1. Background
Occupational stress is a recognized phenomenon in which a person gradually suffers from adverse cognitive and behavioral reactions at work. Occupational stress develops when job requirements and workers' abilities are imbalanced. Stress affects organizational inefficiency, human resources turnover, absenteeism due to work, increased healthcare costs, and decreased job satisfaction (1-3). Based on the literature, overwork, excessive requirements, and responsibilities lead to health risks (4). Chronic occupational stress causes physical and mental health problems (5, 6). The International Labor Organization (ILO) has identified occupational stress as the most well-known health phenomenon threatening workers (7). As occupational stress increases, health problems such as alcoholism, drug abuse, hypertension, and cardiovascular diseases develop, and quality of life decreases (8, 9).
Causes of occupational stress are classified into those related to the nature of the occupation role (excessive work pressure, time pressures, lack of job control, and improper job conditions), role within the organization (role stress, role conflict, role ambiguity, and level of responsibility), career advancement (lack of job security, job stagnation, and promotion), labor relations (workplace bullying, dark leadership, discrimination, and upstream and downstream confrontation), and organizational structure (formality, management style, decision making, and participation) (3). Medical staff experiences heavy occupational stress due to excessive work pressure, increased demand from the patient, occupational hazards, work disproportionate to pay, and increased competition for a job promotion. As a result, the burnout rate among physicians is higher than the other occupational groups (10). Most physicians take medication to overcome occupational stress (11).
Spiritual intelligence is "the adaptive use of spiritual information to facilitate problem-solving and the achievement of everyday goals," which can affect occupational stress. Spiritual intelligence consists of the following components: The capacity to look beyond objects and materials, the ability to experience broad levels of consciousness, the ability to experience every day, the ability to use spiritual resources to solve problems, and the ability to be pious (12). Spiritual intelligence helps medical students achieve academic success, better care for their patients, and be happier (13). Higher spiritual intelligence is associated with reduced stress, anxiety, and depression, which improves mental health and job performance. Thus, it can improve the health of healthcare workers (14-16).
In late 2019, a novel Coronavirus spread from Wuhan, China, rapidly becoming a global health crisis. Facing the Coronavirus disease 2019 (COVID-19) pandemic put the medical staff under more physical and psychological pressure than before (17, 18). In such a crisis, medical students may be abused. During the pandemic, medical students were employed in clinical care differently. Some universities forbade interaction with the patient, while others employed students as front-line personnel (19).
According to mental health guidelines and psychosocial considerations, during the COVID-19 pandemic, the World Health Organization (WHO) protected medical staff against chronic stress and mental health deterioration. It should be kept in mind that this situation will not disappear overnight; rather than repeating short-term crisis measures, the focus should be placed on long-term job capacity (20).
2. Objectives
The present study aimed to determine the level of occupational stress in medical interns during the COVID-19 pandemic and the effect of spiritual intelligence.
3. Methods
3.1. Study Design and Setting
This cross-sectional study was carried out on medical interns at Shahid Beheshti University of Medical Sciences, Tehran, Iran, in the autumn of 2020. Medical students studying in the fifth academic year and above who volunteered to participate in the study were included. Also, participants who gave incomplete answers to the questionnaires were excluded from the study.
3.2. Sample Size
Due to the lack of similar studies in Iran, considering P = 50% in Cochran's formula, the sample size was estimated to be 209 (d = 0.07, α = 5%, and 10% drop). We obtained the list of medical interns from the School of Medicine. We considered a corresponding number for each eligible person. Then sampling was performed based on the simple random method using a random number table. This study intentionally used simple random sampling to avoid selection bias.
3.3. Measures
To collect the data, online questionnaires were designed. The link to the questionnaires was sent to the target population using WhatsApp and Telegram social networks. They were asked to respond to the questions and send back their answers online. The study questionnaires comprised three parts: (1) socio-demographic characteristics (age, gender, marital status, academic year, residence status, career interest, economic status, smoking, and alcohol consumption), (2) Opisow Occupational Stress Questionnaire, which had 60 statements and was answered based on the five Likert scales- scored between 60 and 300-. This questionnaire evaluated an individual's occupational stress on six subscales: Role workload, role inefficiency, role duality, role limit, responsibility, and physical environment. The validity and reliability of the Persian version of the Opisow occupational stress questionnaire have been confirmed in Iran (Cronbach's α = 0.83) (21) (3) King Spiritual Intelligence Questionnaire, which had 24 statements and was answered based on the five Likert scales -scored between 0 and 96-. This questionnaire evaluated an individual's spiritual intelligence on four subscales: Existential thinking, production of personal meaning, transcendent awareness, and expanding consciousness. The validity and reliability of the Persian version of the King questionnaire have been confirmed in Iran (Cronbach's α = 0.87) (22).
