1. Background
Sleep is an important and dynamic process in infants, children and adolescents. The development of sleep parallels neurologic, physical, and behavioral development, and reciprocal relationships can be found between these aspects of development. In recent years, according to studies on the importance of quantity and quality of children’s sleep, the role of sleep disorders in the quality of life of children and their parents has received much attention. Insomnia is a common sleep complaints in pediatrics, with a prevalence of 20 - 30% (1).
This disorder is in the fifth edition of the diagnostic and statistical manual of mental disorders (DSM-5) as well as the third edition of the international classification of sleep disorders (ICSD-3) in the form of dissatisfaction with sleep quantity or quality (e.g., difficulty in initiating sleep, maintaining sleep, or waking up early in the morning and being unable to return to sleep) defined for at least three nights per week for at least three months in spite of enough opportunity for sleep that leads to feelings of distress and impaired performance (2). Behavioral insomnia in children is generally divided into the limit-setting subtype and the sleep onset associations subtype (1). The first subtype occurs when a child refuses to or delays going to bed when the caretaker stipulates. The second subtype is due to the child’s dependency on specific objects, stimulation, or setting for initiating sleep or returning to sleep (3).
Insufficient sleep in children and adolescent disrupts the functioning of the cardiovascular (4), immune, and various metabolic systems (5); also it can with effect on central nervous system lead to alteration in the neurobehavior, emotion and mood neurocognitive functions (4). For instance, insomnia might decrease glucose metabolism in the prefrontal, posterior parietal, thalamic regions, affecting alertness and restorative processes, and leading to prefrontal cortex dysfunction. Deficiencies in working memory, executive functioning, impulsivity, academic performance, sleepiness, and daily fatigue are other consequences (6).
It is noteworthy that this disorder, by changes in the activity level and function of the appetite regulating hormones, such as ghrelin, leptin, resistin, adiponectin and orexin, leads to an increase in fat and obesity (7). Moreover, insomnia by an elevation in the sympathetic nervous system activity, dysregulation in hypothalamic-pituitary-adrenal (HPA) axis activity, and an increase in inflammatory cytokines such as tumor necrosis factor-alpha, interleukin 6 and C-reactive protein increases the risk of cardiovascular diseases, such as hypertension and atherogenesis, also increases insulin resistance, type 2 diabetes, and mortality (8).
Attention deficit hyperactivity disorder predominantly hyperactivity-impulsivity presentation (9), anxiety, depression (10), suicidal thoughts, and high-risk behaviors, including alcohol abuse, substance abuse, crime, and violence, are other adverse outcomes of insomnia and poor sleep quality in children and adolescents (11).
Therefore, due to the widespread consequences of insomnia persistence and the role of perpetuating factors of the behavioral and cognitive in causing insomnia (12), the use of interventions based on psychological principles, such as individual, group, online, web-based or telephon-based multicomponent cognitive-behavioral therapies (CBT-I), for insomnia is recommended (10). The therapeutic approach includes a combination of psychoeducational, bahaviral, and cognitive strategies (13).
The KiSS program, is the CBT-I program. This program is comprised of sleep education and sleep hygiene education, relaxation, stimulus control therapy, sleep restriction, and cognitive restructuring strategies. Also, in some session used of imaginative or hypnotherapeutic strategies (14). Therefore, the psychoeducation strategies of CBT-I can correct misconceptions, reduce worry, and create the optimal environment for the letting down of vigilance. The Behavioral strategies are capable of eliminating environmental reinforcement and learned associations. Whereas, the cognitive strategies change the dysfunctional cognition of parents and children to change the child's sleep patterns, to deal with bedtime fears and the consequences of insomnia (13). Also, hypnotherapeutic strategies can be used to increase personal control as well as to create awareness of physical changes that occur in relation to changes in the mind.
Evidence for the short-term effectiveness of the KiSS program on insomnia were demonstrated in a pilot study by Schlarb et al. (15). Then, Schlarb et al. examined the short and long-term effects of the KiSS program on chronic insomnia in children. The results of the aforementioned study showed that this program leads to changes in sleep parameters, including improvement in sleep onset latency (SOL), number of nocturnal awakenings per night, sleep efficiency (SE), and daytime sleepiness. In the follow-up stage, these results after 3, 6, and 12 months remained stable (16).
In this regard, other CBT-I studies have had similar results. The first study, Paine and Gradisar examined the effect of CBT-I on behavioral insomnia in school-aged children. Children showed significant improvements in sleep latency, waking up after sleep onset, (SE), and sleep anxiety but not TST (17).
