1. Background
Substance use and its consequences place a considerable social and economic burden on society (1). According to the united nations office on drugs and crime (UNODC), 271 million adults, or 5.5% of the world's adult population, had used drugs in the previous year, 2019. While this number is almost similar to that of the previous year, a longer-term view indicates a sharp increase relative to 2009 (2).
Based on the available evidence, drug use has several consequences, including increased mortality, high-risk sexual behavior, increased risk of sexually transmitted diseases, etc. (3). For instance, UNODC reported that nearly 350 lives were lost due to drug use in 2019 (4). Moreover, those with drug use tend to become more dependent chronic users, leading to physical, psychiatric, and medical comorbidities, apart from stigmatization and social marginalization. These people's feelings about the world (e.g., marginalization) are mainly shaped by their lived experiences (5). Furthermore, several studies warned about high rates of resumed drug usage among addiction sufferers who stop using drugs, ranging from 60 to 80% (6).
According to national statistics, drug use has increased in Iran in recent years and reached about 2.7% of the country's population (7). So, in Iran, drug use is three times the global average (8). Several reasons are mentioned for this issue, including the shared border with Afghanistan, the largest producer of opium worldwide (9).
Studies performed on drug use during the past decades have mainly focused on understanding this issue and the effectiveness of treatment (6). However, to effectively prevent and/or minimize the negative consequences of drug use, it is important to extend our knowledge about the mental health and psychological challenges of these patients in addition to paying attention to the physical condition and drug treatments to ensure appropriate support and application of effective strategies (10). In other words, no one else can meaningfully express the real experience of the intended problem. Therefore, engaging those with lived or living experience in the planning, delivery, and evaluation of programs and policies can provide vital information to policymakers to make sure that an effective approach is followed that best meets the needs of those suffering from the target problem, as well as their families. In this line, there is extensive support for growing and developing the lived experience of those with substance use in both developed and developing countries (6, 11-13). The study of lived experiences describes the point of view of many people about a concept or phenomenon. The main goal of this method is to reduce people's experiences from a concept to a description of the true nature of that phenomenon. In this method, data is collected from people who have experienced the phenomenon in question. Usually, data collection in lived experience analysis studies includes deep and multiple interviews with participants (14).
When it comes to the causes of the spread of addiction in a society, it is very simple and possible for anyone who knows the alphabet of social issues to state reasons such as the lack of recreational facilities, limited employment, lack of faith and commitment, etc. However, to what extent is the contribution of each of the problems in creating the phenomenon of addiction and its social spread, where and how to start to fight it, the suitability of the morals and social standards of this society with the societies that benefit from specific methods have been successful in reducing the effects of addiction, how much and whether these methods can be effective. Dozens of other questions are issues that should be determined by research. To identify the problem and provide solutions to solve the problem, it is necessary to pay attention to the structure of the society, such as the historical, economic, social, political, cultural, demographic, and regional conditions and the state of social relations, the management system of society, family and political management. Therefore, simply conducting similar studies in other societies and using their results in other groups, especially regarding the problem of addiction, does not seem correct.
2. Objectives
In this research, the aim was to identify the experience of drug users regarding the psychological aspect of their lifestyle. Since the people treated with methadone will reach some mental stability with the passage of time, the research was conducted on these people.
Based on what was mentioned above, using a community-based participatory research approach, this study investigated the lived experience of substance users under methadone maintenance therapy in Iran.
3. Methods
3.1. Study Design
Narrative inquiry (a type of qualitative research) was applied in this study, which is, according to previous studies, one of the most effective methods developed to understand the experiences of a particular group (15, 16). This approach is based on listening to other people's experiences to capture and understand their feelings, experiences, and the reasons behind their behaviors (6). The current study has been conducted based on data collected through in-depth interviews and field notes.
3.2. Participants
A total of 26 in-depth interviews were conducted with people who suffered from substance use (7 females and 19 males) in 2021. Participants were selected using purposive and convenient sampling techniques during the study period. The criterion for participating in the interview was a history of methadone treatment for more than three months and a willingness to participate in this study. To select the patients, a coordination meeting was first held with the officials of the three addiction treatment centers in Isfahan, Iran. After going through the administrative process and obtaining the necessary permits, the researchers arrived at the centers. In all patients who went to outpatient methadone maintenance treatment centers to receive methadone, the entry criteria were checked. If they met the necessary conditions, the objectives of the study were explained to them. If they wished to participate in the study, after obtaining written consent, they were given a turn for an interview. The participants' interviews were from August 21 to October 4.
