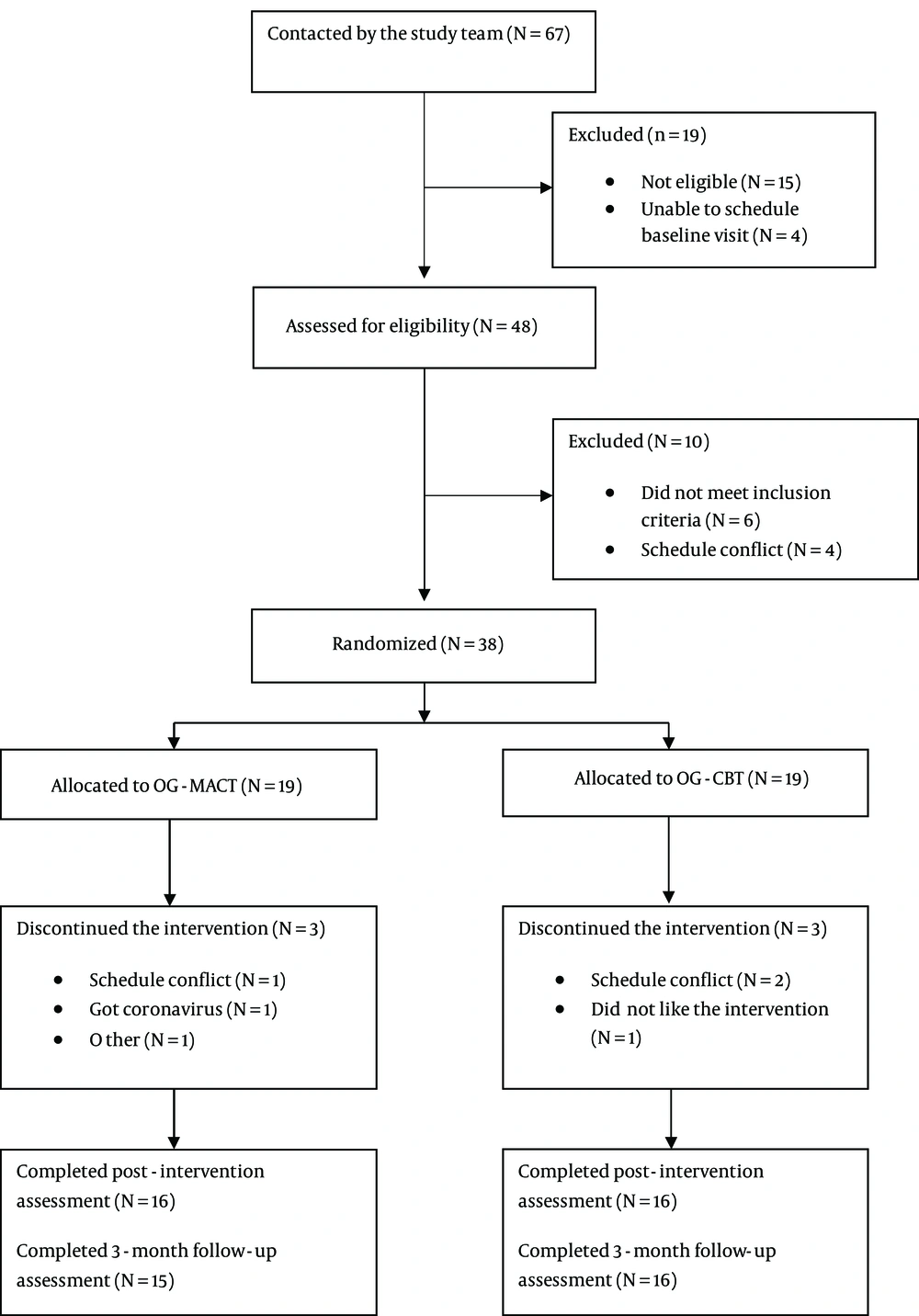
The basic characteristics of the study groups are reported in Table 2. There was no significant difference in chi-square statistics in the variables in the demographic characteristics questionnaire between the two groups. The overall sample consisted of 28 women (90.3%) and three men (9.7%) between 20 and 46 years of age (mean = 30.32; SD = 7.04), over half of whom were single (58.06%, n = 18). A high percentage of the sample were university students or people who had already completed their university education (87. 1%, n = 27). More than half of them had misophonia in their family members (58.06%, n = 18). The eating sound was the most frequently reported annoying sound. Obsessive-compulsive personality disorder (58.06%, n = 18) and anxiety disorders (45.16%, n = 14) had the most comorbidity with misophonia. In total, 15 of the 19 OG-MACT participants (80%) and 16 of 19 OG-CBT participants (84%) completed the courses. Figure 1 describes the flow of the participants during the trial.