In another study, Ma et al. published a systematic review and meta-analysis on the efficacy of CBT-I in children and adolescents with insomnia. A significant pooled effect size was reported for SOL and SE% and no significant pooled effect size was reported for TST (10).
In addition to the CBT-I, the use of therapeutic approaches of complementary medicine that directly affect the predisposing factors of biological and physiological, cortical arousal, sympathetic system activity, and the HPA axis in individuals with insomnia is recommended for the treatment of this disorder (2).
Reflexotherapy is a form of natural, holistic therapy (18) in which pressure is applied with specific thumb and finger techniques on reflex points on hands, feet, and ears. Based on the reflexotherapy theory, there are 10 equal longitudinal zones, invisible electrical currents, running the length of the body from the top of the head to the tips of fingers and toes. Reflexotherapy is based on the principle that reflex points connect with organs, glands, or systems and structures within the entire body (19).
In this treatment, by stimulating the reflex points of each disorder, not only local reactions but also physical and psychological reactions are created at the end of each session throughout the body. Physical reactions appear in the form of energy balancing by unblocking zones, improvement in endocrine function, and increase of hormone secretion, neurotransmitters, circulatory flow, and parasympathetic nervous system activity (20), urination and toxins excretion, pain relief, deep relaxation, sleepiness, change of sleep pattern, restoration of homeostasis, and increase of immune system performance. Psychological reactions also appear in the form of the improvement of concentration, reduction of fear, worry, and anxiety, and improvement of quality of life; accordingly, most individuals improve significantly after three to six sessions (21). In addition to the above-mentioned effects, Esmel-Esmel et al. stated that reflexology can induce variations in the brain waves activity in correspondence with the appearance of a high degree of sleepiness and sleep (N1 and N2 nonrapid eye movement [NREM] sleep) (22).
Recently, in a meta-analysis, Huang et al. examined the effect of foot reflexology on adult sleep disturbances. The results of the aforementioned study showed that foot reflexology is a noninvasive and convenient intervention to alleviate sleep disturbances and improve the sleep quality of adults (23).
2. Objectives
According to differences between the KiSS program and reflexotherapy in terms of underlying principles and the method and mechanism of action and the fact that no research has been performed on the comparison of the effectiveness of these two nonpharmacological treatments in pediatric insomnia and professionals’ insufficient knowledge of choosing the best treatment strategy, the present study compared the effectiveness of the KiSS program and reflexotherapy on insomnia among children.
3. Methods
3.1. Design
The method of the present research was quasi-experimental in which a pretest-posttest and follow-up design was used in two experimental and two control groups.
3.2. Sample
The statistical population of this study included children of 8 - 10 years with insomnia referring to Medical & Psychology Clinic of Shokoufeh, Tehran, Iran, within July to October 2021. The sample size was estimated to be about 17 children by considering the variable of children sleep disorders in Schlarb et al.’s study with scores of 7.25 ± 44.55 and 6.86 ± 51.25 for both experimental and control groups (16), respectively, power of test 80%, confidence of 90% using the comparing means formula (24) in each group, which with a probability of sample drop out was finally considered 20 children in each group. Accordingly, 80 children were selected by the convenience sampling method.
3.3. Inclusion/Exclusion Criteria
The inclusion criteria were the parent's willingness and their children to participate in the study, having literacy level at least diploma for children's parents, obtaining a T score above 70 in the subscale of disorders of initiating and maintaining sleep.
The exclusion criteria were also having other sleep disorders in Sleep Disturbance Scale for Children (SDSC) scale, having history of organ transplant surgery and physical disease such as cardiovascular disease, epilepsy, and skin disease, fracture, wounds, inflammation or infection in the feet because they would not be able to receive reflexotherapy, having emotional or behavioral disorders in Child Symptoms Inventory-4 (CSI-4) and using other treatments simultaneously or 6 months before the KiSS program and reflexotherapy.