The interviews were conducted in a safe and quiet room, respecting the privacy of the patients and assuring them that their information would not be shared with anyone. The first author conducted all interviews. The interview guidance contained several open-ended questions designed to extract the interviewees' experiences. In-depth and semi-structured interviews were used to collect information. The interview protocol was implemented in four stages. In the first step, the interviews started with the opening text. In this part, information about the purpose of the research was given to the participants. In this section, the confidentiality of their answers was discussed to reduce the participants' concern. In the second step, questions were raised. These questions were about what challenges and experiences the patients had in psychological issues and what conditions affected these problems and experiences. Additional questions were asked when necessary for clarification. The third stage was the implementation of probes, which were used to encourage people to talk or not to go astray during the interview, such as: "May you explain more?" Finally, and in the fourth stage, it was the end of the interview. The interview was finished when the participants described their experience, and no further explanation was necessary.
All interviews were audio-recorded and transcribed. The interviews lasted from 70 to 90 minutes. In addition to audio recording, field notes were taken for the greater accuracy of data collection. The Interviews continued to the point where researchers felt that new information could no longer be obtained with the inclusion of new samples after 26 interviews. It is worth noting that all interviews were read repeatedly to achieve immersion and obtain a sense of the whole. Data analysis proceeded in parallel with interviews.
3.3. Data Analysis
Colaizzi's method (1978) was applied to analyze the collected data (17). It includes seven steps: Initially, the researcher reads the transcripts to gain a sense of the participant(s). Afterward, statements with significance to the research question should be identified and extracted, which must be direct quotations of the interviewee to reflect the research data accurately. Afterward, the researcher begins to articulate what the statements mean to extract themes, followed by categorizing similar themes. Eventually, the results should be integrated into a comprehensive topic description. Following an inductive approach, the codes were extracted by two independent reviewers, and arguments were referred to a more experienced and knowledgeable third party. An excel spreadsheet was created and used to collate and screen the relevant codes and themes. Data analysis was administered using MAXQDA version 2020.
It is worth noting that since the present study aimed to evaluate the lived experiences of patients with substance use, coding and theme extraction were carried out within the framework of research questions. For this purpose, the researchers only relied on the data to extract the themes, and previous theoretical ideas and findings were not considered. All transcripts were read repeatedly to achieve immersion and obtain a sense of the whole.
3.4. Ethical Considerations
The research purpose and methodology were scrutinized by the research ethics committee of the authors’ university (IR.IAU.YAZD.REC.1400.025). Written informed consent was obtained from all participants before entering the study and after a comprehensive introduction to the study protocol. In addition, the participants were informed that they could withdraw from the study at any time. Confidentiality of the study participants' information was maintained throughout the study by making them anonymous and asking them to provide honest answers.
4. Results
Twenty-six (n = 26) subjects participated in this study, 7 females and 19 males. Most of the participants were educated diploma and above. The participants' age ranged from 25 to 53 years old. At the time of the interview, participants were in the methadone treatment phase for more than three months.
The characteristics of participants and their backgrounds are provided in Table 1.
