1. Background
Schizophrenia spectrum disorders (SSD) are characterized by psychotic symptoms (1) and emotional dysregulation (2). According to Cohen and Minor (3), negative emotions in patients with schizophrenia are associated with psychotic symptoms (4) and poor quality of life (5) and contribute to the formation and persistence of psychotic symptoms (6). The prevalence of SSD is approximately 3.5% in the general population (7), and the associated hospitalization rate is estimated at 25 to 38% (8).
Schizophrenia is one of the top ten causes of disability worldwide and is recognized as the most debilitating psychiatric disorder (9, 10). Frequent hospitalization in the acute phase of the disease increases the economic burden of SSD patients (11). Reduction of recurrence and prevention of readmission are among the treatment priorities for patients with Psychosis (12). The prevalence of SSD ranges from 05% and 0.6 to 0.89% in Iran, according to diagnostic criteria (13, 14), while Rahimi-Movaghar et al. reported a prevalence rate of 1% (15). Considering the population of Iran (over 86 million people), statistically, 765,400 people may suffer from psychotic symptom (16), which indicates the importance of psychological interventions.
The outcomes of medication use are often poor (17) and sometime maybe harmful for SSD patients (18), because clinically, they do not improve the patients’ cognitive symptoms significantly, and approximately 50% of patients do not respond to medications (19). Many therapies have been practiced for psychosis, such as psychoanalytic-psychodynamic therapy, systematic therapy, cognitive-behavioral therapy and its derivatives, combined approaches, and supportive psychotherapy (20) but the acceptance and commitment therapy (ACT) is a promising approach for filling this therapeutic gap for patients with psychiatric disorders (21). Although ACT has significant effects on the believability of auditory hallucinations, the impact of this approach on negative symptoms, delusional beliefs, and duration of therapeutic effects is unclear (22). For instance, White et al. used the ACT application along with TAU with a three-month follow-up for after psychosis emotional malfunctions in a randomized trial study. Minor progression in negative symptoms and considerable growth of improvement in mindfulness skills (23) were the outcomes of this therapy. Cramer et al. demonstrated that interventions based on short-period mindfulness, such as the ACT, have positive, but short effects on improvement of positive symptoms, duration of hospitalization, and concentration. They also are effective in supportive therapy for those suffering from psychosis (24). In a research called “ACT” and in an AB single-case study for hospitalized patients with psychosis, Larsson et al. (25) mentioned that this type of therapy is practical for them and can noticeably affect their quality of life. Furthermore, the patients themselves found ACT valuable.
For psychosis, ACT is commonly implemented in groups (26, 27). The less frequent use of single-case programs in psychiatry is due to a lack of knowledge of their practical value, not their usefulness (28). Accordingly, there are scares single-case studies on patients with SSD, and only one patient has been examined in some of these studies. Single-case studies are valuable for diagnosis, especially for psychiatric disorders (29), as well as development of appropriate therapies (30). Besides, ACT protocols for psychosis are still in their infancy and need to be revised (26). Khoury and Lecomte suggested performing ACT in at least eight sessions for inpatient with psychosis (31) and some experts suggested four sessions of the therapy (32), while in the present study, ACT was performed as a single-case intervention in 15 sessions for the following reasons: cost-effectiveness and assistance in the management of treatment costs in single-case projects for examining behavioral or educational interventions, besides the flexibility of single-case projects in different situations (33); assessment of the sustainability of intervention effects (34); and the limited number of single-case studies compared to group studies (27).
Although the effectiveness of ACT in reducing anxiety, believability of symptoms, and readmission has been investigated and its advantages have been observed in improving emotional symptoms, the reducing social damages, and distress related to hallucination (35), focusing on the emotional component and its role in maintaining psychotic symptoms is an important issue that should not be overlooked. Moreover, people with SSD may experience a recurrence of psychotic symptoms and emotional maladaptation throughout their lives. However, no study has been carried out to determine how people with SSD can move toward their life values through the ACT process following the alleviation of psychotic symptoms, improvement of emotion regulation, and reduction of psychotic symptoms.