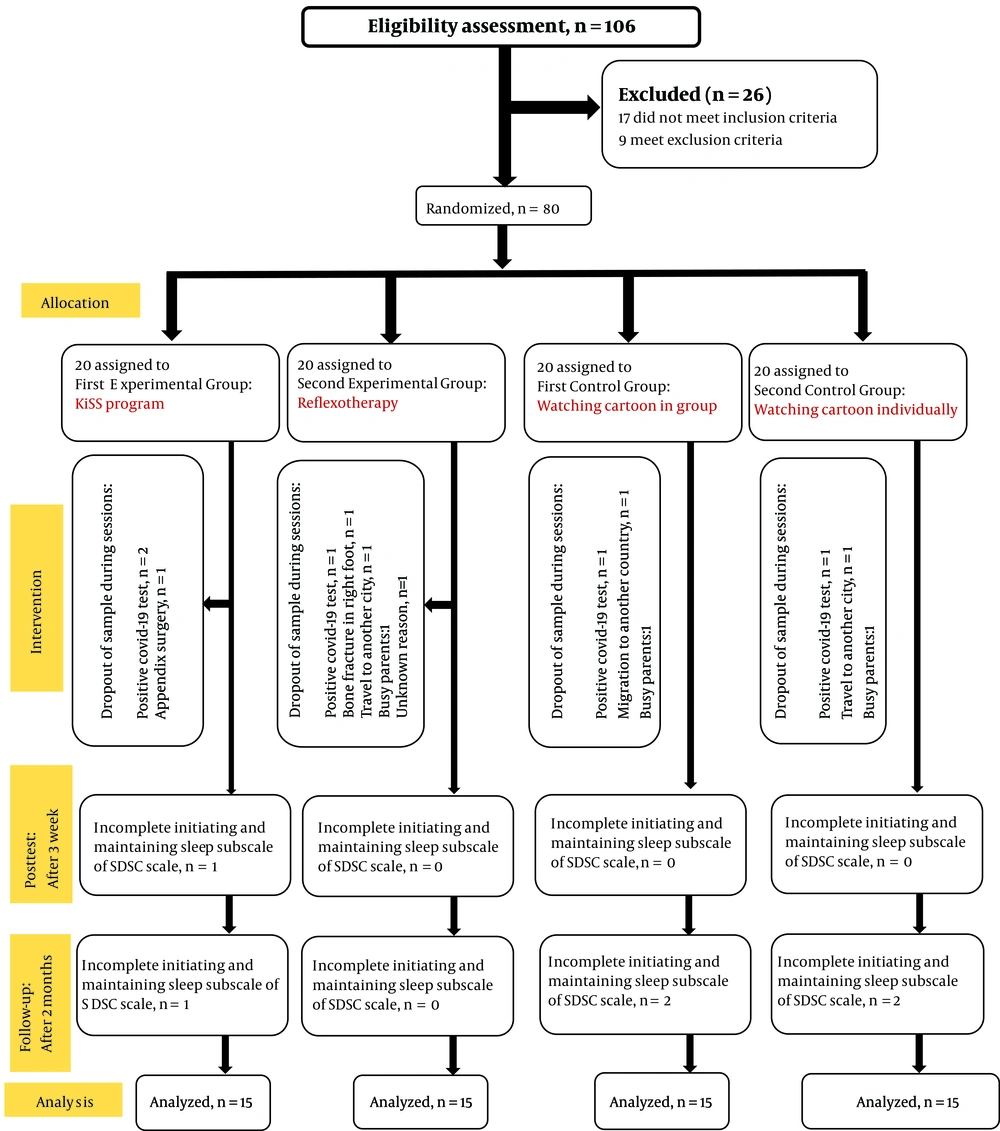
The children were randomly assigned to two experimental and two control groups (20 individuals per group). Since more studies have shown that there is a positive correlation between the group cohesion, patient’s recovery and outcome of treatment in group therapy (25). So, in this study due to the difference in the implementation of the two intervention methods (i.e., group-individual) and in order to control the effect of the group cohesion on the research results, two control groups were used (Figure 1).
3.4. Study Questionnaires
Questionnaires used in this study included a Personal Information Questionnaire, SDSC, and CSI-4 presented in the subsequent sections.
3.4.1. Personal Information Questionnaire
According to the objectives of the research, the items of Personal Information Questionnaire were designed by a researcher in the field of date of birth according to the birth certificate, gender, parents’ education, child’s medical history and use of drugs, and Parent's solutions about sleep disorder of the child.
3.4.2. Sleep Disturbance Scale for Children
The SDSC was designed by Bruni et al. (26) to assess sleep disorders in children of 6 - 15 years. The SDSC is a 26-item scale that examines children’s sleep status over the past 6 months. By the use of factor analysis, Bruni et al. divided the items into six subscales, including initiating and maintaining sleep disorders (seven items), sleep breathing disorders (three items), arousal/nightmare disorders (three items), sleep-waking transition disorders (six items), excessive somnolence disorders (five items), and nighttime sweating (two items).
The parent or caregiver completed the questionnaire using pencil-and-paper within 10 - 15 minutes. Scoring is performed based on a five-point Likert scale. Total scale scores range from 26 to 130, (26) and higher scores indicate more acute sleep disturbance. The total score and the score of each subscale are converted to a T score for interpretation. Based on T-score, children are divided into three clinical categories, namely normal (T score < 50), borderline (T score: 50 - 70), and clinically significant (T score > 70) (27).