| Case | Age | Gender | Year of Substance Use | Methadone Treatment Time (mo) |
|---|---|---|---|---|
| 1 | 53 | Male | 31 | 34 |
| 2 | 32 | Male | 10 | 20 |
| 3 | 45 | Male | 20 | 23 |
| 4 | 25 | Female | 6 | 6 |
| 5 | 51 | Male | 28 | 31 |
| 6 | 48 | Male | 32 | 15 |
| 7 | 38 | Female | 11 | 5 |
| 8 | 29 | Male | 10 | 4 |
| 9 | 37 | Male | 8 | 13 |
| 10 | 48 | Male | 21 | 18 |
| 11 | 47 | Male | 23 | 23 |
| 12 | 50 | Male | 28 | 8 |
| 13 | 30 | Male | 12 | 6 |
| 14 | 52 | Male | 26 | 15 |
| 15 | 39 | Male | 18 | 5 |
| 16 | 47 | Male | 16 | 9 |
| 17 | 51 | Male | 33 | 12 |
| 18 | 44 | Male | 17 | 13 |
| 19 | 36 | Female | 14 | 8 |
| 20 | 44 | Male | 21 | 21 |
| 21 | 32 | Female | 8 | 6 |
| 22 | 39 | Male | 18 | 21 |
| 23 | 47 | Male | 28 | 14 |
| 24 | 44 | Female | 15 | 7 |
| 25 | 36 | Female | 12 | 10 |
| 26 | 34 | Female | 5 | 5 |
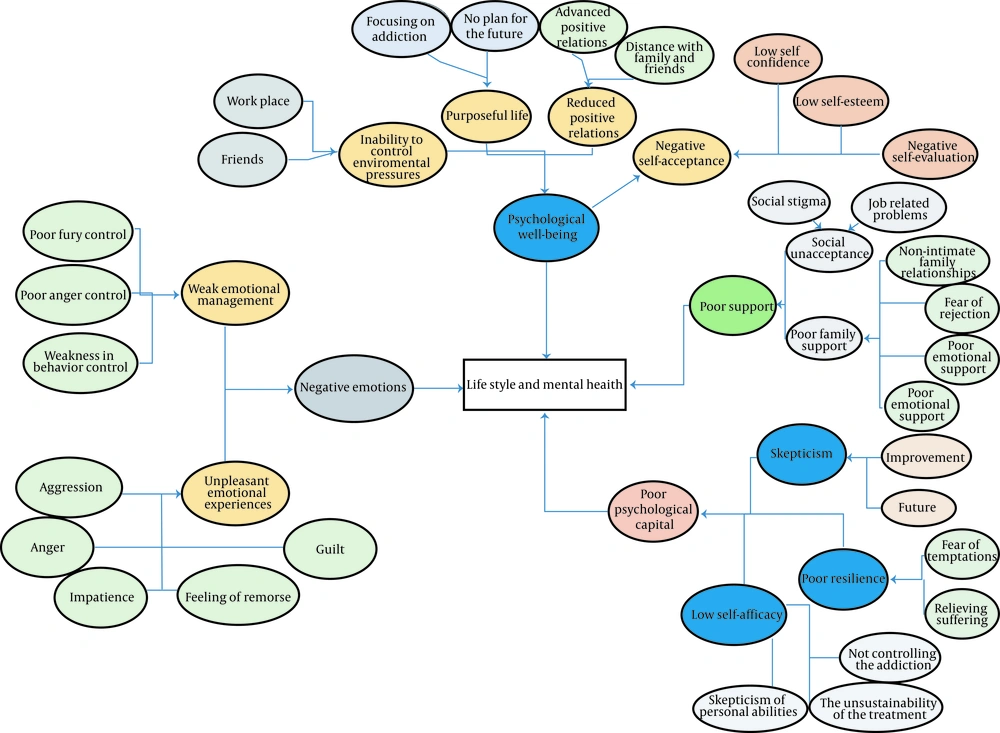
As mentioned before, all interviews were audio-taped and transcribed, and data analysis was performed simultaneously with the interviews. Data analysis was performed by two researchers independently; so that each of them read the transcript and open-coded the data (17). The extracted codes were discussed between the researchers, and arguments were referred to a more experienced and knowledgeable third party. Four themes and 11 sub-themes emerged from the categorized data. The themes were as follows: (1) negative emotions (feelings that cause you to be miserable and sad); (2) poor psychological capital (a set of resources a person can use to help improve their performance); (3) poor Support (contains two components of weak family support and social unacceptance; (4) psychological well-being (contains four components of negative self-acceptance, reduced positive relations, not having a purposeful life, and inability to control environmental pressures) (Table 2).
