1. Background
Dysmenorrhea is the most common gynecological disorder among adolescent girls and women of childbearing age (1). Primary dysmenorrhea (PD) refers to painful menstruation without anatomical or obvious pelvic pathology (in contrast with secondary dysmenorrhea) (2-4). The onset of PD is usually in adolescence, within 1 - 2 years after menarche (the occurrence of a first menstrual period in a female adolescent) (1, 2). The etiology of this disorder is an increase in the production or an unbalanced amount of prostanoids secreted by the endometrium during menstruation (2). Symptoms of pain from PD usually begin a few hours before or just after the start of the menstrual period in a cyclical form and may last for 48 - 72 hours. This pain presents as suprapubic cramps and sometimes low back pain in the lumbosacral region, diffused anterior thigh pain, nausea, vomiting, diarrhea, and rarely syncope attacks. It is colic in nature and improves with abdominal massage or body movement (2, 5).
Dysmenorrhea can be considered a multifactorial disorder (6) with influential factors such as age (4, 7), maternal history of dysmenorrhea (1, 3, 6), menarche age (8-10), Smoking (3, 4), body mass index (BMI) (7, 11-13), exercise (14), nutritional status (8, 15), low socio-economic status (7), etc. In addition, the relationship between the severity of dysmenorrhea and psychological factors such as stress (8), depression or anxiety (6), poor sleep quality, inattention and hyperactivity problems, and negative self-perception has also been documented (16). Psychological factors can specifically aggravate the pain and problems caused by primary dysmenorrhea (one of the main factors reducing the quality of life and social activities among young women). Although PD is not life-threatening, it can lead to disability and inefficiency (9).
Previous studies have reported that women with dysmenorrhea tend to express more negative attitudes toward illness, menstruation, and body image than other women (6). Painful conditions are predicted to impair body image perception and negatively affect quality of life by reducing self-esteem and depression (17). Thus, body image concern is one of the main psychological factors, and a multifaceted structure consisting of cognitive, emotional, perceptual, and behavioral is important (18) that can even predict cosmetic surgeries to control this concern (19). body image components can predict the severity of dysmenorrhea (20). Patients with spinal pain reported swollen backs only due to concerns about body image (21). Also, higher pain levels led to more dissatisfaction with body image, resulting in more severe depression (22).
On the other hand, empirical evidence shows that cognition has an important role in pain indices and patients' adaptation to chronic pain (23). Metacognition is a multidimensional concept referring to individuals’ knowledge of their cognitive processes contributing to the cognition evaluation, monitoring, or control (24). Thinking about pain can help individuals cope (positive metacognition) or believe pain is harmful and uncontrollable (negative metacognition). Thus, positive metacognitive beliefs reduce rumination and subsequent chronic pain (25, 26). For example, a positive and significant relationship has been confirmed between subscales of metacognitive beliefs and the overall score of headache indices (23). A deficiency in the ability or use of metacognitions would lead to emotional disorders, ultimately increasing chronic pain (26). On the other hand, self-aware individuals have fewer concerns about their body image, leading to the presumption that subscales of metacognitive variables could predict changes in body image concern (27).
Another variable that has recently attracted the attention of researchers in pain is the concept of pain self-efficacy, reflecting and predicting many specific behaviors and pain justifications among patients with chronic pain (28). In a study by Ferrari et al. on 199 patients with chronic low back pain, low-pain self-efficacy had a significant relationship with the intensity and duration of pain (29). People with high levels of pain self-efficacy can use the desired resources to reduce pain and discomfort and control pain (30).