Bruni et al. performed a psychometric evaluation of SDSC and reported the internal consistency ranging of 0.71 to 0.79, diagnostic accuracy of 0.91, and test-retest reliability of 0.71. Bruni et al. reported acceptable sensitivity and specificity of this scale for distinguishing between the control group and children with sleep disorders to be 0.89 and 0.74, respectively (26). In Ghaneian and Kazemi-Zahrani’s study, the reliability of this scale was reported as 0.72 (28).
3.4.3. Child Symptom Inventory-4
The CSI-4 as a behavior rating scale designed by Sprafkin and Gadow to screen children for emotional and behavioral disorders within 5 to 12 years in 1994 with the publication of the fourth edition of (DSM). The latest edition of the Child Symptoms Questionnaire, as in previous versions, has two checklist, including parent and teacher. The parent checklist was used in the present study. This checklist has 97 items that each item is answered a 4-point Likert scale. There are two scoring procedures, namely symptom count scores and symptom severity scores. In this study, the count score method was used.
In this method, an individual’s score is obtained by adding the number of phrases they answered with “often’ and “very often”. In Mohammad Esmaeel’s study (29), test-retest reliability coefficients were estimated from the lowest level (0.29) for a social phobia to the highest level (0.76) for conduct disorder. Except for social phobia, all were significant at the level of 0.01.
Experts’ positive comments and judgments about the homogeneity and appropriateness of CSI-4 content with the measured domain confirmed the content-related validity for identifying and screening behavioral and emotional disorders in children.
Criterion-related validity was evaluated by comparing disorders’ scores and psychiatric-based diagnoses. The high specificity and sensitivity of majority disorders in the questionnaire indicate the criterion-related validity of this inventory.
Significant differences in the scores of normal and clinical groups in all disorders indicate appropriate discrimination validity (29).
3.5. Intervention Protocols
3.5.1. KiSS Program
This cognitive- behavioral therapy protocol was developed by Schlarb, a psychologist at the University of Tübingen, Germany, in 2013 to treat insomnia in children of 5 - 10 years, including sleep education and sleep hygiene education, relaxation, stimulus control therapy, sleep restriction, and cognitive restructuring for children and parents. Also, in some session used of imaginative or hypnotherapeutic strategie for pediatrics. Furthermore, the children is given a soft toy, the leopard Kalimba, as a therapy puppet and coping model.
The KiSS treatment is performed in six sessions with 4 - 6 children in each group (three sessions for children and three sessions for parents in 3 weeks). The duration of each weekly session is about 100 minutes (14). This protocol was translated by Baghdassarians and Bagheri in 2016 and used for the first time in Iran. A summary of the structure and content of the sessions is as follows:
The first session (parent): Sleep and parents’ behavior
- Introduction: Familiarity with each other
- Psychoeducation (CBT-I): Sleep and its disorders, prevalence, influence factors, and sleep problems consequences
- Parental behavior and sleep (CBT-I): Bedtimes routines, sleep hygiene rules, reward system
- A brief overviewto the sessions for children: Working with Kalimba and relaxation methods
- End of the session: Evaluation of session, and homework
The second session (children): Sleep helper Kalimba
- Introduction: Familiarity with each other, what are we doing here? rules of the sessions
- Psychoeducation (CBT-I): What is the reason for sleeping? and what are your sleep problems?
- Do you know Kalimba (CBT-I: Coping model): Sleep helper, magic spots for favorable sleep, and magic breathing method (relaxation and deep breathing)
- Imagination: Being powerful with knights’ armor (imaginary method)
- End of the session: Reward and homework
The third session (parent): Solving sleep problem
- Introduction: First experience, and changes
- Parental behavior and sleep (CBT-I): Behavior analysis, essential parenting strategies, stimulus control, and positive self-reinforcement
- End of the session: Evaluation of the session and homework
The fourth session (children): Being brave and strong
- Introduction: Report on homework and asking about something happened at home?
- Sleep hygiene (CBT-I): Your bed and the bedtime routine are important
- Overcoming sleep-related fears (CBT-I): Strategies to deal with sleep-related anxieties, learning imaginary methods, and increasing self-esteem by becoming a hero (i.e., coping mechanism)
- Imagination: I use sleep tree for sleep (imaginary method)
- End of the session: Rewards and homework
The fifth session (children): My toolbox for good sleep
- Introduction: Report about homework and are you a hero?