| Variables | OG-CBT (N = 16) | OG-MACT (N = 15) | Total (N = 31) | χ2 or t | P-Value |
|---|---|---|---|---|---|
| Age (y) | 29.43 ± 5.52 | 31.26 ± 8.47 | 30.32 ± 7.04 | 0.71 | 0.47 |
| Age of onset | 1.19 | 0.75 | |||
| Childhood | 5 (16.12) | 5 (16.12) | 10 (32.25) | ||
| Teenager | 6 (19.35) | 6 (19.35) | 12 (38.7) | ||
| Adult | 5 (16.12) | 4 (12.90) | 9 (29.03) | ||
| Gender | |||||
| Female | 15 (48.38) | 13 (41.93) | 28 (90.3) | 0.44 | 0.50 |
| Male | 1 (3.22) | 2 (6.45) | 3 (9.7) | ||
| Education | |||||
| Diploma | 1 (3.22) | 3 (9.67) | 4 (12.9) | 2.61 | 0.45 |
| Bachelor | 10 (32.25) | 7 (22.58) | 17 (54.83) | ||
| Master | 5 (16.12) | 4 (12.90) | 9 (29.03) | ||
| Doctoral | 0 | 1 (3.22) | 1 (3.22) | ||
| Marital status | |||||
| Married | 7 (22.58) | 5 (16.12) | 12 (38.7) | 1.30 | 0.52 |
| Single | 9 (29.03) | 9 (29.03) | 18 (58.06) | ||
| Divorced | 0 | 1 (3.22) | 1 (3.22) | ||
| Misophonia in other family members | |||||
| Yes | 8 (25.80) | 10 (32.25) | 18 (58.06) | 0.88 | 0.34 |
| No | 8 (25.80) | 5 (16.12) | 13 (41.93) | ||
| Comorbid disorder | |||||
| Anxiety disorders | 9 (29.03) | 5 (16.12) | 14 (45.16) | 2.63 | 0.10 |
| Depression/depressive disorders | 3 (9.67) | 5 (16.12) | 8 (25.80) | 0.27 | 0.59 |
| ADD/ADHD | 2 (6.45) | 2 (6.45) | 4 (12.90) | 0.005 | 0.94 |
| OCD | 1 (3.22) | 1 (3.22) | 2 (6.45) | 0.002 | 0.96 |
| OCPD | 7 (22.58) | 11 (35.48) | 18 (58.06) | 2.78 | 0.09 |
Abbreviations: OG-CBT, online group-cognitive behavior therapy; OG-MACT, online group-mindfulness‐and acceptance‐based therapy; ADD/ADHD, attention deficit disorder/attention deficit hyperactivity disorder; OCD, obsessive-compulsive disorder; OCPD, obsessive-compulsive personality disorder.
a Values are expressed as mean ± SD or No. (%).
The chi-square statistics for age, education, and marriage variables were more significant than 0.05 in comparing the three groups. Therefore, the three groups did not significantly differ in terms of age, education, and marriage.
4.2. Treatment Effectiveness
Table 3 shows the results of the repeated measures analysis of variance of the two experimental groups in the pre-test, post-test, and three-month follow-up phases in self-report questionnaires. The effects of time and group interaction were significant in none of the scales. In other words, the difference between the mean scores of the scales at different times did not differ according to the type of treatment group (OG-CBT versus OG-MACT).
