1. Background
The global population is moving toward old age, which is followed by certain challenges and opportunities for all people. Despite living longer, people do not live a healthy life today, and about three-quarters (23%) of the total number of global mortalities occur among people at or above 60 years of age. The most common reason has been chronic and long-term diseases (1). An increase in age and entrance into old age can be followed by a higher chance of affliction with one or more chronic diseases, and most old adults suffer from at least one chronic disease (2). These chronic diseases, which their threat is higher for old adults, include muscular/skeletal and genetic disorders along with cancers, mental disorders, chronic respiratory problems, heart diseases, stroke, and nervous system diseases (3). Chronic nervous system diseases afflict 5 - 55% of those older than 55 years of age (4, 5) and are followed by a high risk of health issues, mortalities, disabilities, falling down, and hospitalization (6). As these diseases are chronic and long-term in nature, higher age is associated with higher risks of the disease and the co-occurrence of other age-related disorders (7). Hence, old adults’ dependence grows while their autonomy gets seriously limited. They become dependent on almost all daily activities (e.g., going to the restroom, taking a bath, dressing up, eating, and walking) and instrumental activities (e.g., managing earnings, using a phone, preparing food, and taking medicine) for which they need assistance (8-13). Besides the chronic nature of diseases that often afflict old adults during emergencies, particularly virus pandemics, old adults with chronic diseases are more vulnerable (14), and because there is no definite cure or vaccine for the coronavirus, and it is easily transmitted from one person to another, they are encouraged to stay home to prevent the rapid spread of the disease (15). Also, in most cases, when a chronic disease occurs, a family member takes care of the old adult patient (16-20); and is responsible for the caregiving and decision-making for the old adult patient (21). A further spread of the disease faces the caregivers with many changes in their role and makes them spend more time supporting the patient (22). That makes caregivers’ life limited to the act of taking care of the family (23), so they forget all about their own leisure and social relations. As a result, their quality of life and general health are adversely affected (24). Caregivers are at the risk of negative physical, psychological, and social effects, such as low immunity, sleep disorder, miscommunication with the patient or other family members, and caregiving burden (25). They also experience a higher level of anxiety, depression, and stress (26). Due to the undervaluation of their health, they experience less immunity, leading to more health threats (27). As for the quarantine during the coronavirus pandemic, about half of the caregivers reported that the pandemic and the concomitant quarantine reduced the time spent on personal affairs by 30.3%. They also reported increased psychological conflicts in families (by 15.5%) and changed lifestyles. Caregivers also reported an increased level of anxiety (45.9%), depression (18.6%), irritability (26.2%), and distress (28.9%). Overall, the quarantine was accompanied by a higher burden for caregivers, often in the form of anxiety and distress (28, 29). Munoz-Bermejo et al. maintained that if caregivers spend 20 hours a week for caregiving, their mental health can be damaged (30). Rodakowski et al. explored care receivers’ functional status and stated that this variable directly affected caregivers’ depression symptoms and was associated with increased caregiving burden (31). According to the literature, caregivers of patients with chronic diseases of the nervous system experience a higher burden and a higher level of depression than caregivers of old adults. They also experience more distress and a higher level of depression (almost twice as high as non-caregivers) (17). In a similar vein, Yu et al. found that a higher level of perceived caregiving burden is associated with a lower level of cognitive function and longer hours of caregiving than non-caregivers (32). It can, therefore, threaten the caregiver’s mental and physical health (33).
Besides, the burden can be increased for long-term caregivers faced with more health issues (32). Particularly in the current conditions and regarding the coronavirus pandemic, caregivers might consider caring for their old patients tougher than before, leading to an increased risk of anxiety, depression, and other psychological disorders (15). Overall, it can be argued that the care-receiver’s low cognitive and functional status is followed by more caregiving activities and spending lower time for moderation and adjustment of familial, occupational, and social affairs (34). Caregivers’ reduced capacity to perform basic daily activities can lead them to experience more caregiving burden (31, 34-38) and can directly affect their mental health (34).