3.4. Data Analysis
Data were described by frequency, percentage, mean, and standard deviation using SPSS version 16. Data were also analyzed using structural equation modeling (SEM) with EQS6.1. For the model fitness to be acceptable, the following criteria were considered: The value of chi-square to the degree of freedom (CMIN/df) < 5.0, the goodness of fit index (GFI) > 0.90, the comparative fit index (CFI) > 0.90, and the root mean square error of approximation (RMSEA) < 0.08 (23). The statistical significance (P < 0.05) and practical importance (β > 0.2) were also considered.
3.5. Ethical Considerations
This study was approved by the Ethical Board Committee of Shahid Beheshti University of Medical Sciences (IR.SBMU.PHNS.REC.1399.130). All participants completed an informed consent form. They were assured about the confidentiality of their information.
4. Results
Of 895 eligible medical interns, 300 were invited to complete the questionnaire. Finally, 209 medical interns with a mean age of 25.33 ± 2.48 years participated in the study. Also, 56.9% and 43.1% were female and male, respectively. Table 1 demonstrates participants' socio-demographic characteristics.
| Variables | Frequency (%) |
|---|---|
| Age group | |
| < 26 | 142 (67.9) |
| ≥ 26 | 67 (32.1) |
| Gender | |
| Male | 90 (43.1) |
| Female | 119 (56.9) |
| Academic year | |
| 8th | 21 (10.0) |
| 7th | 140 (67.0) |
| 6th | 48 (23.0) |
| Marital status | |
| Married | 41 (21.0) |
| Single | 154 (79.0) |
| Residence status | |
| Home with family | 40 (19.1) |
| Alone at home | 128 (61.2) |
| Dormitory | 19.6 (19.6) |
| Career interests | |
| Moderate | 51 (24.4) |
| Good | 91 (43.5) |
| Excellent | 67 (32.1) |
| Economic status | |
| Moderate | 84 (40.4) |
| High | 124 (59.6) |
| Smoking | |
| No | 49 (23.4) |
| Yes | 160 (76.6) |
| Alcohol consumption | |
| No | 162 (78.3) |
| Yes | 45 (21.7) |
Table 2 depicts scores for occupational stress and spiritual intelligence in detail. The mean total occupational stress score of the participants was 184.57 ± 23.57. Among subscales of occupational stress, the physical environment had the highest score (33.87 ± 6.94), while the role limitations had the lowest score (29.28 ± 4.91). The mean total spiritual intelligence score of the participants was 50.44 ± 13.97. Among subscales of spiritual intelligence, critical existential thinking had the highest score (15.64 ± 5.32), while the conscious state expansion had the lowest score (7.60 ± 3.70). Based on the results of skewness and kurtosis, the data have a normal distribution.