| T0: Pre-Treatment | T1: Post-Treatment | T2: 3-Month Follow-up | Time | Time × Group Interaction | Partial Eta Squared | Observed Power | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OG-CBT | OG-MACT | OG-CBT | OG-MACT | OG-CBT | OG-MACT | F | P | F | P | |||
| MQ | 40.3 ± 7.1 | 42 ± 7.4 | 28.8 ± 11.5 | 29.5 ± 14.1 | 24.8 ± 7.8 | 28.2 ± 12.2 | 40.03 | < 001 | 0.31 | 0.66 | 0.01 | 0.09 |
| DTS | 40.4 ± 9.7 | 39 ± 9.4 | 47.7 ± 9 | 45.7 ± 8.3 | 46.6 ± 11.3 | 48.9 ± 10.2 | 15.23 | < 001 | 1.09 | 0.33 | 0.03 | 0.22 |
| WHOQOL-BREF | 78.9 ± 13.3 | 83.6 ± 15.3 | 80.7 ± 11.8 | 86.3 ± 14.4 | 81.2 ± 13.6 | 85.3 ± 10.4 | 1.07 | 0.34 | 0.09 | 0.88 | 0.003 | 0.06 |
| Physical health | 52.4 ± 17.5 | 63 ± 18.8 | 56.6 ± 13.1 | 65.7 ± 18.2 | 57.3 ± 16.5 | 645 ± 13.5 | 1.18 | 0.30 | 0.24 | 0.71 | 0.008 | 0.08 |
| Social relationships | 39.5 ± 22.6 | 52.7 ± 21 | 43.7 ± 16.2 | 51.6 ± 20.2 | 45.8 ± 16.9 | 52.7 ± 15.6 | 0.72 | 0.48 | 0.83 | 0.43 | 0.02 | 0.18 |
| Environment | 55.6 ± 15 | 54.3 ± 17.2 | 53.3 ± 15.8 | 55 ± 16.3 | 52.9 ± 13.5 | 52 ± 14.4 | 0.71 | 0.44 | 0.28 | 0.67 | 0.01 | 0.38 |
| Psychological | 47.6 ± 16.8 | 48 ± 17.9 | 51 ± 12.3 | 55.2 ± 17.2 | 51 ± 15.3 | 56.6 ± 14.3 | 4.1 | 0.02 | 0.71 | 0.49 | 0.02 | 0.16 |
| DASS-21 | ||||||||||||
| Anxiety | 6.4 ± 3.9 | 4.8 ± 4.16 | 5.4 ± 3.5 | 3.7 ± 4 | 4.3 ± 4.6 | 2.3 ± 2.4 | 7.33 | 0.001 | 0.06 | 0.93 | 0.002 | 0.06 |
| Depression | 7.1 ± 5.5 | 6.3 ± 4 | 5.7 ± 4.8 | 5.6 ± 4.1 | 5.4 ± 4.6 | 4.8 ± 2.4 | 3.42 | 0.03 | 0.14 | 0.86 | 0.005 | 0.07 |
| Stress | 11.3 ± 4.4 | 12.3 ± 3.2 | 10 ± 4.6 | 10 ± 2.8 | 8.6 ± 4.5 | 9.8 ± 2.9 | 10.81 | < 001 | 0.69 | 0.50 | 0.02 | 0.16 |
Abbreviations: OG-CBT, online group-cognitive behavior therapy; OG-MACT, online group-mindfulness‐and acceptance‐based therapy; MQ, misophonia scale; DTS, distress tolerance scale; WHOQOL-BREF, world health organization quality of life questionnaire; DASS-21, depression anxiety stress scale.
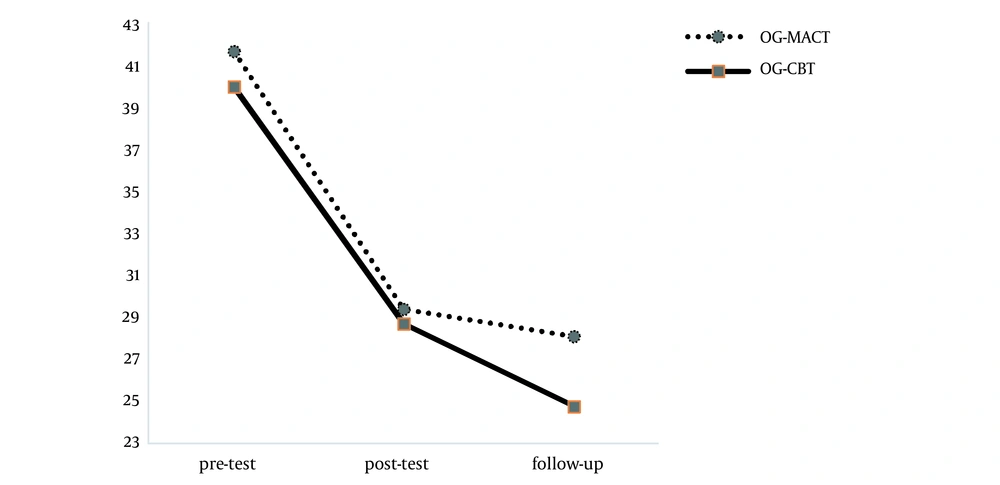
The results of Table 3 show that the effect of time on misophonia scores is significant (F = 40.03, P < 001). Regardless of the studied groups, there was a significant difference between the mean scores of misophonia in the pre-test, post-test, and follow-up phases (Figure 2). This finding also applies to the distress tolerance questionnaire (F = 15.23, P < 001). Data analysis for the DASS questionnaire also showed the significance of the subscales of depression (F = 3.42, P = 0.03), anxiety (F = 7.33, P = 001), and stress (F = 10.81, P < 001) over time. However, there was no significant difference in the quality of life over time (F = 1.07, P = 0.34). After examining the subscales, it was found that except for the subscales of mental health (F = 4.1, P = 0.02), other subscales, including environmental health (F = 0.71, P = 0.44), physical health (F = 1.18, P = 0.3), and quality of social relationships (F = 0.72, P = 0.48) were not significant.