2. Objectives
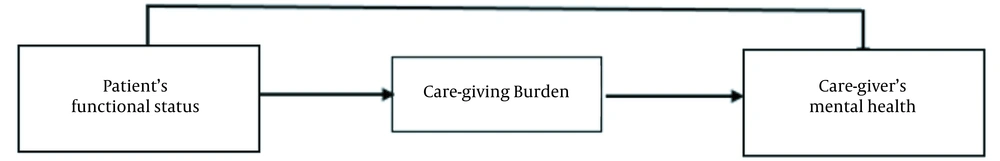
By considering the significance of taking care of old adults, caregivers’ mental health, and the effect of patients’ functional status on the caregivers’ burden and mental health, particularly during the coronavirus pandemic, the present research aimed to explore the moderating effect of caregiving burden on the association between patients’ functional status and caregivers’ mental health. The suggested model of moderating the role of caregiving burden on the association between the functional status of patients and caregivers’ mental health is shown in Figure 1.
3. Methods
This study was performed following a correlational design.
3.1. Participants
The research population comprised caregiver families of old adults (60 years old or higher) afflicted with a chronic disease in the nervous system (e.g., Alzheimer’s disease, Parkinson’s disease, and stroke), and the size of the population was not definitely clear. The sample size was calculated by the Cochran formula, without the population size, as 325 subjects. Participants were recruited following a convenience sampling method, and all of them filled out the questionnaires (n = 325). The inclusion criteria were: (1) Being a family caregiver (upon one’s own will and to be in full charge of taking care of the patient), (2) for patients, be an old adult afflicted with Alzheimer’s disease, Parkinson’s disease, MS or stroke (60 years of old or higher), (3) for caregivers, to be willing to participate in this study, (4) ability to read and write, (5) having no acute physical or mental disease, (6) no history of ecstasy drug abuse, and (7) receiving no payment in return for the caregiving act. The exclusion criterion was the unwillingness to participate or withdraw.
3.2. Research Procedure
Initially, written informed consent was obtained from all participants before entering the study and after a comprehensive introduction to the study protocol. Then, data collection tools, including the demographic information questionnaire, the patient’s functional status, mental health scale, and caregiver’s burden inventory, were converted to electronic versions and sent to the caregivers through emails or social network groups and forums (e.g., forums of patients with Parkinson’s disease), Mehr Association, and brain attrition chatroom a well as other relevant groups. A total of 325 questionnaires were filled out. After applying the inclusion/exclusion criteria and considering the withdrawal of some respondents, 249 questionnaires were considered for statistical analysis. Data were collected from 22 September 2020 to 19 January 2021.
3.3. Instrumentation
3.3.1. Demographic Questionnaire
It contains basic demographic characteristics of participants, including age, gender, occupation, education level, marital status, relation to the patient, length of time taking care of the patient (the overall time of caregiving and the mean hours of weekly caregiving), affliction or non-affliction with an acute physical or mental disease, whether consuming ecstasy drugs, whether receiving any payment for the act of caregiving, patient’s gender and age, patient’s type of disease, main task of caregiving or decision making for the patient, and so on.
3.3.2. Mental Health Questionnaire (MHQ)
The MHQ is developed by Goldberg in 1978 (39). It contains 28 items categorized into four subscales, each with seven items that intend to explore the health state (items 1 to 7), anxiety and sleeplessness (items 8 - 14), one’s capability of standing against professional needs or everyday needs (items 15 to 21), and the state of depression or history of suicide (items 22 to 28). Items one and 15 - 21 are reverse scored. The overall questionnaire is rated on a three-point Likert scale. In each sub-scale, a score of 0 - 7 indicates a severe state of the respondent; one between 7 and 14 represents a borderline level; a score ranging from 14 to 21 indicates a healthy state. Overall, if a respondent receives a total score of 0 - 28 from the 4-scales, his/her state of mental health is identified as severely low; a score of 28 - 56 is interpreted as a borderline state of health; and a score between 56 and 84 represents a good or desirable state of mental health. As for the reliability and validity of Goldberg’s questionnaire, a factor analysis ran in 2004 investigated construct validation of the instrument, which was rated on a Likert scale (40). They used principal component analysis (PCA) with varimax rotation. In this research, the test-retest method was used to evaluate the reliability of the instrument, and the r-value was estimated at 0.74. With a cutoff score of 6.7, the sensitivity and specificity of the test were estimated at 0.88 and 84.2, respectively. The validity of the questionnaire is also tested by Griffiths et al. in 1993 (41). The cutoff point was estimated at 3.4, and the sensitivity and specificity were reported to be 0.81 and 0.82, respectively. Some researchers examined the psychometric properties of this instrument, such as Taghavi, who investigated the validity and reliability of the Persian version of the questionnaire and reported Cronbach’s alpha of 0.9 and 0.97 (42). In this study, Cronbach’s alpha was estimated at 0.83 for the mental health questionnaire. It was found to range from 0.71 to 0.87 for the subscales, which is considered acceptable. Hence, the scale and sub-scales were adequately valid.