2. Objectives
Considering the contradictions in the findings reported in the literature and the assumption that ACT is effective in correcting an individual’s perception of psychotic experiences and emotional dysregulation, this study aimed to determine the effectiveness of ACT on positive and negative psychotic symptoms and emotion regulation in patients with SSD.
3. Methods
3.1. Research Design
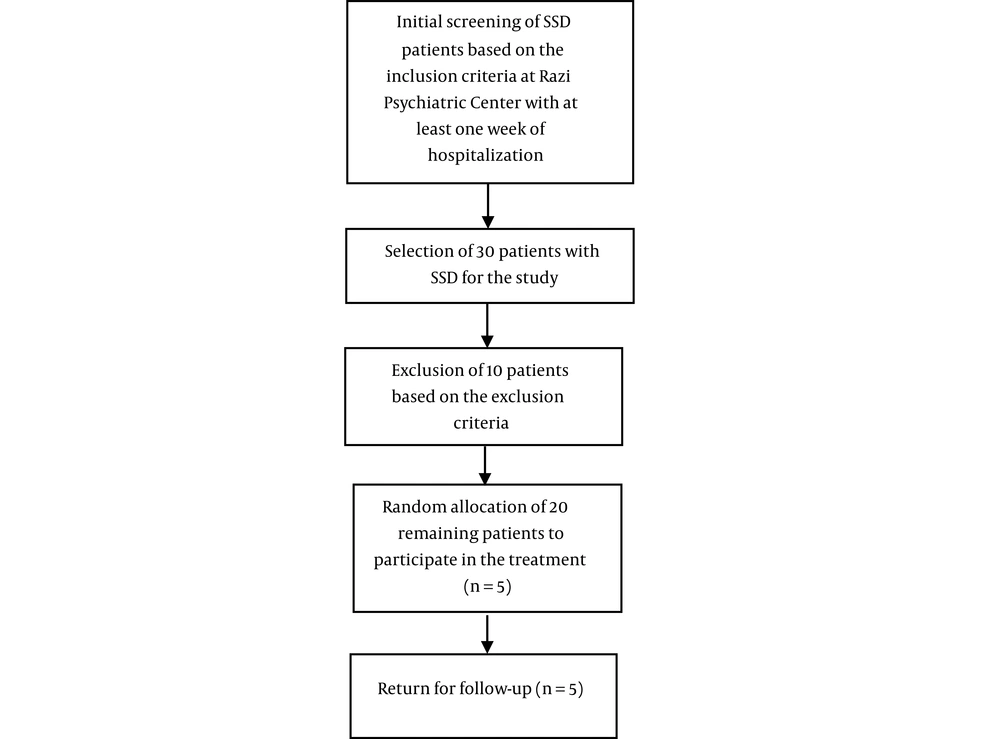
The experimental design of this AB single-case study included a follow-up phase, the initial sampling was accessible and without blinding. The statistical population consisted of all SSD patients, admitted to Razi Educational and Therapeutic Psychiatric Center in Tehran, Iran, in 2021. At the beginning, thirty patient were chosen accessibly for the research. Afterwards, 10 people were excluded due to the exclusion criteria. Among the 20 participants who had inclusion criteria to the study, five participant (three men and two women in the age range of 32 - 43 years) were randomly allocated to participate in the intervention through drawing. (Figures 1 and 2)
The sample in the present study was determined according to the minimum sample size required to confirm or reject research hypotheses in single-case designs. According to Horner and Odom (36), single-case designs could potentially provide a minimum number of intervention effects (i.e., changes between the baseline and intervention periods) if only three series were implemented. Nevertheless, they recommended that considering four series was better because conducting the study might face some problems (e.g., a participant may move to another city, or they may be hospitalized in other medical centers and need to be eliminated from the study). Thus, the sample size was determined at five participants.
The present article was extracted from a doctoral dissertation in rehabilitation counseling, approved by the Ethics Committee of Tehran University of Rehabilitation Sciences and Social Health (IR.UWSR.REC.1399.013). The present study was also registered in the Iranian Registry of Clinical Trials (IRCT20210412050937N1) on 07/22/2021 and performed at Razi Educational and Therapeutic Psychiatric Center, Tehran, Iran.
