1. Background
Aging is a gradual and inner biological process occurring in all living creatures and affecting numerous cells, tissues, organs, and body systems to a great extent. As a result of these changes, the well-being and health of a person may decline, but aging is not considered an illness at all (1). With improved financial and social situations and the development of hygiene standards, mortality rates and stillbirths have decreased, and life expectancy has increased in societies. Consequently, the population pyramid has evolved, and the mean age of the population and the share of older adults in the population have also increased (2). According to the statistics provided by the World Health Organization (WHO), the number of people aged 60 years or older will change from 12% in 2015 to 22% in 2050 worldwide (3).
The population of older adults in Iran has also been estimated to grow from 5.4% in 1975 to 10.5% in 2025. Based on the latest census by the Statistical Center of Iran (SCI), the number of people aged 60 years or older has been increased by 9.27% (4).
It is probable that through aging, different problems and diseases in physical and mental aspects will arise in older adults, the most important of which include sleeping disorders (5). Sleep is one of the most fundamental needs of humans, and according to the research, the third critical problem faced by older adults is the low quality of sleep. As this affects all aspects of life, it should concern those providing health services (6). Enough sleep and rest influence physical and emotional health. Epinephrine and serotonin are produced during sleep, chemical reactions occur, and cell nourishment is increased to prepare the body for daily activities by reclaiming energy. In addition, recovery of memory and learning to reduce anxiety, stress, and tension happen during sleep. Without proper sleep and rest, the ability to focus, judge, and perform mental activities is decreased, and the mood and behavior of the person change. Recent studies have shown that in the short term, lack of sleep can lead to disorders, such as low glucose, high blood pressure, an increase in cortisol levels, and an increase in sympathetic nervous system function (7, 8).
As the longevity of human life grows, the focus on promoting quality of life leads to the necessity for increasing efforts in detecting and treating sleeping disorders in older adults (9). Older adults have a low sleep quality, and there is a close relationship between sleep quality and the quality of life. Sleep quality should be continued by ensuring sleep hygiene among older adults; thus, the quality of life should be increased (10). Treatment of sleep problems and disorders can improve older adults' quality of life and daytime functioning (11).
Complaints about sleeping disorders in older adults are common, which might be connected to different physical, mental, and environmental factors; however, this matter is generally a multifactor issue in older adults. The most common and critical sleeping disorders in older adults are insomnia, sleep apnea, restless leg syndrome, rapid eye movement- sleep behavior disorder, and delayed sleep phase syndrome (12). The issues related to sleep in older adults have significant negative effects on people's lives. They might result in daytime sleepiness, depression, falling, memory and attention dysfunction, problems in concentration, irritability, dementia, tiredness, unstable temperament, anxiety, and overuse of sleeping medications (13, 14).
One of the non-medicinal methods that can be effective is called Emotional Freedom Techniques (EFT). This technique, consisting of tapping and cognitive therapy, can be used either by a trainer or by people themselves (15). In different studies, this technique has been used to treat various psychological disorders, such as anxiety, depression, phobias, and post-traumatic stress disorder (PTSD), and different physical disorders like headaches, pain, brain injury, fibromyalgia, psoriasis, and seizures (16, 17). Physiological evaluations have shown that this technique has affected controlling cortisol levels and positive changes in gene expression, nerve plasticity, balancing inflammations and immunity response, destroying tumors, and controlling the autonomic nervous system (18, 19).
Medicinal treatments and non-medicinal treatment methods, such as sleep hygiene, stimulus control, limited sleep, relaxation, and cognitive behavioral therapy, could be used to manage difficulties in low-quality sleep. These methods may suit various sleeping disorders (12, 20). In managing and treating sleeping disorders, most studies carried out have been based on sleep hygiene methods (21), logotherapy (22), medicinal therapy and acupuncture (23), regular moderate physical activity (24), hydrotherapy (25), cognitive behavioral therapy and tai chi (26, 27) and limited research has been done in the field of emotional freedom techniques (28, 29). Thus, the EFT method is a relatively simple, new, and, more importantly, probably non-invasive method without side effects. It is possible for individuals to practice this technique alone at home without incurring any additional expenses and with minimal time commitment.
2. Objectives
As the population of older adults and the problems related to low quality of sleep in this age group have increased, many studies have been carried out in Iran and around the world using different treatment methods; therefore, this study was done to investigate the effect of this method on managing the quality of sleep in older adults.