3.3.3. Caregiver Burden Inventory
The short form of the caregiver burden inventory was developed in 1989 by Novak and Guest to measure self-care (43). It has 24 items categorized into five subscales of time dependence (items 1 - 5), developmental (items 6 to 10), physical (items 11 - 14), social (15 - 19), and emotional burden (20 - 24). This questionnaire is rated on a five - point Likert scale ranging from zero (‘not at all disruptive’) to 4 (‘strongly disruptive’). The score ranges from 24 to 120. A score of 24 - 47 is interpreted as a low burden; that of 38 - 71 is taken as a moderate burden; a score of 72 to 95 represents a high burden, and a score between 96 and 120 is interpreted as a strong high burden (44). The reliability and validity of the caregiver burden inventory were substantiated (43). The studies showed that the subscales accounted for nearly 66% of the variance of caregiving burden. Moreover, Cronbach’s alpha was estimated at 0.85 and 0.87 for the first and second subscales, respectively, as 0.86, 0.73, and 0.77 for the third, fourth, and fifth subscales. Shafizade et al. reported a Chronbach’s alpha of 0.97 for the Persian version of this questionnaire (45). In the present research, Cronbach’s alpha was estimated at 0.94 for the caregiver burden inventory and 0.79 and 0.93 for the subscales, respectively. These values attest to the acceptable reliability of the scale and its subscales.
3.3.4. Patient’s Functional Status Scale
Lawton-Brody instrumental activities of daily living scale (IADL), developed in 1969, contains 16 items aiming to evaluate an individual’s dependence/independence in daily activities. There are two sub-scales, daily activities (7 items) and instrumental activities (9 items), all to be rated on a three-point Likert scale. A score of zero to 2 represents ‘not able to do so’, ‘I am able to do so with some help’, and ‘I am able to do so without help’, respectively. To estimate the overall score, all scores are added up, the results range from zero to 32. A higher score implies more independence in doing daily activities. A score of zero to 6 implies total dependence, 7 to 12 means slight dependence, and a score of 13 or higher indicates independence. The content validity of the scale was substantiated (46), and researchers also used the test-retest method to substantiate the reliability of the Persian version of this questionnaire, which was estimated at 0.90 (indicating good reliability) (47). In the present research, Cronbach’s alpha was used to test the internal consistency of the scale, which was found to be acceptable for the sub-scales and the overall scale.
3.4. Data Analysis
The collected data first entered SPSS 26 for descriptive and inferential statistical analyses. The former included measures of central tendency, such as frequency, minimum, maximum, percentage, and mean, and measures of variability, including standard deviation. The latter included the Pearson correlation coefficient. These statistical analyses were conducted to explore the caregivers’ and patients’ demographic information and test the research hypotheses. The structural equation modeling (SEM) analysis was done in AMOS to test the moderating effect of the caregiving burden on the relationship between caregivers’ social support and mental health.
4. Results
4.1. Demographic Characteristics
The participating caregivers’ demographic information is summarized in Table 1, which indicates that among 249 caregiving participants, 80.7% were female. The mean age of participants was 45.05 years, of which, by gender, the mean age of women (45.57 years) was slightly higher than men caregivers (42.85 years). The results also showed that a higher percentage of caregivers were employed and married (60.4% and 66.3%, respectively). Also, according to Table 1, the percentage of caregivers with a bachelor’s degree was higher than other groups (38.6%).