3.2. Participants
The inclusion criteria were as follows: (1) patients who diagnosed with SSD according to the psychiatrist diagnosis; (2) relative control of acute symptoms (those whose impulsivity and aggression are controlled according to their psychiatrist); (3) age range of 18 - 45 years; (4) voluntary participation and written informed consent of the patient and his/her legal guardian based on codes of professional ethics in the clinical trial ; (5) minimum education of high-school diploma; (6) hospitalization for at least one week in the ward; and (7) scores > 90 on the Positive and Negative Syndrome Scale (PANSS) and > 120 on the Difficulties in Emotion Regulation Scale (DERS). On the other hand, the exclusion criteria, accompanied by the psychiatrist and with reference to psychiatric cases of the patients and the diagnostic criteria, were as follows: (1) having of criminal or judicial problems; (2) severe learning disabilities (Patients who struggle to read, write and reason, and also to recall or organize information, based on their first interviews); (3) neurological disorders (Such as epilepsy, multiple sclerosis (MS), Parkinson’s disease (PD), and Alzheimer’s disease); (4) high levels of disordered behaviors or high risk of suicide or homicide; and (5) diagnosis of mental retardation (mental function or intelligence is lower than the average of society and compromising or poorly adaptive behaviors)
3.3. Research Tools
The PANSS, which contains 30 questions, was developed in 1986 by Kay et al. to measure the severity of positive and negative psychotic symptoms in patients with SSD. The alpha coefficients of the original version of PANSS were 73% and 83% for the positive and negative symptom subscales and 79% for the general pathology subscales, respectively (37). The Cronbach’s alpha coefficient of this scale was estimated at 80% in Iran (38) and 77%, and its validity was reported to be acceptable based on factor analysis (39, 40).
Moreover, Gratz and Roemer developed DERS. The reliability of this scale was estimated at 88% based on test-retest, and its internal consistency was 93% based on Cronbach's alpha (41). The final version of DERS contains 36 items. Asgari et al. reported the reliability of the Persian version of this scale to be 86% and 80% based on Cronbach's alpha coefficient and bisection method, respectively (42), and Mazloom reported a Cronbach's alpha coefficient of 85% (43).
3.4. Intervention and Its Implementation
The research protocol was based on a book, entitled “acceptance and commitment therapy and mindfulness for psychosis” (44). The intervention sessions were held in the counseling rooms of Razi Educational and Therapeutic Psychiatric Center in Shafa 1, Shafa 2, and Mehr 1 wards. The main ACT topics in the sessions were as follows: treatment logic, acceptance strategies, failure, self-identity, mindfulness exercises, compassion, clarification of values, previous unsuccessful attempts to deal with the symptoms of psychosis, alleviation of experiential avoidance, and coping with emotional distortions.
To reduce acute psychotic symptoms, mindfulness exercises were performed for 15 minutes in each session. Due to cognitive problems, fewer metaphors and abstract contents were used. In addition to ACT, the participants received their routine treatment (Pharmacotherapy and psychiatric services that patients receive after hospitalization and with the order of psychiatrist) at the hospital. They received ACT in 15 sessions (45 minutes per session) over eight weeks (The duration of the intervention sessions was conducted during eight weeks) after stabilization with medications (Consistency of the drug effects on patients’ acute psychotic symptoms or beginning of the intervention sessions after controlling the acute psychotic symptoms according to the patient’s psychiatrist’s diagnosis) and completed the PANSS and DERS in three baseline sessions, five intervention sessions, and two follow-up sessions (one month and three months after the intervention, respectively).
3.5. Statistical Analysis
Statistical analysis was performed using SPSS version 16 and Microsoft Excel. The research hypothesis was evaluated via visual analysis of graphs, non-overlapping indices, and Cohen's d effect size. In single-case studies, Ferguson reported values of 0.41, 1.1, and 2.7 for small, medium, and large effect sizes, respectively (45).