3. Methods
3.1. Participants
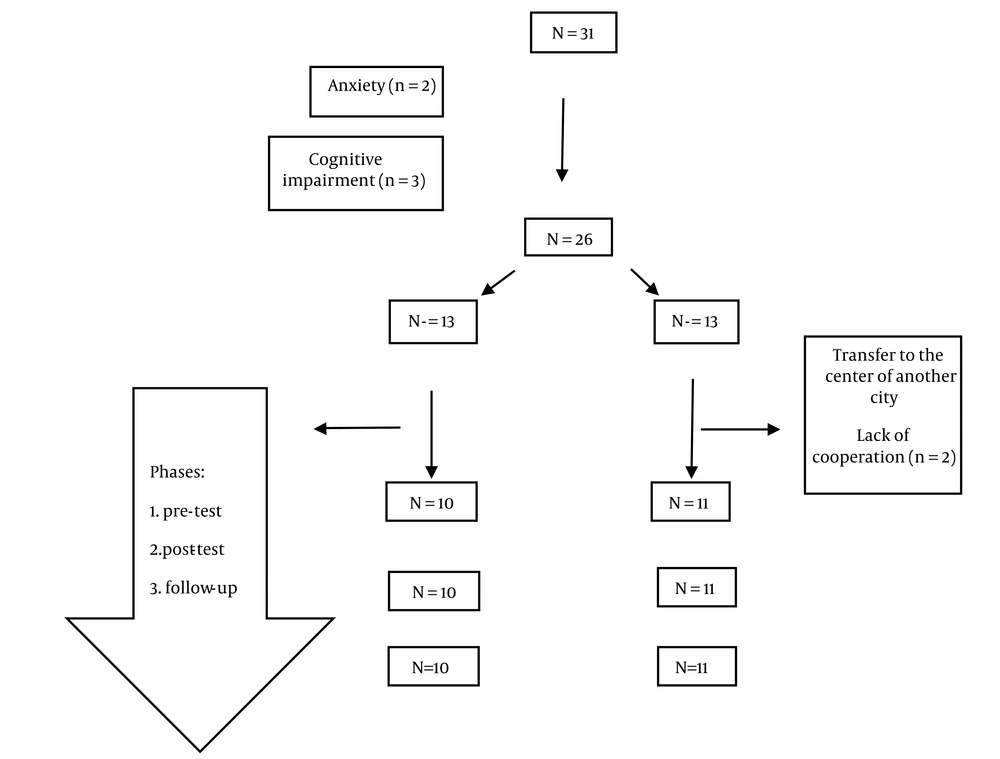
This study's target group included the elderly at the Hamrah Salamat Day-Care Center of Babol, Babol County, Mazandaran Province, north of Iran. Inclusion criteria were having 60 years and older, a Pittsburgh Sleep Quality Index (PSQI) score of more than 5 or a sleepiness score of more than 10, and giving informed consent. Afterward, questionnaires for anxiety, depression, and cognition were filled out for them. Those with impaired cognition or extreme hearing loss, along with those elderlies with severe anxiety or depression who were under treatment, had drug problems, or did not tend to participate, were excluded from the study. The list of all medications they used was evaluated, and if they affected sleep, they were controlled during analysis through statistical methods, such as regression. The selection was based on the Pass software and the article's information, with a mean value of 11.88, a standard deviation of 2.538 in two intervention and control groups, and a power of 95%. Ten samples in each group were estimated, too. The convenience sampling method and according to the study's inclusion criteria, 21 people participated and were divided into two groups: intervention and control. (Figure 1)
3.2. Measures
The demographic variables assessed in this study were age, sex, level of education, marital status, and evaluating the list of medications.
3.2.1. The Sleep Quality Index
The PSQI was used to investigate the sleep quality of older adults in the past month. This index was created by Buysse et al. at the Pittsburgh Psychoanalytic Center. Its validity (86.5) and reliability (89.5) were tested in Iran in 2009 in a study by Shahri Far (30, 31). This index has 9 components, but as question No.5 has 10 sub-components, the index has 19 items, scored on a four-point Likert scale from 0 to 3. This index has 7 sub-scales, including subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleeping disorders, the use of sleeping medications, and daily functionality disorders. Getting a score higher than 5 on the index means poor sleep quality.