| Theme, Sub-theme 1 and Sub-theme 2 | Codes |
|---|---|
| Negative emotions | |
| Weak emotion management | |
| Poor anger control | Inability to control anger, inability to control anger in the face of stressful events, inability to control anger during arguments, loss, inability to control yourself when feeling angry, Inability to control anger when methadone-maintenance therapy dose is reduced, inability to control self-anger behaviors, grumpiness when lacking access to drugs, inability to control anger |
| Weakness in behavior control | Weak behavior control in cases of late access to drugs, inability to control behavior during delayed substance use |
| Unpleasant emotional experiences | |
| Anger | Anger in cases of delayed use, Direct association between feeling anger and time since the last use |
| Impatience | Boredom when drugs are not available, feeling boredom between two consumptions |
| Aggression | Aggressive behaviors when drugs are not available, Violence, and substance use |
| Guilt | Thinking about leaving the family due to feeling guilty, suicidal thoughts due to feeling guilty, feeling guilt from beating and burning children's hands, feeling of guilt towards the family, feeling guilty because of neglecting the wife, guilt mitigation by comparing the actions with other addicts, feeling of cruelty, feeling of abuse the family's trust |
| Feelings of remorse | Regret of being addicted, regret caused by experience learned due to addiction |
| Poor psychological capital | |
| Skepticism | |
| Improvement | Pessimism about self-improvement, pessimism about the post-withdrawal period, pessimism about the future, pessimism about improving health in the future |
| Future | Despair towards the future, frustration, fear of changing conditions hinders substance withdrawal, inability to withdraw the substance use due to fear of the future, the importance of emphasizing hope for the future, pessimism about the future due to the impact of addiction history, pessimism about the future, hopelessness towards life |
| Poor resilience | |
| Fear of temptations | Temptations caused by anger, fear of recursing, fear of inability to self-control after withdrawal, worrying about being tempted to use drugs again, the importance of self-control |
| Relieving suffering | Increasing the dose to forget the grief of mother's death, substance use to forget the grief of losing the brother, substance use to confront unpleasant events, to mitigate the grief of losing a loved one, to cope with personal problems |
| Low self-efficacy | |
| Not controlling the addiction | Poor self-control against the temptations of continuing substance use, lack of control over the temptation at the start of the addiction |
| The unsustainability of the treatment | Tendency to use drugs if available, occasional use of heroin even under MMT, friend's temptation after overcoming drugs, withdrawal due to family pressures |
| Skepticism of personal abilities | Skepticism of personal abilities to successfully withdraw the drug's use, lack of self-confidence to create positive conditions |
| Poor support | |
| Weak family support | |
| Fear of rejection | Fear of exposing addiction and rejection from the family, fear of being rejected by the partner, using makeup and clothes to hide the addiction |
| Poor emotional support | The important role of the partner in quitting, the impact of the partners' affection and companionship, the need for emotional support of others, loss of family's affection, poor emotional relationship with the family, feeling of being abandoned by the family |
| Non-intimate family relationships | Declined relationships with the family lead to the development of addiction, poor marital status, staying away from the family, being forgotten by the family, difficulties of substance withdrawal due to inadequate knowledge of the spouse |
| Not being reliable in the eyes of others | The inattention of the family members, being neglected by the family, the neglect of the family to the addicted person, being humiliated by the husband due to the addiction |
| Social unacceptance | |
| Job-related problems | lack of job security, low job security, problems in finding a job due to addiction history, job dismissal |
| Social stigma | Fear of being stigmatized as a thief, history of incarceration for drugs, fear of being accused of stealing, worrying about people's feelings, being subjected to the destructive stigma |
| Psychological well-being | |
| Negative self-acceptance | |
| Low self-confidence | The feeling of losing confidence due to substance use, the feeling of lack of confidence |
| Negative self-evaluations | Self-loathing, disliking yourself, having bad feelings about yourself, not feeling good about yourself, yourself, not imagining yourself as a good person |
| Low self-esteem | Deciding to substance use to avoid humiliation by the husband's friends, the feeling of becoming a worthless human being, the feeling of being inefficient, the feeling of being a worthless |
| Reduced positive relations | |
| Reduced healthy relationships | Desire to stay at home, distance from old friends due to addiction, lack of relationship with friends, inability to travel due to addiction, not spending time with friends due to addiction |
| Gaining distance from family members | Distancing from children, feeling alienated from the girl as she grew up, being rejected by the family, children distance their addicted parents as they grow up, not having fun with the family, being annoyed while having fun with the family due to covert substance use, |
| Not having a purposeful life | |
| Not having a plan for the future | Spending time without a plan, lack of plans for future life, lack of a plan for the future, ignoring the future, feeling aimless |
| Efforts that enforce addiction | Working to earn substance money, making money for drugs, switching to a lower-paid job for easier substance use, working just to earn substance money |
| Inability to control environmental pressures | |
| Temptations of addicted friends | Friends' temptation for the first use, substance use to avoid being humiliated by friends, having addicted friends, Having addicted friends as the main reason for substance use |
| High-pressure working environment | Relations with addicted persons at the workplace, first use at the workplace, continuing to use due to friends' temptations at the workplace, substance use due to stimulations caused by the new workplace, having addicted colleagues |
An outline of the thematic network is provided in Figure 1.