4. Results
4.1. Characteristics of the Participants
In this study, five participant, with a mean age of 38.4 years, participated in the ACT (SD = 2.6) (Table 1).
| Participants | Age | Sex | Occupational Status | Marital Status | Education | Diagnosis |
|---|---|---|---|---|---|---|
| 1 | 42 | Female | Unemployed | Divorced | Diploma | Schizophrenia |
| 2 | 38 | Male | Employed | Single | Bachelor’s degree | Schizophrenia |
| 3 | 36 | Male | Non-governmental jobs | Married | Bachelor’s degree | Schizophrenia |
| 4 | 36 | Male | Non-governmental jobs | Single | Diploma | Schizophrenia |
| 5 | 40 | Female | Non-governmental jobs | Divorced | Diploma | Schizoaffective disorder |
The participants’ mean and median scores of PANSS and DERS were slightly lower in the intervention and follow-up phases compared to the baseline (Table 2).
| Participants | A | B | Follow-up | |||
|---|---|---|---|---|---|---|
| Mean ± SD | Median | Mean ± SD | Median | Mean ± SD | Median | |
| PANSS | ||||||
| 1 | 100.3 ± 3.06 | 101 | 91 ± 6.04 | 90 | 90.5 ± 4.9 | 90.5 |
| 2 | 108 ± 1 | 108 | 97 ± 6.8 | 95 | 93.5 ± 4.9 | 93.5 |
| 3 | 103.6 ± 1.5 | 104 | 101.6 ± 4.04 | 102 | 102 ± 4.2 | 102 |
| 4 | 110.3 ± 1.5 | 110 | 98 ± 3.5 | 97 | 97 ± 2.1 | 97.5 |
| 5 | 115 ± 1 | 115 | 103.4 ± 9.5 | 102 | 95.5 ± 2.1 | 95.5 |
| DERS | ||||||
| 1 | 136 ± 2 | 136 | 133.6 ± 2.9 | 134 | 126.5 ± 3.5 | 126.5 |
| 2 | 135.6 ± 1.1 | 135 | 127.2 ± 6.05 | 125 | 124.5 ± 2.1 | 124.5 |
| 3 | 132 ± 2.6 | 131 | 128 ± 2.5 | 128 | 130.5 ± 3.5 | 130.5 |
| 4 | 129.3 ± 1.1 | 130 | 120 ± 9.2 | 121 | 110 ± 5.6 | 110 |
| 5 | 135 ± 2 | 135 | 120 ± 6.5 | 118 | 122 ± 2.8 | 122 |
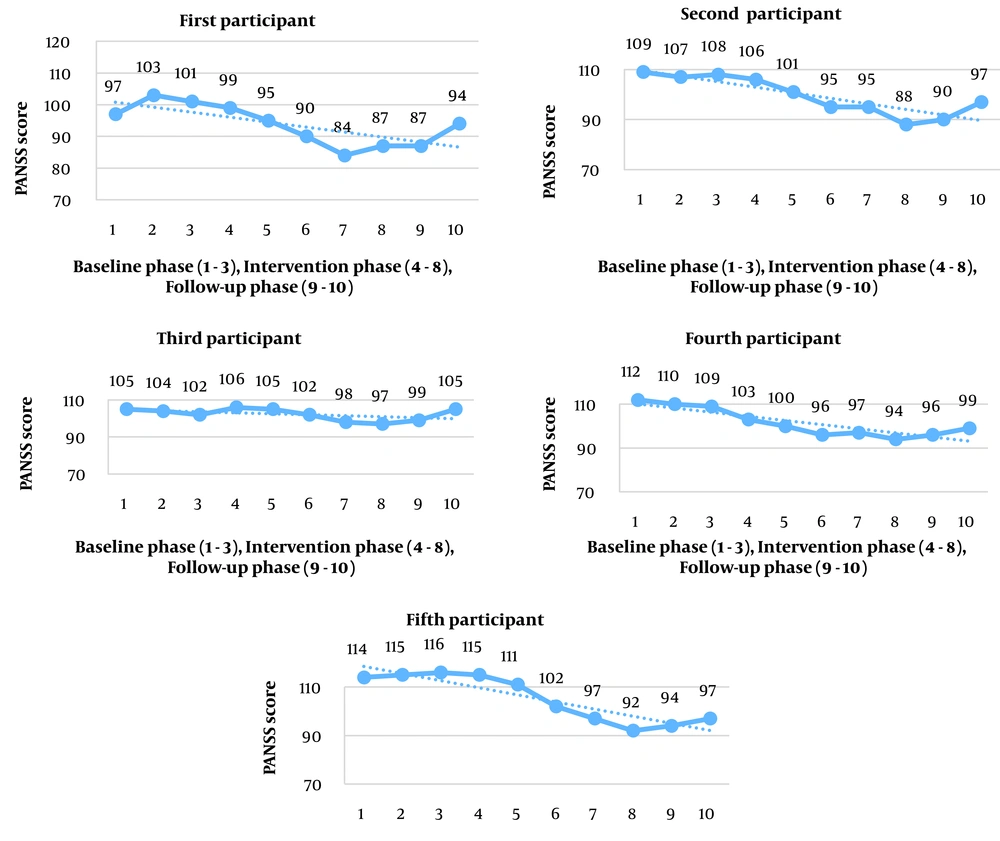
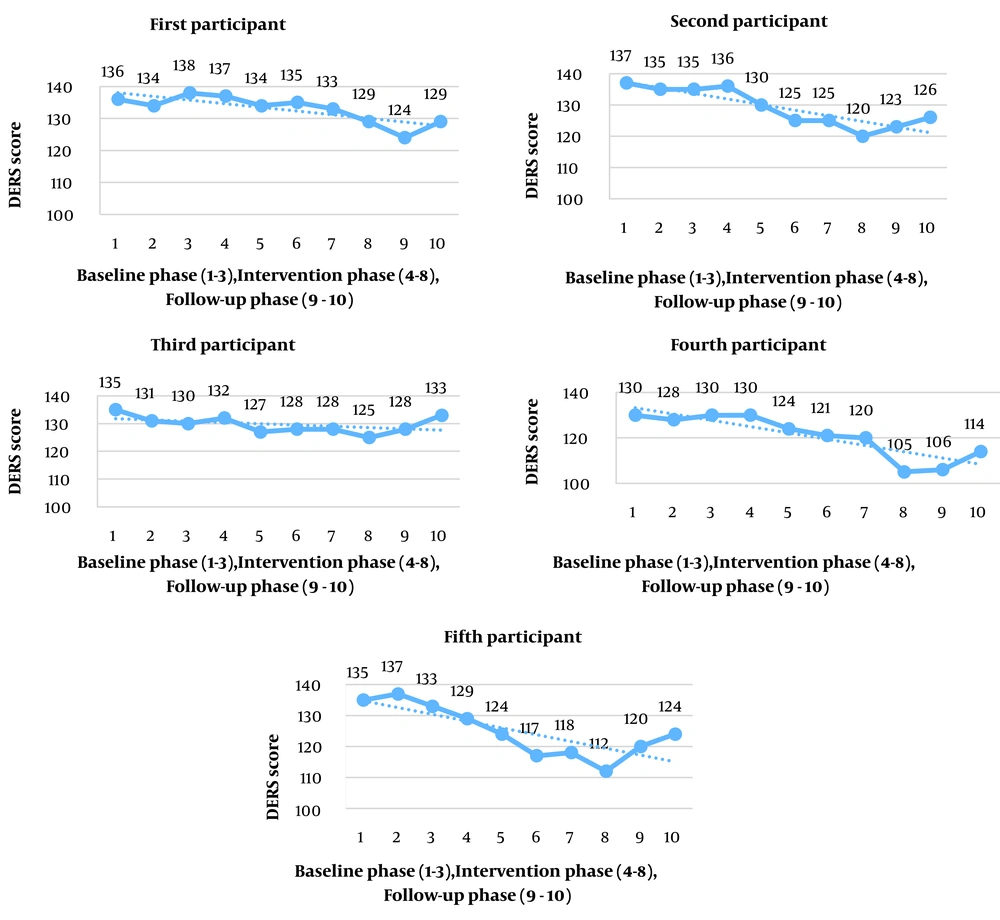
Figures 3 and 4 indicate the trend of changes in the participants’ scores in the baseline, intervention, and follow-up phases.
