1. Background
The Coronavirus disease 2019 (COVID-19) outbreak is one of the biggest global health threats (1), wherein healthcare workers (HCWs) play a leading role in dealing with this condition. In this sense, prehospital emergency medical services (EMS) practitioners are at the forefront in providing care for COVID-19 patients (2). As reported by the National Health Commission of China, 3300 HCWs have been infected since early March, and at least 22 cases have died from this pandemic, according to public media. In Italy, 20% of HCWs have also been infected, and some have even lost their lives (3). In Wu and McGoogan’s study, the prevalence rate in HCWs was reported to be 3.8% during the pandemic (4). In a study by Katayama et al. evaluating the effects of COVID-19 on the EMS system in Japan within January 1 and April 14, 2020, 36981 patients were admitted to hospitals with the diagnosis of acute illness. The difficulty in admitting critically ill patients at the time of the COVID-19 pandemic was also multiplied compared to that in the last year (5).
In a survey on Iranian pre hospital EMS professionals’ response to COVID-19, the findings revealed that the number of EMS calls and ambulance dispatches in Tehran augmented by 347% and 20%, respectively. Despite the compounded workload, the average response time by the EMS stations declined. Call center average wait time was also minimized from 12.7 ± 10.6 to 11.8 ± 9.8 seconds during the COVID-19 outbreak. The prehospital EMS system accordingly neutralized the rising workload due to the COVID-19 pandemic by adding to the working hours and improving the resources and equipment in dispatch centers (6). Given the increased workload among EMS practitioners, their vulnerability multiplied. Previous research during former pandemics (7) also denoted vulnerability to mental disorders among HCWs in response to COVID-19.
Among the significant factors affecting the decline in EMS practitioners’ mental health during the COVID-19 pandemic are a sharp increase in the number of cases infected, disruption to the supply of personal protective equipment (PPE), medication shortages, concerns for infecting family members, and witnessing patient death (8). The results of one study on psychological consequences among Chinese HCWs correspondingly demonstrated that the incidence rate of anxiety disorder was 44.6%, and such values were reported as 34% and 71.5% for insomnia and distress, respectively (9). Fear of COVID-19 has also been more common among the family members of HCWs than in the rest of society. In a survey of volunteer students in China, most respondents reported intense fear of the possible infection of their family members (10). Therefore, interrupted contact with family members was introduced among the factors affecting the mental health of HCWs (11).
In recent years, positivism has been to identify ways to better adapt to life-changing situations and threats. In this sense, resilience has also been one of the most fundamental constructs associated with individuals’ adaptation to society (12) since it helps cope with difficult situations and provides protection against mental disorders (13). By definition, resilience means the assurance of individual abilities to deal with stress and adopt coping mechanisms via emotional stability (12). Therefore, during the COVID-19 pandemic, resilience has been one of the facilitators promoting mental health status. In a study by Eyni et al., modeling COVID-19 anxiety in students based on resilience, the findings revealed that resilience led to a reduction in their levels of anxiety (14). In a qualitative study of psychological distress among Iranian HCWs during COVID-19, the most important sources of distress were introduced as fear of being at work, fear of death, uncomfortable feelings of using PPE, increased workload, equipment shortages, pay injustices, sleep disturbances, stigmatization, and public disregard to quarantine rules. Individual support sources were also delineated as a high level of adaptability, realism, high self-confidence, challenging interests, sense of humor, hope, courage, strong thinking skills, adherence to ethics and spirituality, and inner calm and flexibility (15).
2. Objectives
Resilience also eases the psychological consequences of the COVID-19 pandemic. As prehospital EMS practitioners are at the forefront in terms of communicating with patients with COVID-19, due to the shortage of human resources and the need to improve the mental health of EMS staff, the present study was conducted to investigate the mental health and its relationship with resilience in prehospital EMS staff to improve their resilience and mental health in Iran.
3. Methods
This descriptive/analytical cross-sectional study was conducted in 2020 on the statistical population of EMS practitioners working in 115 EMS stations in Golestan province, northern Iran, who were also involved in providing care for COVID-19 patients. For sample size determination, the following formula was applied in which α refers to type-I error probability, β represents type-II error probability, and r shows the default correlation coefficient:
Considering α = 0.05 (z = 1.96), β = 0.1 (z = 1.28), and r = 0.3 (i.e., the correlation between mental health and resilience), 113 samples were estimated for the present study. Therefore, the data were collected through a web-based questionnaire (docs.google.com/forms/d/e/1FAIpQLSd7_3Cz7imw4-HAabNwJeP1aZWP5wpsENWXgHiFaQOpaxKrA/viewform).