| Variable | No. (%) | Mean ± Standard Deviation |
|---|---|---|
| Gender | ||
| Female | 201 (80.7) | - |
| Male | 48 (19.3) | - |
| Employment status | ||
| Working | 98 (39.4) | - |
| Not working | 151 (60.6) | - |
| Marital status | ||
| Single | 84 (33.7) | - |
| Married | 165 (66.3) | - |
| Education | ||
| High school | 16 (6.4) | - |
| Diploma | 60 (24.1) | - |
| Associate Degree | 13 (5.2) | - |
| Bachelor | 96 (38.6) | - |
| Master | 43 (17.3) | - |
| Ph.D. | 21 (8.4) | - |
| Age | ||
| Female | - | 45.57 ± 12.09 |
| Male | - | 42.85 ± 13.47 |
| Total | 249 (100) | 45.05 ± 12.38 |
Distribution of 249 Caregivers of Old Adults with Chronic Disease, Separated by Demographic Variables
Table 2 indicates the patients’ demographic information. Among 249 patients (care receivers), 57.8% were female. The overall mean age was 74.25 years, and the mean age of female patients was higher than male patients (74.25 years). The results also revealed that 54.6% of patients were afflicted with Alzheimer’s disease, 36.5% with Parkinson’s disease, and 8.8% with a stroke. As for caregivers, the results showed that 78% of caregivers were children, and no sibling caregiver was found in the sample. Concerning the duration of caregiving, 83.5% of the caregivers had been taking care of patients for more than a year. Finally, the findings revealed that the participating caregivers spent 48 hours a week, on average, providing care for patients at home.
| Variable | Abundance | Mean ± Standard Deviation |
|---|---|---|
| Gender of care recipient | ||
| Female | 144 (57.8) | - |
| Male | 105 (42.2) | - |
| Type of disease | ||
| Alzheimer | 136 (54.6) | - |
| Parkinson | 91 (36.5) | - |
| Stroke | 22 (8.8) | - |
| Relationship | ||
| Child | 196 (78.7) | - |
| Spouse | 36 (14.5) | - |
| Sister or brother | 0 (0) | - |
| The others | 17 (6.8) | - |
| Duration of care | ||
| Between 1 - 3 months | 11 (4.4) | - |
| Between 3 - 6 months | 8 (3.2) | - |
| Between 6 - 12 months | 22 (8.8) | - |
| More than 12 months | 208 (83.5) | - |
| Average hours of care per week | - | 48.18 ± 47.38 |
| Age of care recipients | ||
| Female | - | 75.15 ± 8.62 |
| Male | - | 73.01 ± 8.60 |
| Total | 249 (100) | 45.05 ± 12.38 |
Distribution of 249 Old Adults with Chronic Disease, Separated by Demographic Variables
4.2. Bivariate Analysis
As shown in Table 3, the mean score of patients’ functional status, caregiving burden, and mental health was 10.96, 70.07, and 52.50, respectively. This finding shows that the patients enjoyed a moderate functional status and were, thus, slightly dependent on others. Their caregivers experienced a moderate level of caregiving burden and borderline mental health. Moreover, according to Table 3, the Pearson correlation coefficient showed a statistically significant positive correlation between patients’ daily activities and the physical symptoms of caregivers’ mental health (r = 0.14, P < 0.05). Similarly, a statistically significant positive correlation was found between this variable and the anxiety symptoms of caregivers’ mental health (r = 0.21, P < 0.01). Yet, patients’ physical activities did not show to be correlated with the social and depression symptoms of caregivers’ mental health (r = 0.1, r = 0.05, P > 0.05). As for the correlation between patients’ instrumental activities and caregivers’ dimensions of mental health, similar to the daily activities, this variable