| Minimum | Maximum | Mean ± SD | Skewness | Kurtosis | |
|---|---|---|---|---|---|
| Occupational stress | |||||
| Role workload | 19.00 | 45.00 | 30.64 ± 4.41 | -0.087 | 0.276 |
| Role inefficiency | 14.00 | 46.00 | 30.07 ± 5.83 | -0.101 | -0.027 |
| Role duality | 14.00 | 46.00 | 29.37 ± 5.92 | 0.129 | -0.030 |
| Role limit | 11.00 | 40.00 | 29.28 ± 4.90 | -0.534 | 0.479 |
| Responsibility | 11.00 | 44.00 | 31.33 ± 5.56 | -0.606 | 0.698 |
| Physical environment | 13.00 | 49.00 | 33.86 ± 6.94 | -0.552 | 0.090 |
| Total score | 109.00 | 250.00 | 184.56 ± 23.53 | -0.249 | 0.253 |
| Spiritual intelligence | |||||
| Critical existential thinking | 3.00 | 28.00 | 15.64 ± 5.32 | 0.571 | 0.125 |
| Personal meaning production | 3.00 | 20.00 | 11.64 ± 3.36 | 0.289 | 0.019 |
| Transcendental awareness | 0.00 | 28.00 | 15.55 ± 4.67 | 0.295 | 0.580 |
| Conscious state expansion | 0.00 | 20.00 | 7.60 ± 3.70 | 0.617 | 1.146 |
| Total score | 15.00 | 93.00 | 50.44 ± 13.97 | 0.586 | 0.641 |
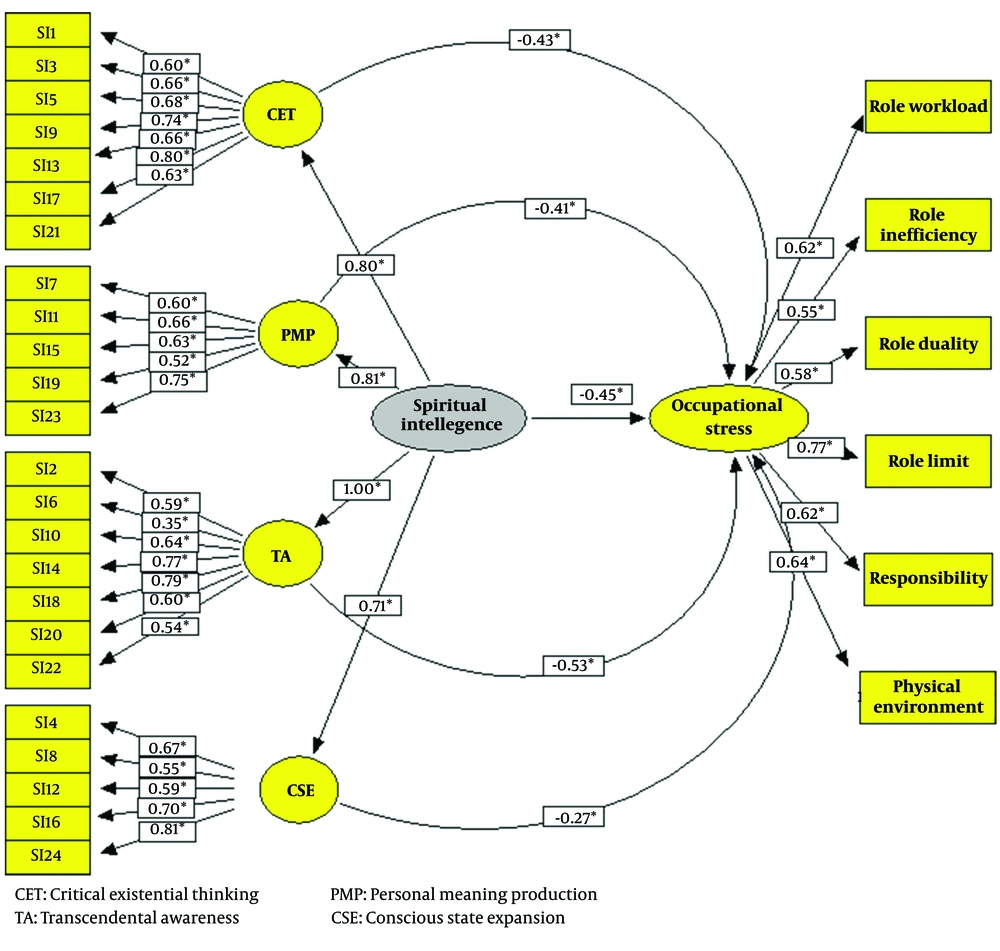
As shown in Table 3, all the model fitness indices were in the acceptable range: CMIN/df = 2.3, RMSEA = 0.07, GFI = 0.91, and CFI = 0.93. Thus, the model proposed in Figure 1 was confirmed. Spiritual intelligence was a factor affecting occupational stress (β = -0.45). Besides, all of the subscales of spiritual intelligence had a negative impact on occupational stress with the following effect sizes: Transcendent awareness (β = -0.53), critical existential thinking (β = -0.43), production of personal meaning (β = -0.41), and consciousness state expansion (β = -0.27).
| Model Fitness Indicators | Values |
|---|---|
| Chi-square | 906.966 |
| Degrees of freedom (df) | 390 |
| Chi-square/df | 2.3 |
| Root mean square error of approximation (RMSEA) | 0.07 |
| Root mean square residual (RMR) | 0.08 |
| Adjusted goodness of fit index (AGFI) | 0.90 |
| The goodness of fit index (GFI) | 0.91 |
| Comparative fit index (CFI) | 0.93 |
Abbreviations: CET, critical existential thinking; PMP, personal meaning production; TA, transcendental awareness; CSE, conscious state expansion.