This study investigated the mental health and resilience of 115 prehospital EMS practitioners in Golestan province, selected by the convenience sampling method using towquestionnaire. The questionnaires was comprised of the General Health Questionnaire-28 (GHQ-28) and the Connor-Davidson Resilience Scale (CD-RISC).
The GHQ-28, developed by Goldberg and Heller (1979), was used to evaluate patients’ morbidity symptoms and various health conditions from a month before the study (16). The factor analysis of this questionnaire also revealed four subscales, each one consisting of seven items, including somatic symptoms, anxiety and insomnia, social dysfunction, and severe depression. The items were also arranged sequentially, namely items no. 1 - 7 for somatic symptoms and items no. 8 - 14 related to anxiety and insomnia. Moreover, items no. 15 - 21 were dedicated to social dysfunction, and items no. 22 - 28 were associated with severe depression. Responses in this questionnaire were scored based on a 4-point Likert-type scale (from 0 to 3), ranging from 0 to 84. Obtaining a high score on this scale indicated more morbidity symptoms; in other words, lower mental health, and conversely, a low score suggested the fewest morbidity symptoms and higher mental health status. The highest score was considered 84, and the cut-off point of 23 could be utilized to identify the cases facing problems. The validity and factor structure of the GHQ-28 translated into Persian by Nazifi et al. was also confirmed in the healthcare centers of Kerman University of Medical Sciences, Kerman, Iran. Moreover, the 28-item GHQ-28 had good reliability and validity (17). In the present study, Cronbach’s alpha coefficient was 0.88.
The CD-RISC consisted of 25 items. The psychometric properties of this scale were determined in six groups, including general and clinical populations, especially individuals from a typical American community, primary care outpatients, general psychiatric outpatients, individuals with generalized anxiety disorders, individuals with posttraumatic stress disorder (PTSD), and two groups of patients with PTSD. The questionnaire scoring was also based on a 5-point Likert-type scale (from not at all true to true nearly all the time). The scores ranged from 0 to 100, and the overall resilience score was classified into four levels, including 0 - 25, 26 - 50, 51 - 75, and 76 - 100 (18). Higher scores accordingly indicated more resilience in respondents. Moreover, the CD-RISC had five subscales, namely personal competence and tenacity (items no. 10, 11, 12, 16, 17, 23, 24, and 25), trust in one's instincts, and strengthening effect of stress (items no. 6, 7, 14, 15, 18, 19, and 20), accepting change positively (items no. 1, 2, 4, 5, and 8), control (items no. 13, 21, and 22), and spiritual influences (item no. 9). Connor and Davidson also reported the Cronbach’s alpha coefficient of this scale as 0.89. In addition, the reliability coefficient obtained from the test-retest method for the CD-RISC in a 4-week interval was 0.87. This scale was standardized in Iran by Mohammadi. For the determination of the reliability of the CD-RISC, Cronbach’s alpha was applied, and a reliability coefficient of 0.89 was reported (19). The validation of this questionnaire in Iran was accomplished in different groups (20-24). In the present study, Cronbach’s alpha coefficient was 0.92.
The inclusion criteria in this study were working in one of the 115 EMS stations in Golestan province and providing care for patients with COVID-19. The exclusion criterion was returning incomplete questionnaires up to 20% of the items, although all individuals in this study answered the items completely.
This study also observed the principles of research ethics, including maintaining the confidentiality of information, obtaining informed consent, and giving the right to withdraw from the study. In addition, this research project with the ethics code of IR.MAZUMS.REC.1399.543 was approved by Mazandaran University of Medical Sciences, Sari, Iran.
3.1. Statistical Analysis
Descriptive statistics were reported in this study using the frequency, percentage, mean, and standard deviation indices. The hypothesis of the normality of the scores of the questionnaires was measured using the Kolmogorov-Smirnov test. The relationship between both questionnaires was examined by structural equation modeling (SEM) using maximum likelihood estimation. In addition, multiple linear regression (MLR) was applied to reflect on the factors affecting the resilience mean score. With the consideration of a significance level of 0.05, the data analysis was performed using IBM SPSS Statistics software (version 22) and IBM SPSS Amos software (version 24.0).