4.1. Negative Emotions
Negative emotions are feelings that cause the person to be miserable and sad (18). Its subthemes included: (1) weak emotion management; and (2) unpleasant emotional experiences. In addition, it contained eight components: Poor fury control, poor anger control, weakness in behavior control, anger, impatience, aggressiveness, guilt, and feeling of remorse. In this line, interviewee 8 noted, “At that time, I had bad feelings and highly aggressive behaviors”.
Or Interviewee 18 stated, “I have two children, and it is difficult for me to tolerate their behaviors at home”.
Or interviewees 3 and 7 mentioned aggressive behaviors when the substance was unavailable.
4.2. Poor Psychological Capital
It refers to a set of resources a person can use to help improve their performance (19). Poor psychological capital contains three components: Skepticism, poor tolerance, and low self-efficacy. Skepticism is about the poor attitude of participants about themselves and their future. It includes two components: Getting rid of the addiction and having a bright future. For instance, interviewee 14 stated, “I'm not hopeful of getting rid of the addiction. You know, I have hurt myself a lot”.
Or interviewee 26 noted, “The skepticism prevented me from trying to withdraw”.
In this study, poor tolerance refers to addicted persons' weakness in coping with negative events and trying to fix the problems. It contains two main components: Fear of temptations and how to relieve suffering. Concerning the former, interviewee 2 stated, “I am really afraid of temptations; I cannot control myself”.
Regarding the latter, interviewee 17 noted, “I had a cousin with whom we grew up together and was my playmate in Isfahan. One day I was informed about his suicide, and I could not believe that. My grave continued for five months. Then, my sister's husband tempted me to use drugs. Since that time, I have used drugs whenever something bad happens to me”.
Or interviewee 1 stated, “My mother's death was terrible for me; hence, I increased the drug dose, which worsened my condition”.
Low self-efficacy refers to not trusting the abilities to achieve success. It contains three components: Hard-to-resist temptations, the unsustainability of the treatment, and skepticism of personal abilities".
For instance, interviewee 16 stated, “I've come to the conclusion that someone who gets addicted can't keep him/herself. I didn't smoke drugs for three years; one day, I went somewhere, and a friend of mine gave me 50 grams of opium. He probably wanted to tempt me. I told myself it was just one time and nothing would happen. I always tell myself this is the last time”.
Another interviewee pointed out that “A considerable share of my income was always for buying drugs, and the rest was for my family. I wasn't a constant consumer, but I couldn't resist temptations”.
Concerning instability of the treatment, participants pointed out that the treatment process is unstable or think so, which means a high likelihood of recurrence. For instance, interviewee 2 said, “I couldn't resist temptations, and currently, I'm using drugs because of friends and family”.
In addition, participants mentioned skepticism regarding their abilities to continue the treatment. For instance, interview 11 said, “I think not being capable of withdrawing the drugs to improve the condition of myself and my family”.
Or interviewee 24 pointed out, “You know, I think withdrawal is difficult for me”.
4.3. Poor Support
Poor support contains two components of weak family support and social unacceptance. The former refers to benefiting the family support, which the participants have been deprived of, that contributed to their worsening status. It comprises four main themes: Fear of rejection, poor emotional support, non-intimate family relationships, and not being reliable in the eyes of others.
In this study, fear of rejection refers to participants' concerns and fears of being rejected by those around them. For instance, interview 13 noted, “I'm the only one with addiction in my family. My wife believes that an addicted person does not deserve married life. I fear being rejected by her. It makes me feel bad”.
Or interviewee 1 pointed out, “I was always dressing well to hide my addiction because I was worried about my lookalike and others' judgment (interview 1)”.
Emotional support refers to poor emotional relations with the family and not benefiting from their support. Interviewees 2 and 17 pointed out the importance of this factor. For instance, interviewee 20 said, “My family and friends supported me in resisting temptations after the withdrawal. But I fear it as I'm aware of its negative consequences. I have decided to go to my sister's house for the next holiday to avoid bad people”.
According to the findings, non-intimate family relations were among the factors that increased the likelihood of addiction. For instance, interviewee 3 noted, “I had problems with my family when I was a teenager, as I loved someone, so I distanced myself from my family and started to take drugs”.