5. Discussion
This study investigated the level of occupational stress and the effect of spiritual intelligence on it among medical interns during the COVID-19 pandemic. It was one of the first studies to examine the relationship between spiritual intelligence and occupational stress among medical interns. Spiritual intelligence was a factor that negatively affected occupational stress. All dimensions of spiritual intelligence had a negative impact on occupational stress. Negative coefficients in regression equations revealed a negative relationship between spiritual intelligence and occupational stress. In other words, as spiritual intelligence increases, occupational stress decreases. These findings are in line with the research hypothesis.
In a study by Manoppo et al. on nursing staff, spiritual intelligence significantly negatively influenced occupational stress (path coefficient of -0.155) and turnover intention (path coefficient of -0.154). Besides, occupational stress significantly positively influenced turnover intention (path coefficient of 0.508) (24). The above content was consistent with our findings. In contrast, Dela Pena conducted a study on 34 basic education students and found that spiritual intelligence positively affected occupational stress, which was non-significant (r = 0.209, P = 0.236). This discrepancy may be attributed to the small sample size and different questionnaires used in the recent study (25). Furthermore, in a study by Azadmarzabadi, there was a significant positive correlation between spiritual intelligence and occupational stress (r = 0.102, P < 0.05), which is inconsistent with our findings. This difference may be due to the different questionnaires used to assess occupational stress. The study by Azadmarzabadi was performed on 308 university staff using the King Spiritual Intelligence and Health and Safety Executive (HSE) Stress Questionnaires (26).
Moreover, previous studies have revealed that higher spiritual intelligence reduced staff stress in the workplace, improving the quality of their services. Medical students with higher spiritual intelligence had more control over their behavior in stressful situations (27, 28). When individuals with high spiritual intelligence face occupational stress, they invest more time and effort and select effective coping strategies. They have higher problem-solving skills, which help them overcome difficulties. They ignore the problems' negative aspects and view them as an opportunity (29).
Additionally, religion can contribute to having a high spiritual intelligence. Religion creates a coherent belief system that is higher, giving people meaning in life and hope for the future. Spiritual beliefs enable people to make sense of adversity, stress, and the inevitable losses that occur in life and be optimistic about the next life, accompanied by peace. Attending religious services provides social support for people. Spiritual beliefs are often associated with a healthier lifestyle (30). Considering the effect of spirituality on adapting to different stresses, applying and strengthening spiritual intelligence in healthcare workers can play a constructive role in controlling stress and anxiety (31).
Spiritual intelligence is about the mind and spirit and their connection to being in the world. This requires the ability to deeply understand existential questions and insights at different levels of consciousness. Besides self-awareness, it involves recognizing our relationship to the transcendent, each other, the earth, and all beings. Thus, spiritual intelligence is an essential personal gift enabling a person to maintain inner and outer peace and express love regardless of stressful situations or acute incompatibility (32).
In a study by Semyari et al. on dental students of Tehran universities, spiritual intelligence was moderate (17). According to a study by Rahimi et al., which revealed the spiritual intelligence of nursing and midwifery students in Iran, Kerman has been at the desired level (20).
In our study, the majority of participants had moderate to severe occupational stress. In a study by Faraji et al., occupational stress was reported as a moderate-high level among nurses (33), which is consistent with our results. In the present study, the highest stress level was attributed to the physical environment and the lowest level was attributed to the domains of role duality and role range. In a similar study by Wu et al., two subscales, role ambiguity and role inadequacy, had the highest scores (15). These differences may be due to the differences in the time of studies. Our study assessed occupational stress during the COVID-19 pandemic when medical staff struggled with an increased workload. Most of the time, healthcare workers are under heavy workloads. In general, work is recognized as the biggest stressor in life. The work environment and the nature of the healthcare workers are stressful, which may lead to burnout. They suffer from sleep disorders due to the shifting nature of their jobs. Long-term stress is associated with some diseases, such as hypertension, ischemic heart disorders, and malignancies. It is clear that if healthcare workers are not healthy, they cannot properly care for patients (34). As a solution, coping strategies for occupational stress should be identified. Then protective factors against stress should be strengthened to improve health professionals' quality of life.
This study had some limitations. The study was conducted during the COVID-19 pandemic, which may affect the variables. Thus, in comparison with previous studies, this issue should be considered. According to the study design, it was impossible to control confounding variables. So, we recommend future analytical studies. In the proposed model, other variables such as age, gender, marital status, economic status, smoking, and alcohol consumption are not considered.
5.1. Conclusions
According to the fit indices of the proposed model, it can be concluded that the proposed model was acceptable. All subscales of spiritual intelligence had a negative impact on occupational stress. Thus, awareness of this matter helps the officials manage medical students' job stress by promoting their spiritual intelligence.