4.3. Clinically Meaningful Improvement
The stable change index, considering Cronbach's alpha 0.71, was calculated. Based on this index, the changes of nine members of the OG-MACT group with a range of -0.54 to 5.39 and 11 members of the OG-CBT group with a range of -0.18 to 4.85 were stable. According to the study of Mehrabizadeh Honarmand and Roushani (23), the cut-off point of the tool was calculated to be 35.9. Based on this cut-off point, the changes of eight members of OG-MACT (53%) and 11 members of OG-CBT (69%) were clinically significant.
5. Discussion
The findings of this study showed that there was no statistically significant difference in the score of misophonia in general and its subscales between the two treatment groups. However, the effect of treatment over time (pre-test, post-test, and follow-up) was significant in both groups, and the clinical significance of treatment was 69% in OG-CBT and 53% in OG-MACT, showing, according to group members, that the maximum attendance at meetings and exercises was directly related to the effectiveness of treatment. Findings based on the effectiveness of OG-CBT are consistent with that of Schroder et al. (12) study in which 90 patients with misophonia were treated as a group using the CBT approach; although in the present study, the clinical significance of OG-CBT was greater than Schroder et al. (12) study (68% vs. 48%), the treatment process might influence this outcome. In a randomized controlled trial, Jager et al. (16) compared CBT treatment with the control group and found that CBT treatment was significant compared to the control group. Other studies that have examined CBT in the treatment of misophonia have been case studies, and all of them have confirmed the effectiveness of this treatment (10, 12-15), in line with the present study. In the case of OG-MACT, only one case study was conducted in line with the present study, which confirmed the effectiveness of both treatments (3).
As mentioned earlier, patients with misophonia experience higher anxiety than normal individuals (6, 11, 31, 32). In this study, anxiety levels were assessed over time, and the results showed that in addition to the reduction of misophonia, the patients' anxiety also decreased significantly. This finding is consistent with the findings of Muller et al. (15), and Singer (22) studies, who found that the treatment of misophonia effectively reduced anxiety symptoms of patients with misophonia. In this study, other variables such as distress tolerance that decreases in misophonia according to the research literature (2) were evaluated, and the results showed a decrease in anxiety tolerance after misophonia treatment. This finding has not been evaluated as evidence-based in other studies, although Schneider and Arch (3) used techniques to increase the patient's anxiety tolerance and stated that the client's distress tolerance increased after treatment.
In explaining the findings, it seems that the study of treatment approaches of each group can be helpful. MACT online group therapy, to increase the therapeutic effect of various therapeutic components, uses the ACT (acceptance, mindfulness, cognitive defusion, and values) and DBT (acceptance, mindfulness, opposite action, and behavior chain analysis) approaches. On the other hand, CBT group therapy uses cognitive reconstruction techniques and behavioral skills training such as problem-solving, assertive behavior training, and exposure and response prevention. These techniques target different aspects of misophonia symptoms. Considering the different aspects of treatment, the focus of both treatments is on cognitions and avoidance behaviors. Both of them accept the role of cognition in the occurrence of the problem, but the extent to which each method emphasizes that they play roles in the theoretical analysis is various (33). Based on the present study, it seems that different methods of both treatments can ultimately have the same results for patients with misophonia.
Research literature indicates that in addition to reducing the symptoms of misophonia, depression also improves (22), but treatment does not constantly improve the quality of life (16). The present study failed to significantly increase the quality of life, which seems to be influenced by environmental factors. The present study was conducted during the COVID-19 pandemic when there were restrictions on movement and communication between individuals and access to recreational facilities was limited. Fear of being infected with COVID-19 can cause additional stress for everyone, including participants in the present study, and all of these stressors could directly affect the individuals' quality of life (34). However, after examining the subscales of quality of life, the subscale of mental quality significantly improved. However, there was no significant change in the other subscales (environmental health, physical health, and quality of social relationships), which seems to be due to a decrease in the quality of life environment.
5.1. Limitations and Future Studies
The present study results should be considered according to the following limitations: First, the participants' double stress due to coronavirus infection was a factor in the participants' dropouts, and the uncertain effect of treatment on variables such as stress and quality of life. Second, we did not include a control group. Third, the sample size was small, limiting the generalizability of the findings. For future studies, it would be recommendable to have at least a waitlist control group in randomized controlled trial designs, including a more extensive and diverse sample, for more definite conclusions on efficacy and to improve the generalizability of the findings. Using a multiphase optimization strategy (MOST) design will also be beneficial, particularly to examine specific components of OG-CBT and OG-MACT.
5.2. Conclusions
The results of this study showed that the two online group therapies of CBT and MACT effectively reduced misophonia symptoms and improved the participants' anxiety, stress, depression, and distress tolerance.