Not being reliable in the eyes of others was a significant barrier to receiving support from the family. Participants explained that they had lost the support of their family since they noticed their addiction. For instance, interviewee 5 noted, “They were ignoring me, and I was ignored by them”.
The second component of poor support was social unacceptance, which contained two themes: Job-related problems and social stigma. The former includes a lack of job security problems in finding a job due to addiction history and job dismissal. In this line, interviewee 9 noted, “I fear the future, as I don't have job security”.
Or interviewee 17 pointed out, “I lost my job because of addiction”.
The social stigma component contained fear of being stigmatized as a thief, a history of incarceration for drugs, fear of being accused of stealing, worrying about peoples' feelings about you and your habits, and being subjected to the destructive stigma. Interviewees noted that even after withdrawal, they are subject to stigma. For instance, interviewee 10 said, “It's really true. It doesn't worth it. They make money from drugs in ways incompatible with my personality. For instance, selling their furniture. In the eyes of society, there is no difference between addicted persons, either rich or poor”.
He also added, “When I went to the toilet, why he didn't come back? Is he using drugs? I'm always subject to stigma. I'm always worried that my family members will accuse me of stealing something that is lost”.
4.4. Psychological Well-being
The participants pointed out their psychological problems since the onset of addiction. It contains four components: Negative self-acceptance, reduced positive relations, not having a purposeful life, and inability to control environmental pressures. The negative self-acceptance and reduced positive relations contain low self-confidence, negative self-evaluations, and low self-esteem. The first theme refers to negative self-evaluations of the addicted person and contains three subthemes: Low self-confidence, negative self-evaluations, and low self-esteem. In other words, participants believed that the addiction declined their self-esteem, which is translated into low self-confidence. For instance, interviewee 3 said, “Addiction took everything from me. It destroyed my self-confidence, and I do afraid of being judged by others”.
Most of the dissatisfactions were regarding personal performance and bad feelings about oneself. In this line, interviewee 6 pointed out “I did hate myself”.
Or interviewee number 18 noted, “I think of being a worthless human”.
The component of reduced positive relationships comprised of reduced healthy relationships and gaining distance from family members. The former refers to enjoying a healthy relationship with friends and others. For instance, interview 23 said, “Even I do not have enough time to spend with my friends because they are not addicted”.
Or interviewee 1 noted, “When I decided to reduce the frequency of substance use, I had enough time to go out with my friends. I didn't like to stay at home”.
Concerning gaining distance from family members, interviewee 5 noted, “There was a huge distance between us, but everything has changed”.
Or interviewee 26 noted, “My family members did not like me and were ignoring me. The same was true for my children”.
The other important component did not have a purposeful life. The participants pointed out not having a purpose and only caring about their addiction. This theme comprises two components: Not having a plan for the future and efforts enforcing the addiction. Concerning the former, participant 1 noted, “I cared about nothing except my addiction. Even I did not have a plan for my child”.
Or participant 22 said, “Drugs made my life aimless. It was just day and night. The best days of my life, when I could do many positive things, have been wasted”.
Participants noted that their only aim was to find drugs. For instance, participant 13 pointed out, “I did not have fun those days. My life was just working, working, and working. Then, addiction created an extra burden, and I did not have any option except to earn more money to buy drugs”.
The last extracted theme was the inability to control environmental pressures and comprised of temptations of addicted friends and a high-pressure working environment. Regarding temptations of addicted friends, interviewee 8 noted, “I was feeling bad, and my friends tempted me to consume opium”.
Or interviewee 19 said, “I used to go to parties to drink wine and smoke drugs. And soon, it becomes a habit”.
Concerning the second component, interviewee 17 said, “25 years ago, everyone in my workplace was addicted. You may not believe I had no option except to use drugs; it was not to enjoy. Soon I was addicted. Initially, we smoked drugs for fun once or twice a month. For me, it took five years to become addicted. When I found a new job, one of my collaborators was an addicted person who used to consume black drugs (i.e., opium). He told me that I have a simple code to stay away from those who consume white drugs. However, I told myself it was ok to use for one time, let's test it, and it was so good. I used to consume white drugs for five years”.
The other main theme was incentives to withdraw, which comprised three themes: (1) understanding negative consequences; (2) long-term problems of addiction; and (3) maintaining family cohesion. The first theme contained six components of family disputes, maintaining social dignity, self-control problems, health status, financial loss, and losing job opportunities.