According to Figure 3, the slope of change for the first, second, third, and fifth participants was slight and descending, indicating a reduction in the PANSS and DERS scores and small changes. However, in the fourth participant, the slope of the line was downward and steep; in other words, change occurred at a greater speed and to a greater extent.
| Participant | NAP | PND | PAND | PEM | Cohen’s d Effect Size |
|---|---|---|---|---|---|
| PANSS | |||||
| 1 | 0.9 | 0.8 | 0.8 | 1 | 1.7 |
| 2 | 1 | 1 | 1 | 1 | 1.9 |
| 3 | 0.6 | 0.4 | 0.6 | 0.6 | 0.6 |
| 4 | 1 | 1 | 1 | 1 | 4 |
| 5 | 0.9 | 0.8 | 0.8 | 0.9 | 1.4 |
| DERS | |||||
| 1 | 0.7 | 0.4 | 0.7 | 0.8 | 0.8 |
| 2 | 0.8 | 0.8 | 0.8 | 0.8 | 1.6 |
| 3 | 0.8 | 0.8 | 0.8 | 0.8 | 1.5 |
| 4 | 0.8 | 0.8 | 0.8 | 0.9 | 1.2 |
| 5 | 1 | 1 | 1 | 1 | 2.7 |
According to Table 3, the non-overlapping indices for the third participant in PANSS and for the first participant in DERS were small and medium, respectively, with a slight overlap, which suggests the small effect of the intervention. The non-overlapping indices for other participants showed moderate to high effects in both scales, suggesting moderate and high non-overlapping effects in the intervention phase compared to the baseline phase; in other words, the intervention had medium and high effect sizes.
| Participants | NAP | PND | PAND | PEM | Cohen’s d Effect Size |
|---|---|---|---|---|---|
| PANSS | |||||
| 1 | 0.5 | 0 | 0.7 | 0.5 | 0 |
| 2 | 0.6 | 0 | 0.7 | 0.5 | 0.5 |
| 3 | 0.4 | 0 | 0.7 | 0.5 | 0 |
| 4 | 0.5 | 0 | 0.7 | 0.5 | 0.1 |
| 5 | 0.7 | 0 | 0.7 | 1 | 0.9 |
| DERS | |||||
| 1 | 0.9 | 0.5 | 0.8 | 1 | 2.2 |
| 2 | 0.6 | 0 | 0.7 | 0.5 | 0.4 |
| 3 | 0.2 | 0 | 0.7 | 0.2 | 0.9 |
| 4 | 0.8 | 0 | 0.8 | 1 | 1.1 |
| 5 | 0.3 | 0 | 0.7 | 0 | 0.3 |
According to Table 4, the percentage of non-overlapping data (PND) index was 0.0 for all participants in both scales (except for the first participant on DERS), which shows the percentage of follow-up phase points and suggests that the downward trend line in the follow-up phase did not continue and that the scores of the two scales were higher in the follow-up (a small non-overlapping effect). The other three indices were small, medium, and high, suggesting small, medium, and large non-overlapping effects in the intervention phase compared to the baseline phase, respectively. The discrepancy between these values is attributed to differences in calculations and the greater number of observations in the intervention phase compared to the follow-up, which suggests a greater non-overlapping effect. Therefore, among the evaluated indices, the PND index presented a more accurate comparison.
5. Discussion
This study aimed to determine the effectiveness of ACT on positive and negative symptoms and emotion regulation in patients with SSD. It was performed for the first time as a single-case study on five participant in Razi Educational and Therapeutic Psychiatric Center, and the results showed the effectiveness of ACT in reducing psychotic symptoms and improving emotion regulation. Although these results are inconclusive, and many factors may play a role in the patient's recovery (including TAU), ACT is an effective therapeutic intervention to provide psychological services to patients with SSD. Also, differences between the PANSS and DERS scores in the intervention and follow-up phases indicated small to medium effect sizes.
Considering the mean PANSS scores in the baseline, intervention, and follow-up phases, the rate of psychotic symptoms decreased in patients to some extent. Although the purpose of ACT is not to reduce the symptoms of psychosis, these changes may be one of its outcomes (46). Regarding the relationship between experiential avoidance and hallucinations (26) and delusions (47), it seems that ACT can change the patient's relationship with the symptoms rather than the symptoms themselves. The results are consistent with the findings of study by Yildiz (48). Since SSD patients suffer from symptoms, such as depression, anxiety, and hallucinations, it seems that ACT can first reduce the psychological stress of hallucinations and then decrease the symptoms of psychosis and emotional dysregulation.