3.2.2. The Epworth Sleepiness Scale
The validity of this scale has been reported in the study by Masoudzadeh et al., based on the content, and its reliability has been assessed using Cronbach’s Alpha (0.70) (32). This scale has been designed to assess sleepiness. In ESS (Epworth Sleepiness Scale), individuals rate their sleepiness in 8 daily situations from 0 (I do not take a nap) to 3 (I probably take a nap). The overall score of ESS is calculated by summing scores of all 8 questions, which can range from 0 to 24. The final score of ESS ranging from 0 - 8 shows natural sleepiness, 9 - 12 shows mild sleepiness, 13 - 16 means moderate sleepiness, and a score higher than 16 indicates severe sleepiness. An ESS score of above 10 is clinically considered significant and indicates sleepiness.
3.2.3. Geriatric Anxiety Inventory
In 2007, Pachana composed an inventory of 20 parts to evaluate anxiety symptoms in the elderly. This inventory has 20 components (with two-option answers of yes and no) and three dimensions, including cognitive (11 components), motivational (5 components), and physical (4 components) dimensions. Bandari et al., in a study, normalized this inventory (Cronbach’s alpha of 0.957) in Iran (33, 34). A score of 9 or higher shows that the individual has anxiety.
3.2.4. The Geriatric Depression Scale
The 15-question outline of this questionnaire was designed by Marc et al. and normalized by Malakouti et al. in Iran. The results of the tests showed agreeable reliability ratios. Cronbach’s Alpha of 0.9 and test-retest reliability of 0.58 were obtained (35, 36). This questionnaire has 15 items, including yes-no questions. Each answer is graded with 0 and 1, and based on the results, the patients can be divided into four groups (0 - 4 normal, 5 - 8 mild depression, 9 - 11 moderate depression, and 12 - 15 severe depression). Individuals with a score of 5 or higher are declared as depressed.
3.2.5. Quality of Life in Older Adults
This questionnaire was constructed by Hyde et al. in England based on the compensating needs model. It was normalized by Heravi-Karimooi et al. in Iran (Cronbach’s alpha of 0.97). The exclusive questionnaire for assessment of quality of life in older adults (CASP-19) is the most commonly used instrument for evaluating quality of life in older adults (37, 38). The questionnaire mentioned has 19 dimensions: control, autonomy, self-realization, and pleasure. The control dimension has 4 phrases, the autonomy dimension has 5 phrases, the self-realization dimension has 5 phrases, and the pleasure dimension has 5 phrases. These items are rated on a Likert-type scale with 4 options ranging from “most of the time” to “never”. The lowest score for each phrase is “zero,” and the highest is “three”. Scoring for 6 phrases (including items 1, 2, 4, 6, 8, and 9) is opposite. The maximum score reported for the questionnaire is equal to 57 (complete satisfaction in all 4 dimensions), and the minimum score is equal to zero (the total lack of satisfaction in quality of life).
3.2.6. The Abbreviated Mental Test Score
This test was originally formed by Roth and Hodkinson in 1972 to evaluate orientation and memory in hospitalized older adults. The validity and reliability were tested by Foroughan et al. (39-41). This form is an abbreviated form of the MTS mental test consisting of 10 questions, and for each correct answer, one point is given, and it only takes 3 minutes to complete the test. Another benefit of this test is that it can be filled out for illiterate individuals. If people obtain a score of 6 or lower, they have a cognitive disorder.
3.3. Procedure
Sleep quality in older adults was assessed by the PSQI, and sleepiness quantity was evaluated by the ESS. The other materials used in this study were GDS (Geriatric Depression Scale) related to depression, GAI (Geriatric Anxiety Inventory) related to anxiety, AMTS (Abbreviated Mental Test Score) related to cognitive disorder, and CASP-19 questionnaire related to the quality of life of older adults.
In the next step, after the interventions, sleep quality, sleepiness, and quality of life of the elderly were re-evaluated by filling out the questionnaires. Also, a month after the intervention, a re-evaluation was done for re-assessing the participants and evaluating the effects of the interventions. The results were analyzed using SPSS version 23, statistical analysis software.
3.4. Treatment Interventions
3.4.1. The Procedure of the EFT Method
In this method, some points of the body, which are also used in acupuncture and deep pressure therapy (DPT), are tapped with the tips of the fingers. Before administrating this method, some sentences, known as corrective and reminder sentences, focus on the person's problems. In corrective sentences, the people declare that despite having problems, they love and accept themselves. Still, in reminder sentences, the people focus on their problem, try to change their cognition somehow, and bring forth the problems from deeper layers of their mind to surface and neutralize them by voicing them and simultaneously tapping. While tapping the points, they replace them with the right beliefs. The number of points on the body that are tapped consists of 9 different parts of the body: the external part of the hands, top of the head, tip of the eyebrow, end of the eyebrow or outer corner of the eye, under the eye, under the nose, under the lips or chin, collarbone, and armpit (42). The time of the intervention was in the morning, and there was no time limit or repetition of the intervention by people at home.