- Sleep hygiene (CBT-I): My cozy corner
- Revising strategies: Sleep tools and quiz
- Imagination: Kalimba’s friends
- End of the session: Rewards, and Kalimba says (bye-bye)
The sixth session (children): Review
- Introduction: Experience and alternations
- Parenting behavior and sleep (CBT-I): Revision of positive parenting behavior, being consistent is important, and revision of sleep hygiene
- Imaginations and stories
- End of the session: Session evaluation
3.5.2. Reflexotherapy Protocol
The reflexotherapy protocol and reflex points of insomnia disorder presented by James, reflexology specialist of the London School of Reflexology (30) were translated by Baghdassarians and Bagheri in 2016 and used for insomnia in children. The structure and contents of reflexotherapy sessions and reflex points of insomnia disorder are discussed in the next part.
The parents of children in the reflexotherapy group are taught during a session about the duration of treatment, the necessary equipment (i.e., sheets and towels to keep your feet warm), not using varnish during six sessions of treatment, not using food one hour before the treatment session, and not using jewelry and watches during sessions, not doing exercise activities two hours after the therapy session. Then, reflexotherapy is performed twice a week; each session lasts 60 minutes, and six sessions in the treatment center are held by the therapist. During each treatment session, the child lies on the examination bed in a quiet room with low light and a suitable temperature (31).
After placing the moderately thick pillow under the child’s head, knees, and lower legs and placing the hands on the sides of the body (21), the steps of preparing the foot, relaxing the foot, and stimulating the reflex points of insomnia are followed, respectively.
- In the preparation stage, after cleaning the feet with cotton and a solution of water and alcohol, according to special rules, lavender oil or Vaseline is used to lubricate the feet (31).
- In the relaxation phase, 10 techniques are used to relieve tension in the leg muscles and increase blood circulation. These techniques include: Ankle rotation technique, wringing the foot, finger stretching and rotation, solar plexus rotation and relaxation, longitudinal zoning relaxation, knuckle draw and roll, hacking, chest stretch, dorsal and soles friction, side to side relaxation and friction (32).
- Then, using the thumb-walking technique and tonify, the reflex points of the brain, hypothalamus, brainstem, pituitary gland, pineal gland, adrenal gland, solar plexus, spine and diaphragm are worked on the soles of both feet, respectively. Each session will end with the participant’resting for 10 minutes and drinking a glass of water (31).
3.5.3. Watching the Cartoon
The children of the first control group watched the cartoon in groups of four members, two sessions per week and each session lasting 60 minutes for six sessions. The children of the second control group watched the cartoon individually, two sessions per week and each session lasting 60 minutes for six sessions.
3.6. Intervention
In this study, of 106 children referring to Medical & Psychology Clinic of Shokoufeh, 80 children who met the inclusion and exclusion criteria were selected according to convenience sampling method. The scores of children diagnosed with insomnia in the initiating and maintaining sleep subscale of SDSC were used as pretest scores to be compared with posttest and follow-up scores.
The children were randomly assigned into two experimental groups of the KiSS program and reflexotherapy (20 children in each group) and the first and second control groups (20 children in each group). Then, the children of the KiSS program and the first control group were randomly divided into five subgroups of four members. Therefore, the KiSS program was applied in the first experimental group and watching cartoons in the first control group. Reflexotherapy was applied in the second experimental group and watching cartoons in the second control group individually. At the end of the treatment sessions, the disorders of initiating and maintaining sleep subscale, or in other words, the first posttest at the same time, were completed by the parents of the two experimental and control groups. Furthermore, the insomnia scores were calculated and again after 2 months at a specific time completed by the parents of the children. It is noteworthy due to dropout the samples for different reasons, for example, positive covid-19 test, incomplete initiating and maintaining sleep subscale of SDSC scale, surgery, bone fracture, travel, migration and busy parent in the implementation phase, posttest and follow-up in all four groups, the number of children in each group was reduced to 15 individuals.
3.7. Statistical Analysis
The data were analyzed with SPSS 22 using descriptive statistical indicators, including mean and standard deviation, as well as inferential statistics indicators, including mixed-design analysis of variance (ANOVA) method.
4. Results
As previously mentioned, in the present study, there were four groups and 15 participants in each group. The mean age values of children in the KiSS program and reflexotheraphy groups were 8.93 ± 0.83 and 8.80 ± 0.91 years, respectively. The mean age values of children in the first and second control groups were 8.97 ± 0.74 and 9.07 ± 0.70 years, respectively. According to the results of one-way ANOVA no significant difference was found between the groups in age. According to the chi-square test, no significant difference was detected between the groups regarding gender.