4. Results
A total of 115 EMS practitioners were included in this study, 99.1% and 85.2% of whom were male and married, respectively. The mean age of the subjects was 32.63 ± 7.56 years. Most practitioners also held a bachelor’s degree (47.8%). Regarding the type of employment, most EMS practitioners worked in a compulsory medical service program (31.3%). In addition, the average work experience was 8.82 ± 6.85 years. Table 1 shows the descriptive information of EMS practitioners in this study.
| Factors | No. (%) |
|---|---|
| Gender | |
| Male | 114 (99.1) |
| Female | 1 (0.9) |
| Marital status | |
| Single | 17 (14.8) |
| Married | 98 (85.2) |
| Education level | |
| Associate’s degree | 51 (44.3) |
| Bachelor’s degree | 55 (47.8) |
| Higher | 9 (7.9) |
| Type of employment | |
| Permanent | 34 (29.6) |
| Temporary-to-permanent | 20 (17.4) |
| Contractual | 19 (16.5) |
| Compulsory program | 36 (31.3) |
| Corporate | 6 (5.2) |
The GHQ-28 mean score was 25.73 ± 8.90. Table 2 shows the mean scores of the GHQ-28 subscales. With reference to the cut-off points, 49.6% and 43.5% of the EMS practitioners were in mild and good mental health conditions, respectively. The rest were identified with moderate mental health. Considering the GHQ-28 subscales, 60.9% and 38% of the EMS practitioners had good and mild mental health conditions, respectively. The rest had moderate mental health status. Based on the subscale of somatic symptoms, 86.1% and 4.3% of the respondents were in good and mild mental health conditions, respectively. The rest were characterized by moderate mental health status. With regard to the social dysfunction subscale, 55.7% and 40.0% of the practitioners were in good and mild mental health conditions, respectively. The rest were in moderate mental health status. Based on the severe depression subscale, 89.6% and 9.6% of the EMS practitioners were in good and mild mental health conditions, respectively. The rest were in moderate mental health status. In addition, the mean score of the CD-RISC was 72.25 ± 12.63, and the values of other subscales are reported in Table 2.
| Factors | Mean ± SD | Regression Coefficient (b) | Standard Error | Standardized Regression Coefficient (β) | Critical Ratio Z = b/SE | P-Value |
|---|---|---|---|---|---|---|
| Mental health → Somatic symptoms | 6.09 ± 3.35 | 1.00 | 0.80 | |||
| Mental health → Anxiety and insomnia | 5.47 ± 4.17 | 0.88 | 0.16 | 0.64 | 5.71 | < 0.001 |
| Mental health → Social dysfunction | 12.04 ± 2.43 | - | ||||
| Mental health → Severe depression | 2.13 ± 2.90 | 1.02 | 0.17 | 0.71 | 6.03 | < 0.001 |
| Resilience → Personal competence and tenacity | 23.50 ± 4.54 | 0.65 | 0.11 | 0.59 | 5.86 | < 0.001 |
| Resilience → Trust in one’s instincts and strengthening effect of stress | 18.42 ± 3.90 | 0.81 | 0.17 | 0.48 | 4.67 | < 0.001 |
| Resilience → Accepting change positively | 15.12 ± 2.82 | 0.52 | 0.14 | 0.37 | 3.65 | < 0.001 |
| Resilience → Control | 8.74 ± 2.10 | 8.56 | 0.12 | 0.79 | 7.38 | < 0.001 |
| Resilience → Spiritual influence | 6.47 ± 1.47 | 1.00 | 0.80 | < 0.001 |
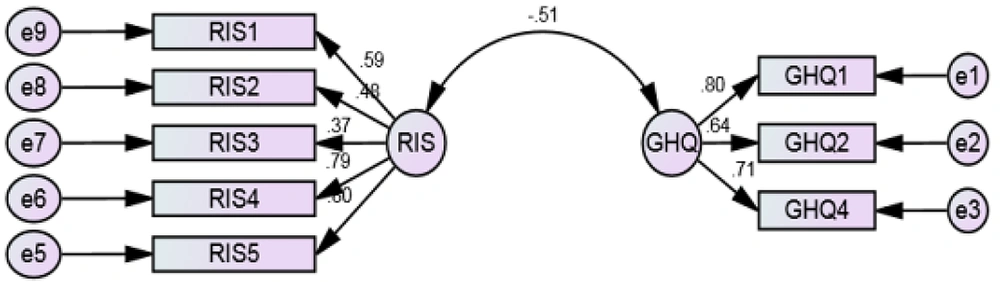
The measurement model in this study using SEM is illustrated in Figure 1. This model was obtained after some corrections (i.e., upon removing the social dysfunction subscale in the GHQ-28 due to having a regression coefficient less than 0.3). The results of the goodness-of-fit indices of the above-mentioned model are reported in Table 3. The reported indices of the root mean square error of approximation (≤ 0.08), comparative fit index (≥ 0.9), parsimonious comparative fit index (≥ 0.6), goodness-of-fit index (≥ 0.9), Chi-square divided by the degrees of freedom (≤ 3), and P-value ( > 0.05) have acceptable values, indicating that the model has a good fit (25).