Before beginning sessions, the participants were asked about the severity of their problems. They gave a score between 0 - 10 depending on their problem's severity, which was repeated at the end of each session. The severity of the problem is usually decreased. In the first session, the sentences presented to older adults were about familiarizing them with this method, encouraging them to participate in sessions, and accepting it. In the first round, wrong beliefs about an issue were declared, and in the next round, the goal was to replace negative beliefs with positive ones or, in other words, eliminate them. From the second session to the eighth, sentences related to sleeping problems, concerns, fears, and even bad memories were recounted.
Teaching sleep hygiene and general guidelines for keeping a natural rhythm of sleep and wakefulness consist of these suggestions: keeping regular sleeping and waking hours, eating light meals before going to bed, regular exercise, writing worrying thoughts and attending to them in the next day, keeping the bedroom cool, dark, and quiet, not taking a nap during the day, not watching TV in bed, not drinking coffee, smoking, and drinking before going to bed (43).
4. Results
According to Table 1, the participants of this study were all older female adults aged between 64 - 79 years old, with a mean age of 70.86 ± 3.812 years old. The mean age in the intervention group was 71.09 ± 1.814 years old, and in the control group, it was 70.60 ± 5.337 years old (P: 0.787). The chi-Square test was used to compare the frequency of data regarding age, marital status, and level of education between the two groups. The highest frequency in the intervention and control groups belonged to those aged between 60 - 75 years old. Regarding marital status, the number of married and widowed participants was the same in the intervention group. Still, in the control group, more people were widowed. Also, primary education had the most frequency in both groups.
| Variables | Intervention Group, No. (%) | Control Group, No. (%) | P-Value a |
|---|---|---|---|
| Age | 0.787 | ||
| 60 - 75 | 11 (100) | 8 (80) | |
| Above 75 | 0 (0) | 2 (20) | |
| Marital status | 0.561 | ||
| Married | 5 (45.5) | 4 (40.0) | |
| Single | 0 (0) | 0 (0) | |
| Widowed | 5 (45.5) | 6 (60.0) | |
| Divorced | 1 (9.1) | 0 (0) | |
| Level of education | 0.682 | ||
| Illiterate | 0 (0) | 1 (10.0) | |
| Primary | 6 (54.5) | 6 (60.0) | |
| Middle school | 2 (18.2) | 1 (10.0) | |
| Diploma | 2 (18.2) | 2 (20.0) | |
| Higher education | 1 (9.1) | 0 (0) |
a Chi-square test (P < 0.05).
As seen in Table 2, there was a decrease in average sleepiness and PSQI and an increase in the average quality of life in the repeated-measures test conducted on each control and intervention group, meaning there has been progress in both groups.
| Pre-test (Mean ± SD) | Post-test (Mean ± SD) | Follow-up (Mean ± SD) | |
|---|---|---|---|
| Sleep quality (PSQI) | |||
| Intervention group | 10.55 (2.770) | 7.45 (2.464) | 6.00 (2.646) |
| Control group | 11.30 (2.791) | 8.80 (3.293) | 6.60 (2.413) |
| Sleepiness (ESS) | |||
| Intervention group | 8.82 (2.786) | 6.64 (3.107) | 5.00 (2.145) |
| Control group | 8.20 (2.201) | 5.70 (2.359) | 5.10 (2.234) |
| Quality of life (CASP) | |||
| Intervention group | 44.09 (6.774) | 46.09 (5.839) | 47.64 (5.353) |
| Control group | 38.40 (7.121) | 38.50 (6.654) | 39.70 (6.147) |
A repeated-measures analysis of variance (ANOVA) with Time (pretest, posttest, and follow-up) and groups (intervention and control) effects was performed to see if there were any interactions between time and groups. Results showed that there were no significant interaction effects for any subscale, including subjective sleep quality (P = 0.786), sleepiness (P = 0.568), and quality of life (P = 0.289). Therefore, these findings indicated that the intervention was not effective.
A repeated-measures analysis of variance (ANOVA) was conducted, examining the effect of time for each group separately to evaluate their changes over time on the subscales of sleep quality, sleepiness, and quality of life. The resulting F-statistic and P-value for the time effect separately for each intervention and control group were provided in Tables 3 - 4 - 5.