Based on the results of Table 1, the Shapiro-Wilk index related to the dependent variable was not significant in any of the groups and any of the implementation stages at the level of 0.05. This finding indicated the normal distribution of the insomnia variable in four groups and three implementation stages. The result of Levene’s test in evaluating the assumption of the equality of error variances showed that the difference in error variance of insomnia scores in the three stages of pretest, posttest, and follow-up was not significant at the level of 0.05. This finding confirmed the assumption of the equality of error variances between the data. Moreover, the results of one-way ANOVA showed no significant difference between the groups in insomnia before the intervention (F [3, 56] = 0.64; P < 0.05). Also, the assumption of the equality of variance-covariance matrices of the dependent variable for insomnia was (Box’s M = 4.85; F = 0.42; P = 0.867) established at the level of 0.05.
| Groups | Mean (Standard Deviation) | Shapiro-Wilk | ||||
|---|---|---|---|---|---|---|
| Pretest | Posttest | Follow-up | Pretest | Posttest | Follow-up | |
| KiSS program | 24.07 (4.06) | 10.73 (3.06) | 10.47 (2.82) | 0.915 (0.162) | 0.955 (0.600) | 0.919 (0.189) |
| Reflexotherapy | 24/80 (3.65) | 9.67 (2.35) | 17.53 (2.36) | 0.950 (0.521) | 0.914 (0.157) | 0.960 (0.697) |
| First control group | 24.27 (4.15) | 24.47 (3.92) | 24.67 (3.52) | 0.922 (0.206) | 0.948 (0.491) | 0.972 (0.881) |
| Second control group | 22.87 (3.91) | 23.27 (3.73) | 23.60 (3.62) | 0.941 (0.390) | 0.889 (0.065) | 0.963 (0.742) |
Mean, Standard Deviation and Shapiro Wilk of Insomnia Index in Experimental and Control Groups
The results also showed that the interaction effect of time × group on insomnia (F = 107.87 [110, 6]; P = 0.001; η2 = 0.855; Wilks’ lambda = 0.021) was significant at the level of 0.01. According to the results of Mauchly’s test, the value of chi-square related to insomnia (χ2 [2] = 0.864; W = 8.7; P < 0.05) was significant at the level of 0.05; therefore, the assumption of sphericity was violated. For this reason, degrees of freedom were corrected using the Greenhouse-Geisser method. The results of mixed-design ANOVA analysis (Table 2) also showed that the interaction effect of time × group on insomnia (F [5.28, 98.56] = 144.81; P = 0.001; η2 = 0.886) was significant at the level of 0.01.
| Sum of Squares | Error Sum of Squares | df | F | P | η2 |
|---|---|---|---|---|---|
| 1997.69 | 257.51 | 5.28, 98.56 | 144.81 | 0.001 | 0.886 |
Results of Mixed-Design ANOVA Method for the Interaction Effect of Group × Time on Insomnia
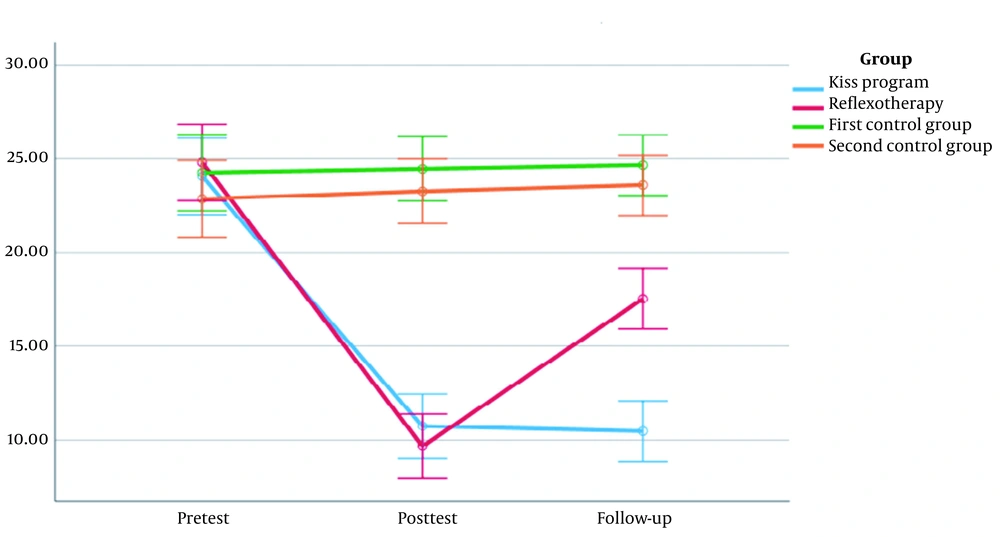
Then, analyses were performed to pairwise compare the interactive effect of group × time on insomnia, the results of which are presented in Table 3. According to the results of Table 3, the KiSS program reduced insomnia to a significant level of 0.01, compared to the first control group (F [1.67, 46.87] = 236.92; P < 0.01). Figure 2 also shows that the mean scores of insomnia in the KiSS program group decreased, compared to those of the first control group in the posttest phase, and the changes in the follow-up phase remained. Although according to the results of Table 3, reflexotherapy also affected insomnia at a significant level of 0.01, compared to the second control group, (F [1.81, 50.68] = 174.27; P < 0.01), Figure 2 shows that the effect of this independent variable in reducing insomnia was not stable and insomnia scores in the follow-up stages increased significantly. Therefore, based on the results of Table 3, the difference between the effectiveness of the KiSS program and reflexotherapy in insomnia among children (F [1.73, 48.46] = 34.21; P < 0.01) was significant at the level of 0.01. This difference is shown in Figure 2.