| Root Mean Square Error of Approximation | Parsimonious Comparative Fit Index | Comparative Fit Index | Goodness-of-Fit Index | Chi-Square Divided by the Degrees of Freedom | Degrees of Freedom | P-Value |
|---|---|---|---|---|---|---|
| 0.08 | 0.66 | 0.97 | 0.95 | 1.82 | 19 | 0.265 |
Table 2 lists the regression coefficients between the research factors. The results revealed that all regression coefficients between the subscales of the questionnaires and their factors were significant. Standardized coefficients were also used to compare the subscales and determine the one more effective in mental health or resilience. In the GHQ-28 and CD-RISC, somatic symptoms and spiritual influence were the most important subscales, respectively.
In addition, the covariance and correlation coefficient between the two questionnaires were -0.15 and -0.51, respectively, which were significant (P = 0.001). These results also indicated that mental health deterioration (higher scores) diminished resilience in the EMS practitioners.
In Table 4, the factors affecting the resilience mean score were determined using MLR (R2 = 0.54). Accordingly, the type of employment and resilience mean score had a significant effect on the resilience mean score of EMS practitioners of 115 EMS stations in Golestan province. On average, the resilience mean score of the practitioners with the corporate type of employment was approximately 13.35 points higher than permanent employment. Accordingly, the resilience mean score dropped by an average of 0.77 as the mental health mean score elevated. Other variables did not show a significant effect on the resilience mean score.
| Factors | Regression Coefficient | Standard Error | P-Value |
|---|---|---|---|
| Gender | |||
| Male | Reference | ||
| Female | 15.11 | 10.86 | 0.167 |
| Age | 0.08 | 0.27 | 0.766 |
| Marital status | |||
| Single | Reference | ||
| Married | 4.67 | 3.08 | 0.133 |
| Education level | |||
| Associate’s degree | Reference | ||
| Bachelor’s degree | 1.14 | 2.38 | 0.634 |
| Higher | 2.17 | 4.95 | 0.662 |
| Work experience | 0.11 | 0.35 | 0.757 |
| Type of employment | |||
| Permanent | Reference | ||
| Temporary-to-permanent | 6.27 | 3.52 | 0.078 |
| Contractual | 2.69 | 3.46 | 0.438 |
| Compulsory program | 6.98 | 4.24 | 0.103 |
| Corporate | 13.35 | 5.29 | 0.013 |
| Mental health status | -0.77 | 0.12 | 0.001 |
5. Discussion
This study aimed to investigate the relationship between mental health and resilience among prehospital EMS practitioners in Golestan province, northern Iran. In this regard, more than half of these individuals were in moderate mental health conditions. In the present study, all the prehospital EMS professionals involved in the operating sector were male. In Maiorano et al.’s study, examining mental health risk factors in HCWs in Italy, female subjects were observed to be more vulnerable than male subjects to the psychological consequences of COVID-19 (26), which could not be compared to the findings of the present study because there were no female participants.
In Saffari et al.’s study, evaluating the psychological consequences of COVID-19 in the general population and HCWs revealed that anxiety and depression mean scores in HCWs were higher than in the general population (P < 0.001); nevertheless, there was no significant difference in the levels of stress between both groups (27). A review study by Bahar et al. demonstrated that mental health could be related to the levels of resilience in HCWs (28). In the present study, the resilience mean score also decreased by an average of 0.77 following the increase in mental health mean scores. The results of other investigations also showed that individuals with high levels of resilience could suffer less from mental disorders (29, 30). Roman-Mata et al. similarly reported that the professionals working in EMS stations during the COVID-19 pandemic showed more resilience and flexibility (31).