and the physical symptoms of mental health showed a significant, positive correlation (r = 0.16, P < 0.05). Moreover, this variable and the anxiety symptoms of caregivers’ mental health showed to be positively and significantly correlated (r = 0.23, P < 0.01). Yet, no significant correlation was found between this variable and the social and depression symptoms of mental health (r = 0.1, r = 0.05, P > 0.05). Overall, there was a statistically significant positive correlation between patients’ functional status and anxiety symptoms (r = 0.24, P < 0.01), physical symptoms (r = 0.16, P < 0.05), and the total mental health score (r = 0.17, P < 0.01). No statistically significant correlation was found between this variable and the social and depression symptoms of mental health (r = 0.09, r = 0.00, P > 0.05). Generally, the results revealed a statistically significant positive correlation between patients’ functional status and mental health (r = 0.17, P < 0.01). This significant correlation points to the fact that a patient’s lower functional status is associated with limited independence in daily and instrumental activities and the caregiver’s lower state of mental health, and vice versa. The results also showed a statistically significant negative correlation between the patient’s functional status and caregiving burden (r = -0.44, P < 0.01). In other words, the higher the patient’s functional status score and the more independence he/she has in daily activities, the less the caregiver’s caregiving burden.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Mean ± Standard Deviation |
|---|---|---|---|---|---|---|---|---|---|---|
| Patients’ functional status | 1 | 10.96 ± 8.83 | ||||||||
| Daily activity | 0.92** | 1 | 7.22 ± 4.64 | |||||||
| Instrumental activity | 0.93** | 0.7** | 1 | 3.74 ± 4.88 | ||||||
| Care burden | -0.44** | -0.41** | -0.41** | 1 | 70.07 ± 18.81 | |||||
| Total mental health | 0.17** | 0.17** | 0.15* | -0.61** | 1 | 52.50 ± 12.67 | ||||
| Physical symptoms | 0.16* | 0.14* | 0.16* | -0.57** | 0.82** | 1 | 12.76 ± 4.38 | |||
| Anxiety symptom | 0.24** | 0.21** | 0.23** | -0.62** | 0.85** | 0.17** | 1 | 12.55 ± 4.36 | ||
| Social symptoms | 0.00 | 0.05 | -0.03 | -0.21** | 0.61** | 0.28** | 0.26** | 1 | 10.31 ± 3.87 | |
| Depression symptoms | 0.09 | 0.10 | 0.06 | -0.47** | 0.80** | 0.48** | 0.61** | 0.4** | 1 | 16.88 ± 3.78 |
Correlation That That Shows the Correlation, Mean, and Standard Deviation of Variables
Other analyses of correlation indicated the differences between groups of gender, so that the correlation between patients’ functional status and caregivers’ mental health in the female group of caregivers was statistically significant, and it was not significant for males. This result may show that female caregivers are at higher risk of health damage than males in the caring process of old adults with chronic illnesses. Also, the findings showed that female caregivers tolerate more caring burden than males, indicating their need for more additional support than men.
4.3. Path Analysis
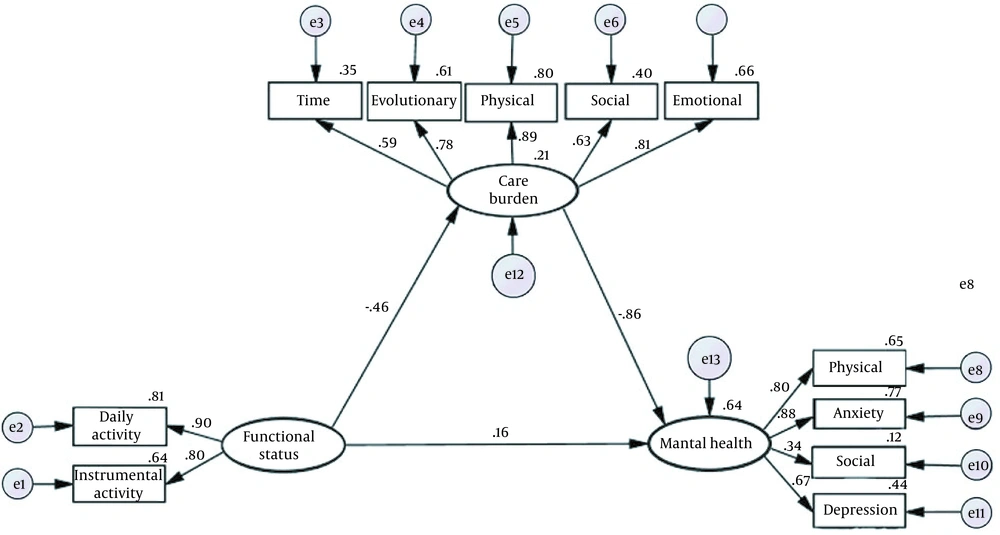
To answer the question of ‘Does the caregiving burden moderate the association between patient’s functional status and caregiver’s mental health?’, we used SEM analysis to plot the following model (Figure 2). The goodness of fit indices was used to substantiate the model fitness. The model fitness was confirmed.