| Groups | Sum of Squares | Error Sum of Squares | df | F | P | η2 |
|---|---|---|---|---|---|---|
| The first group a - the second group b | 273.76 | 224.09 | 1.73, 48.46 | 34.21 | 0.001 | 0.550 |
| The first group a - the third group c | 948.42 | 112.09 | 1.67, 46.87 | 236.92 | 0.001 | 0.894 |
| The second group b - the fourth group d | 905.09 | 145.42 | 1.81, 50.68 | 174.27 | 0.001 | 0.862 |
| The third group c - the fourth group d | 0.42 | 33.53 | 1.68, 46.50 | 0.35 | 0.664 | 0.012 |
Pairwise Comparison of the Interactive Effect of Group × Time on Insomnia
5. Discussion
The study results indicated that the KiSS program was effective in the improvement of insomnia in children of 8 - 10 years, and the changes made in the follow-up phase remained stable. The results of this study in the posttest and follow-up phases are consistent with the results Ma et al. (10), Schlarb et al. (16), Paine and Gradisar (17), Bromandnia (33), de Bruin et al. (34), and Meltzer and Mindell (35). The researchers stated that CBT-I could improve insomnia in neonates, children, adolescents, and adults.
For explaining the study results, it can be stated that the simultaneous application of educational, behavioral, and cognitive strategies in the KiSS program protocol with parental participation in sessions and the existence of therapy puppet to teach strategies to children with reducing physiological and cognitive arousal and perpetuating factors has led to the improvement of insomnia in children. Therefore, using the sleep education strategy has been effective in understanding normal sleep patterns as well as having rational expectations about sleep. Additionally, the sleep health education strategy in this protocol has been effective with changes in the child’s lifestyle such as managing caffeine consumption, quiet physical activity, no use of electronic media an hour of bedtime to minimize sleep problems and insomnia consequences. Bedtime routines and rituals also offer predictable cues and familiarity and effective in establishing the optimal environment to eliminate alertness and relaxation, which are both prerequisites for a smooth transition from waking up to sleep (13).
Furthermore, sleep restriction method increases the homeostatic pressure for sleep (36). Also, the instructions of stimulus control method such as establish a consistent sleep-wake rhythm, modification of sleep environment, use the bed just to sleep cause rapid sleep onset (15), and the feeling of satisfaction created in the child and parents leads to continued appropriate behavior.
In addition to the above-mentioned issues, using two techniques of charging magic spots and Kalimba magic-breathing technique led to relaxation by reducing physical tension and physiological arousal. Cognitive techniques of reviewing daily events and using the worry box also help the child cope with dysfunctional thoughts, night worries, and sleep-related anxieties and overcome the perpetuating factors of insomnia (14). Also, according to hypnotic susceptibility at the age of 7 to 14 years, through hypnotherapy presented by Kalimba (15), the children with travel to a magic land and perform the tasks presented were prepared to sleep. It should be noted that parents and therapists during the sessions by reward system elevate the child’s motivation toward coping with insomnia. Receiving a certificate for participation in treatment sessions has also increased the child’s motivation toward coping with insomnia and follow the principles of this protocol even after the end of treatment sessions. Therefore, the use of the aforementioned strategies has played a significant role in the improvement of insomnia (14).
The results of mixed-design ANOVA analysis showed that reflexotherapy also reduced the mean scores of insomnia in the posttest stage. However, the changes were not stable, and the effectiveness of this treatment decreased in the two-month follow-up. Although no study has evaluated the effectiveness of reflexotherapy in insomnia among children to date, the results of this study in the posttest phase are consistent with the results of Huang et al. (23), Farrokhian et al. (37), Gong et al. (38), Hughes et al. (39) and Nasiri et al. (40) in the follow-up phase are different from the study results of Hughes et al. due to the different follow-up time. The researchers concluded that reflexology or foot reflexology massage is effective in the improvement of insomnia in adults and the elderly.