In addition, Arianpour and Amirimanesh demonstrated that the resilience mean scores of the nurses working in COVD-19 wards were significantly lower than those involved in nonCOVID-19 wards (32). The HCWs directly contributing to the diagnosis, treatment, and care of COVID-19 patients due to the growing number of confirmed and suspected cases, increased workload, disruption to the supply of PPE, medication shortages, and no support were also more prone to mental health problems and other symptoms (9).
In a survey by Mousavi et al., reflecting on resilience and self-morbidity caused by COVID-19, the resilience mean score was 78.56 ± 20.95 (33); however, this value among the EMS practitioners in the present study was 72.25 ± 12.63. With reference to Ang et al.’s study, a significant positive relationship was observed between the educational level of Singaporean nurses and resilience (34), which is not consistent with the findings of the present study. The discrepancy in the results of both studies was attributed to the heterogeneity of the statistical populations and the absence of COVID-19 at the time of the study by Ang et al. A 2020 study carried out by Zhang et al. in China on HCWs involved in providing care for COVID-19 patients also demonstrated that the symptoms of mental health disorders were very high and serious (10). Overall, 50.4% of the total participants reported the symptoms of depression. Moreover, 44.6%, 34%, and 71.5% of them expressed levels of anxiety, insomnia, and mental distress, respectively. In addition, a review of the results in this study showed that professionals who were in direct contact with COVID-19 patients obtained a higher anxiety index than those who were not. The anxiety index in HCWs in the affected cities (e.g., Wuhan) was also higher than in other regions (35). A cross-sectional study on HCWs in China during the COVID-19 outbreak in 2021 demonstrated that the prevalence rate of anxiety was about 12.5% (36).
In Sirati Nir et al.’s study, the level of stress in clinical HCWs exposed to COVID-19 was also higher than in nonclinical practitioners. Furthermore, 90.2% of the individuals reported moderate levels of stress (37). In the present study, in terms of anxiety and insomnia, 86.1% and 4.3% of the EMS practitioners were at good and mild levels, respectively. The rest were at a moderate level. Based on the social dysfunction subscale, 15.7% and 5.2% of the respondents were in good and poor conditions, respectively. The rest were in moderate condition. Based on the severe depression subscale, 86.1% and 4.3% of the cases were at good and poor levels, respectively. The rest were at a moderate level. The discrepancy in the results could be associated with the study samples, the duration of the study, and the levels of expectations in HCWs. According to Jahanshahi et al.’s study, the level of psychological distress in the Iranian society in the face of COVID-19 was also higher than in the Chinese society (38).
Of note, the implementation of measures, such as accurate updating of health information records, particularly regarding the number of recovered cases, was associated with the low levels of stress during the COVID-19 pandemic in the Chinese society. Additional information on medications or vaccines, modes of transmission, and updates on the number of infected cases and their locations could also be related to lower levels of anxiety (39). Therefore, based on the results of the reviewed studies, regular care and maintenance of mental health in HCWs while coping with infectious patients and COVID-19 is of utmost importance. As HCWs are at the forefront of dealing with this crisis, they bear huge physical-psychological burdens, requiring more attention and preparation by health system officials.
Positive strategies to cope with stress were also observed to be effective in reducing stress in HCWs. Accordingly, Cai et al., in their study on the COVID-19 crisis in China, reported that the most important factor in relieving stress in HCWs was the positive attitude of their colleagues (40). The need for organizational and social attention and support for first-line HCWs should not also be ignored. Additionally, significant evidence supports the effectiveness of coping, resilience, and social support behaviors in maintaining mental health among HCWs during the COVID-19 pandemic (41). Therefore, HCWs with higher organizational and social support experience less anxiety in relation to COVID-19 (42, 43).
5.1. Conclusions
The present study provided strong evidence for prehospital medical care systems, particularly EMS managers, to assist practitioners during the COVID-19 pandemic. As EMS practitioners are at the forefront of providing care for COVID-19 patients, there is a need to boost their mental health status and levels of resilience by comprehensive planning.