Consistent with the findings of the present study, Shawyer et al. (26) found that ACT had moderate effects on psychotic symptoms. Considering the effect of ACT on stress caused by hallucinations, it seems that ACT improves the patient's emotion regulation after reducing stress, which is effective in reducing their psychotic symptoms. In the present study, ACT had small and moderate effects on psychosis symptoms and emotion regulation, respectively by reducing stress caused by psychotic symptoms and emotion dysregulation; nonetheless, this study had a single-case design.
Regarding the decline in the mean DERS scores, the results of the present study are consistent with the findings of previous studies conducted by White et al. (23), Louise et al. (49), and Villatte et al. (50), which suggested a reduction in emotional dysregulation caused by psychosis and acceptance of emotions. The ACT possibly encouraged patients to move toward their life values and goals by helping them accept their painful mental experiences; this played an important role in their emotional functioning. According to these findings, ACT was effective in improving the patients’ emotional regulation.
Based on the scores of the first, second, fourth, and fifth participants in the intervention phase compared to the baseline phase, the scores of psychotic symptoms and emotional dysregulation decreased compared to the baseline phase, which shows the low to moderate effectiveness of ACT. Also, the first, third, and fourth participants obtained low scores on PANSS in the follow-up, and the scores of the second and fifth participants showed a moderate effect size; in other words, ACT had small and moderate effects on the symptoms of psychosis. Considering the relationship between anxiety reduction and cognitive defusion (51), it seems that ACT, by using failure strategies, such as conscious observation of psychiatric experiences, reduces the stress caused by the symptoms and then diminishes psychotic symptoms and improves emotion regulation. Although it is not clear if cognitive defusion is effective in reducing the symptoms, this study showed that ACT could offer effective strategies, such as acceptance and non-judgment, distancing, and isolation from psychotic experiences.
Tyrberg et al. (52) and White et al. (23) showed that people with psychosis can follow their personal values by attending ACT sessions. However, the average number of ACT sessions in their study was two sessions, while in the present study, 15 ACT sessions were held. Based on the findings, although all participants experienced psychotic symptoms constantly, commitment to therapeutic homework appeared to be effective in reducing psychotic symptoms and improving emotion regulation. By using mindfulness and emotion acceptance, ACT seems to help patients view their treatment as a rewarding experience; this result is consistent with the findings of a study by Spidel et al. (27). This result is of great significance owing to the role of emotion regulation in an individual’s functioning and psychotic symptoms (31). Although ACT may be helpful for SSD patients, any conclusions regarding the effectiveness of ACT for this group should be made with caution. Therefore, further research is needed to replicate our findings using a larger sample size and group therapy and compare the findings with a control group.
The most important limitation of the present study is that due to the COVID-19 epidemic, sampling and testing were performed under strict observance of health protocols. Therefore, it is recommended to perform ACT in a group for people with SSD in psychiatric and mental health centers in case of reduction of the coronavirus disease epidemic. Also, not checking negative symptoms, small sample size, and limited generalizability of the findings made it difficult for us to reach definite conclusions. On the other hand, the strengths of this study include exclusive, patient-centered treatment, collaboration with other therapists (e.g., psychiatrists, psychologists, nurses, social workers and counsellors), and initiation of treatment after control of acute psychotic symptom with medications.
5.1. Conclusions
The application of the ACT may be an appropriate and valuable additive for reducing the psychotic symptoms and improving the emotional regulation of the people with schizophrenia in psychiatric and mental health centers. It can play a valuable role in the mental health of SSD patients by changing their attitude towards psychotic symptoms and improving their emotion regulation. Replication of this study in the future can provide promising results for the establishment of ACT in psychiatric wards. It seems that ACT is a suitable option for psychologists, psychiatrists, nurses, and paramedics working, counsellors, mental health experts and other clinical professionals working in Educational, Therapeutic and Rehabilitation Psychiatric Centers.
5.2. Highlights
The ACT plays an effective role in reducing the positive and negative symptoms of SSD patients and improving their emotional regulation.