In explaining the effectiveness of reflexotherapy in insomnia among children, it can be stated that in this treatment, applying pressure on the reflex points of insomnia for a specified time by causing a reaction in the body has led to the improvement of insomnia in children. According to the theory of nerve impulses, the stimulation of the reflex points related to each disorder leads to the regulation of the function of these points by increasing the nervous connections and transmitting the nerve impulses (23). Therefore, it can be explained that by stimulating the reflex points of the brain, brainstem, and transmission of nerve impulses to these areas, the cerebral cortex is stimulated first, and rituals and habits associated with sleep onset are influenced by cortical activity. These habits establish a relaxed and habitual situation making physiologic sleep onset mechanisms perform their function (5).
Also due to the role of the nuclei of the brainstem network system in control the sleep-wakefulness mechanism (41), the stimulation of the reflex point of the brainstem is important in insomnia improvement (3).
Moreover, the stimulation of the hypothalamus reflex points also leads sleep onset, NREM sleep control and regulates the circadian rhythm of sleep and wakefulness in that plays an important role in the treatment of insomnia (42). Some also believe that the stimulation of the aforementioned reflex points by changing the activity of brain waves, leads to sleepiness and sleep (N1 and N2 NREM sleep) with a feeling of deep relaxation (22). It is noteworthy that the aforementioned reflex points are the same areas that are mentioned in the neurobiological model of insomnia to explain the causes of insomnia (43).
In addition to the reflex points of the brain, brainstem and hypothalamus, the stimulation of the pituitary gland by balancing the function of the endocrine system, pineal reflex point by increasing melatonin secretion, and stimulation of the reflex point of the adrenal gland by decreasing of cortisol levels and anxiety before going to bed, leads to the improvement of this disorder in children.
The stimulation of the reflex points of the thoracic spine, diaphragm and solar plexus also leads to the treatment of insomnia by increasing the parasympathetic system activity (30), relaxation and overcoming the reactions of fear and anxiety before sleep (44).
Some also believe that increase in the secretion of endorphins by stimulating the pituitary and hypothalamic reflex points during treatment sessions and reduction of muscle tension contribute to better relaxation and sleep (45).
In addition to the above-mentioned issues, reflexotherapy also has improved insomnia by creating physical reactions. One of the most important reactions is the feeling of sleepiness and change in sleep patterns occurring during or at the end of the treatment session due to tension reduction, feeling of well-being, deep relaxation, and pleasant warmth created in the body. Consequently, the individual frequently falls asleep and awakens a short time later, much refreshed. In this way, after the reflexotherapy sessions, the clients sleep more and deeper.
Moreover, reflexotherapy, in addition to removing the blockage of zones, balancing the energy flow with improvement in nutrition of tissues and cells, and cleansing of the body toxins through the increase of perspiration and urine leads to the restoring of homeostasis and strengthening the immune system (21); therefore, the energy of the healing power children’s body leads to the improvement of insomnia (18).
Finally, the findings of the present study indicated that there was a difference between the effectiveness of the KiSS program and reflexotherapy in insomnia among children of 8 - 10 years; accordingly, despite the effectiveness of both treatments in the posttest phase, the effectiveness of the reflexotherapy intervention is temporary, and after 2 months of follow-up, the insomnia reappear in children. Therefore, it can be concluded that the KiSS program effects is similar to that of other CBT-I protocol.
However, due to the fact that in order to use this method, children and their parents need to participate in treatment sessions, and some parents and children want to accept a procedure that is administered on them rather than the involvement in the therapeutic process (3), James’s reflexotherapy protocol can also be used as an uncomplicated, safe, and cost-effective nonpharmacological intervention the effects of which appear from the first treatment session to treat pediatric insomnia. However, the effects of this method are not stable similar to those of the pharmacological therapy, and when it is stopped, insomnia disorder reappears after 2 months. To explain the difference between the results of these two treatments, we can point to the role of physiological, cognitive and emotional arousal in the development of insomnia. Because CBT-I, unlike reflexotherapy, targets all types of arousal, which play a very effective role in causing insomnia (46, 47).
5.1. Limitations
One of the most important limitations of this study was the small sample size due to the coronavirus disease pandemic, which makes it difficult to generalize the results. In addition, despite the breadth and comprehensiveness of studies related to insomnia, a limited number of studies have been performed on the effectiveness of the KiSS program and reflexotherapy in insomnia in children, which has limited the possibility of comparing the results.
5.2. Conclusions
Both the KiSS program and reflexotherapy can be used as uncomplicated and safe nondrug interventions to improve insomnia in children of 8 - 10 years. Nevertheless, the KiSS program showed more promising results.