Time effects were statistically significant for the two groups and for sleep quality and sleepiness (P < 0.05).
| PSQI | Type III Sum of Squares | df | Mean Square | F | Sig. a |
|---|---|---|---|---|---|
| Time | 227.145 | 2 | 113.573 | 34.021 | 0.001 |
| Time × group | 1.622 | 2 | 0.811 | 0.243 | 0.786 |
| Error (time) | 126.855 | 38 | 3.338 |
a Repeated-measures test (P < 0.05)
| ESS | Type III Sum of Squares | df | Mean Square | F | Sig. a |
|---|---|---|---|---|---|
| Time | 130.572 | 1.177 | 110.939 | 17.569 | 0.001 |
| Time × group | 2.953 | 1.177 | 2.509 | 0.397 | 0.568 |
| Error (time) | 141.206 | 22.362 | 6.314 |
a Repeated-measures test (P < 0.05)
| CASP | Type III Sum of Squares | df | Mean Square | F | Sig. a |
|---|---|---|---|---|---|
| Time | 61.855 | 1.162 | 53.225 | 4.938 | 0.032 |
| Time × group | 15.315 | 1.162 | 13.178 | 1.223 | 0.289 |
| Error (time) | 238.018 | 22.081 | 10.780 |
a Repeated-measures test (P < 0.05)
5. Discussion
The main objective of this research was to determine the effect of EFT on sleep quality in older adults. In determining the effect of this technique on the sleep quality of older adults in the adult day-care center and comparing the two intervention and control groups, the analyses indicated no significant difference between the study groups in the pretest, posttest, and follow-up. However, both groups had a positive, progressive trend in sleep quality. These methods clinically improved the sleep quality of older adults. Since older adults may be emotionally instable, on this basis, the effect of encountering a therapist can lead to clinical improvement in two groups. Considering that the follow-up was done only one month after the end of the intervention and in some studies, the follow-up was done in 3 and 6 months or even more, also because the EFT possibly has more effect in the long term, the expected result is not achieved.
Also, considering the relatively equal effect of the two methods in increasing the sleep quality of the elderly, both can be used to improve the sleep quality.
In terms of the effect of EFT on the sleepiness of the older adults in the adult day-care center, no significant difference was observed between the intervention and control groups, demonstrating this technique's ineffectiveness. However, both groups' processes were significantly positive, and improvement was made.
This indicates that EFT could not lead to the expected effect. In a similar study, Lee et al. employed this method to assess the severity of insomnia and observed its positive effect, which is inconsistent with our results (29). Of course, in the present study, the variable under study was sleep quality, sleepiness, and mean age of the participants, showing the difference between the studied variable and the tools used and the 10-year lower mean age of participants, which can be a reason for achieving different results.
With regards to determining the effect of EFT on the quality of life of older adults at the adult day-care center and also comparing the two groups, by analyzing the associated data with this variable and according to the different mean of pretest and follow-up, it can be concluded that both groups had progress in the process. Still, neither method had positive and significant effects on the older adults in the two groups, but the quality of life clinically improved. These two groups also did not have any significant difference from one another in the pretest and follow-up. Thus, EFT did not positively affect quality of life either. Research carried out by Niken et al. in Indonesia addressed the effect of spiritual and emotional freedom techniques (SEFT) on the pain experienced by cancer patients. In this study, after employing this method and reducing the participants' pain, their quality of life improved (44). In this research, the number of participants and people under intervention was different from our research, and SEFT (in which there are a greater number of points used for tapping and the sentences are different) was used as the intervention method. Due to the increased points tapped in this method and the longer period needed to perform it, and also keeping in mind the limited tolerance and patience of older adults, this method was not employed.
5.1. Conclusions
The results of the study indicated that the EFT was not effective on sleep quality, sleepiness, and quality of life in older adults, but due to the process of improving the mean of these variables at the times of before up to one month after the intervention, there were clinical benefits. Due to the importance of using a simple technique to treat the disease of sleep quality and its effects on all aspects of older adults' lives, it is advisable to conduct a study with a larger sample size that replicates the findings.
5.2. Limitations of the Study
The results of our research may have been influenced by the absence of random allocation. Also, the elderly present at adult day-care centers were mainly women, and the study's results cannot be generalized to both sexes due to the absence of male participants. Therefore, it is recommended that future studies be conducted on a larger and more diverse sample size, including both sexes, and conducted under favorable conditions. Support for conducting more research in this field is also essential.