Concerning understanding negative consequences, interviewee 16 said, “When I became addicted to drugs, I had continuous conflicts with my family. We were on the edge of divorce, and I went to prison. My wife was trying to force me to withdraw; that's why she went to court”.
Or interviewee 20 noted, “I hated to be known as an addicted person. Even now, if someone knows my past, I will be ashamed”.
Regarding how to obtain drugs, interviewee 14 noted, “Even I couldn't go on a short trip or to family gatherings because I was addicted. Or I had problems going to a seminar. While I used to eat well and wear good clothes, it was obvious that I was addicted, and it was annoying me”.
Interviewee 17 said, “One day, I told myself, hey, this is not a good life, and you must withdraw from drug abuse. So, I went to buy methadone”.
Another important subtheme was maintaining family cohesion. In this regard, interviewee 10 noted, “Why did I decide to withdraw the substance use? My children were grown, and I needed to be valuable in their eyes”.
Or interviewee 6 said, “I have a good relationship with my family, and their happiness is important to me. So, I decided to withdraw”.
According to the findings, one of the most important concerns of addicted persons is disclosing their problems. For instance, interviewee 13 said, “My son is 13 years old, and he has medical problems; that's why my wife didn't notice my addiction yet. Even now that I'm withdrawing, she is unaware of my status”.
5. Discussion
The current study intended to extend our knowledge regarding the lived experience of those suffering from substance use in the Isfahan province of Iran. The participants shared their journey as they faced challenges and problems regarding their daily living or treatment.
In general, the present findings are in line with previous studies. One of our significant findings was the link between negative emotions and a high inclination toward addiction. In this line, Schlauch et al. noted that elevated negative affect was associated with more inclination towards addiction (20). In the same vein, in a study on craving for alcohol, Kavanagh et al. found that experiencing negative emotions increases both frequency and intensity of alcohol consumption (21). In a study on how to prevent addiction, Raisjouyan et al. reported that educational programs could increase emotional quotient, which is translated into reduced inclination towards addiction (22). Furthermore, our literature review showed that those with poor psychological capital are at elevated likelihood of alcohol and substance use (23-25). Those who didn't benefit from family support are more prone to use substances during stressful life events as a part of self-medication, which is consistent with the findings of the present study that revealed the importance of psychological well-being, benefiting from family support and the role of psychological capital in controlling inclinations towards substance use.
Another frequently mentioned code was the stigma associated with addiction and its consequent shame for the person and his/her family. So, one of their most important fears was disclosing the addiction to their loved ones, also reported by several studies. For instance, Goodyear et al. reported highly stigmatizing attitudes toward addicted persons. They also emphasized the fear of addicted people about disclosure of their addiction to their loved ones (26). Or in a study on addiction stigma, Kulesza et al. reported that addiction-related stigma was one of the most common implicit beliefs of those suffering from addiction (27). Shafiei et al. investigated the effect of methadone maintenance treatment on reducing crime and the social consequences of addiction. They also reported that those with substance use are socially stigmatized and ostracized by their families, which methadone can have a positive effect on (28). Aghakhani et al. also pointed out the positive role of family support in preventing and treating drug addiction (29).
We also showed that conflicts with others and family background are major contributors to initiating substance use. So that some interviewees pointed out the temptations of their friends and family members to use substances. In this line, Myers et al., in a study on the evaluation of temptation coping strategies, found that those with negative experiences (e.g., having conflicts with others) and a family member who suffers from substance use employ weaker coping strategies in a temptation situation (30). Similar results are reported by Caricati and Ferrari (31), Brechting and Giancola (32), and Mafa and Makhubele (33).
This study also had limitations. For example, the participants in this study were mostly men, and women did not have much desire to participate in the interviews. On the other hand, this group of people was studied due to more mental stability in people treated with methadone. Also, this study was conducted in three addiction treatment centers in one of Iran's cities. Considering these limitations and the type of study, caution should be exercised in generalizing the results.
5.1. Implications
In this study, four main themes were extracted from the experience of people treated with methadone regarding the psychological dimension of lifestyle. These dimensions include negative emotions, poor psychological capital, poor support, and psychological well-being. In addition to drug treatment and paying attention to the physical aspect of addiction, it is necessary to consider the psychological aspects of patients to develop an effective treatment plan. In this study, these cases were extracted to compile training packages.