Chi-squared value was estimated for the model at 2.58; the goodness of fitness index (GFI) was estimated at 0.92; the adjusted goodness of fitness index (AGFI) was found to be 0.85; the comparative fitness index (CFI) was estimated at 0.92; the increase fitness index (IFI) was found to be 0.96; the normalized fitness index (NFI) was 0.93; the Tucker-Lewis fitness index (TLI) was 0.90, and the root mean square error of approximation (RMSEA) was estimated at 0.07. The output of the abovementioned tests all attests to the fitness of the final model. Hence, we can conclude that the caregiving burden moderates the association between patient’s functional status and caregiver’s mental health.
Table 4 summarizes the direct, indirect, and total effects of patient’s functional status on caregiving burden and mental health. As it can be observed in Table 4 and Figure 2, patient’s functional status affected mental health both directly and indirectly. The latter was moderated by caregiving burden. Table 4 also shows that 64% of mental health variance in the model is explained by exogenous and moderating variables (i. e. patient’s functional status and caregiving burden). Moreover, 21% of the caregiving burden variance is explained by patient’s functional status. Generally, we can conclude that the relationship between patient’s functional status and caregiver’s mental health is moderated by the caregiving burden.
| Variables | Direct Impact | Indirect Effect | Total Effect | Variance |
|---|---|---|---|---|
| On mental health from: | 0.64 | |||
| Patient functional status | -0.16 | 0.40 | 0.24 | |
| Care burden | -0.86 | ---- | -0.86 | |
| On the burden of caring from: | 0.21 | |||
| Patient functional status | -0.46 | ---- | -0.46 |
The Output of Path Analysis, Including Path Coefficients of Direct, Indirect, and Total Impact of Functional Status of Patient with Chronic Disease on Mental Health of their Caregivers
5. Discussion
This study demonstrated that 37% of patients were totally dependent on caregivers, while 28.1% were slightly dependent on help with daily activities, such as eating, taking a bath, and instrumental activities. The results also showed that caregivers experienced a moderate caregiving burden and borderline mental health. Besides, 86% of the caregivers reported experiencing a higher caregiving burden during the coronavirus pandemic, and 76% reported spending more time taking for caring patients. Due to the progressive nature of chronic diseases and considering the fact that the rising age is accompanied by many different diseases for old adults (7), their independence is limited and they come to need help with daily and instrumental activities (9, 13). This finding is consistent with the findings of the present study that 50% of care receivers (patients) are dependent on others. A body of research showed that more than half of old adults have problems doing basic daily activities (48). Similarly, Benjamin et al. and Klimova et al. showed that old adults afflicted with Alzheimer’s disease at the final stage of the disease had to stay in bed, and 45% of stroke survivors get fully dependent on caregivers after discharge from the hospital (49, 50). The progression of old adults’ disease is accompanied by certain complications that are closely linked with the lost autonomy in doing daily activities. Thus, they end up needing others’ help and caregiving at home (12). Old adult patients facing problems in daily and instrumental activities need others’ to help them more than ever before the progression of the disease takes the caregiver’s time more than before (51), and they should spend more time taking care of old adults probably with other diseases too (52, 53). Moreover, in agreement with this finding (the correlation between patient’s dependence for daily activities and caregivers’ overall mental health), Shukri et al. found that caregivers of patients having problems doing daily activities suffer from higher levels of cognitive disorders (by 2.99 times) (54). They are also more prone to depression, which is a key component of mental health. Besides, caregivers of patients highly dependent on help showed to spend 2.63 times as much time as peers on caregiving, and they were at a higher risk of depression. According to Zhong et al., a patient’s functional status directly affects caregivers’ depression symptoms, a key component of mental health (34). Concerning the effect of coronavirus and the consequent quarantine, scientists reckoned that patients with higher physical independence probably live a more active life and are adversely affected by the quarantine (29). During the caregiving task, caregivers attempt to take care of themselves against the virus and also attempt to protect the patient against the infection and prevent the transmission of the disease to others. Thus, they undergo too much burden, which significantly challenges their job and also their self-care attempts. Instances of these challenges are many family caregivers who take care of both their children and old parents. The difficulty of managing these tasks and duties besides one’s occupation, school closure, lack of recreation facilities and leisure, and the difficulty of taking care of the old adults have significantly burdened them (55). In the light of the present finding and the related literature, we can infer that during the pandemic, caregivers experience lower mental health for different reasons. These can be the absence of any nurse and assistant to help with the caregiving, the adverse effects of quarantine on patients’ behavior and functional status, which can increase the caregiving time and be followed by more physical pressures and low mental health. Furthermore, because not all family caregivers are well educated in serving highly dependent patients, they can become socially isolated after a while. This excessive dependence can directly cause mental issues. On the one hand, patients’ functional status directly affects caregivers’ mental health. On the other hand, as the related literature showed, the caregiving burden plays a moderating role in the association between patients’ functional status and caregivers’ mental health. In other words, patients’ functional status can affect caregivers’ mental health through an intervening effect on the caregiving burden. This effect can be attributed to several reasons. For one, old adults’ disabilities and too much dependence on the caregivers can increase the load of caregiving activities. Thus, caregivers hardly find enough time for themselves, their families, leisure, occupation, and social interactions. The time they spend on taking care of old adult patients is lengthened. This dependence, which adds to the burden of caregiving activities, can threaten caregivers’ health. The caregiver can feel severely pressed, and this pressure and burden can, in turn, lower his/her mental health. According to a study by Cao and Yang, the caregiving burden can significantly damage family caregivers’ physical and mental health. They also mentioned that the caregiving burden could moderate the association between patients’ functional status and the anxiety that the caregivers experience (56). Similarly, the present research revealed that the caregiving burden is strongly associated with mental health. Thus, we can conclude that patients’ functional status can affect caregivers’ mental health by affecting the caregiving burden. Concerning the influence of patients’ functional status on the caregiving burden experienced during the coronavirus pandemic, Rainero et al. maintained that the quarantine significantly affected patients’ cognitive and behavioral symptoms (28). Patients experienced more motor disorders because of the social isolation-induced by the quarantine (29). They mentioned the level of physical independence before the quarantine as the best predictor for the severity of patients’ illness. They finally concluded that about half of the caregivers reported the quarantine had tremendously changed their lifestyle, and they had experienced much more caregiving burden during the quarantine, often accompanied by more distress and anxiety. It is also followed by a high rate of anxiety, depression, irritability, and distress. To conclude, we can say that because caregivers are more pressed than usual during the coronavirus pandemic and are faced with more problems for themselves and their patients, and because most caregivers have no psychological support and need to also take care of themselves, they need alternative ways to rest and manage anxiety more than ever before (57). They not only should take care of their body against the virus infection but should also take care of their mental health. For instance, they should refrain from watching, reading, or listening to the news. They can benefit from the deep breathing technique, body stretch, and meditation. In addition, they are recommended to follow a healthy and well-balanced diet, have enough sleep, and avoid alcohol or drugs. They can benefit from a supportive network to share concerns, information, problems, and emotions with family or friends (15).
5.1. Limitations
It is necessary to mention some limitations of our study, including difficulties in access to the target group due to lockdowns imposed to control the COVID-19. Also, the high number of items that should have been filled led to the reluctance of some people to participate in this study.
5.2. Suggestions for Further Research
(1) Conducting interventional research and educational programs for old adult caregiving to improve mental health or prevent caregiving burden;
(2) Comparing caregiving burden across caregivers of patients with Alzheimer’s disease, Parkinson’s disease, MS, and stroke;
(3) Exploring the effect of a formal education program on caregiving burden and mental health;
(4) Using services such as medical staff and physiotherapy for patients to improve their functional status and exploring its effect on caregivers’ mental health and burden;
(5) Educating caregiving and raising caregivers’ knowledge and literacy and consequently the quality of their caregiving; and
(6) Educating how to communicate with patients, particularly for those taking care of patients with Alzheimer’s of dementia.
5.3. Conclusions
In the light of the present findings, we can conclude that patients’ functional status and the caregiving burden experienced can be a good predictors of mental health. Thus, mental health specialists are recommended to develop different educational programs on how to communicate with patients, how to do the caregiving activities, and how to adapt to changing conditions. Also, there is a need for interventions that can help patients to improve their functional status to prevent the caregiving burden and improve caregivers’ mental health. Such interventions can be used to improve caregivers’ physical and mental health and raise the quality of life and the quality of care services provided to old adults, who are precious assets and sources of knowledge to a nation even during the pandemic. This also can help old adults to live better lives.