People’s judgments about their abilities depend on their physical states, which, in turn, are affected by their emotional states and the general quality of life in all its dimensions. Conversely, low self-efficacy can lead to mental states such as fatigue, anger, pain, and suffering, decreasing quality of life (31). Accordingly, people with low self-efficacy surrender instead of seeking to deal with the existing challenges and do not realistically deal with the issues and problems (32, 33). Women's appearance evaluation is related to their health evaluation, and the more they believe in their attractiveness and appearance, the higher they evaluate their health. Hence, when women feel incompetent due to distance from physical social norms, they experience low self-efficacy (34). The results of a study by Jafary et al. also showed a significant relationship between self-efficacy and body image satisfaction (35). On the other hand, Alcı and Yüksel showed a significant relationship between self-efficacy and metacognitive awareness, which could affect academic achievements (36).
2. Objectives
Given that PD, especially in young girls, is one of the most common reasons for absenteeism or refusal from any personal or social activities and can affect their course of life and social activities, it is necessary to consider the role of related variables in its incidence and conduct more studies to take effective measures for the reduction of this pain. However, the review of relevant literature highlighted several studies within the framework of the present study. No research has examined the relationship between metacognitive beliefs and body image concern on the severity of PD and the mediating role of pain self-efficacy through a coherent model so far. Also, considering the importance of examining the present variables on young girls, especially students, the need for the present study is becoming more apparent to fill the existing gap in the literature. Thus, the following research question is raised: Is the proposed model for the relationship between the mentioned variables suitable for the data?
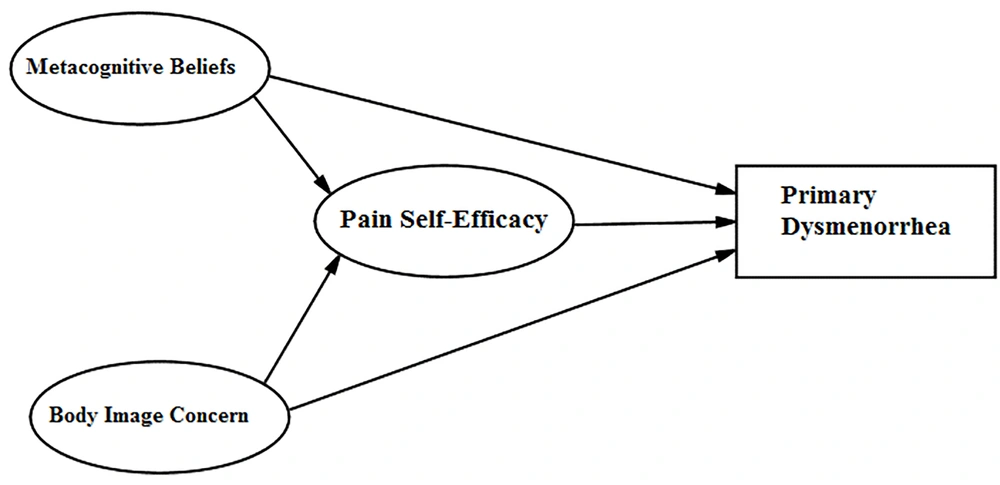
Based on the above question, we hypothesized that metacognitive beliefs and body image concerns affect primary dysmenorrhea directly and also with the mediating role of pain self-efficacy (Figure 1).
3. Methods
This study was applied and cross-sectional. Given that the researchers sought to examine the fit of the structural equation model for some relationships, it was correlational from SEM type, investigating the interrelationships of variables through a causal model. The study’s target population included all female students at Bojnourd universities in the first semester of the academic year 2021 - 2022, selected by convenience sampling.
There are different views on estimating the optimal sample size for structural equation modeling studies, such as Kline (2010) and Loehlin (2004), MacCallum (2001), etc. (37). Thus, given the number of variables under study and the allocation of a coefficient of 25 for each variable, and taking into account the possibility of incomplete questionnaires or experimental mortality, 860 participants were selected as the research sample through convenience sampling. Before distributing the questionnaires, participants received information about the study's objectives, and verbal consent was obtained from them. Participants were free to complete the questionnaires voluntarily. Because of the specific nature of the sample, the answers underwent primary examination after data collection, leading to 736 questionnaires after eliminating incomplete, invalid, and missing data and those not meeting the inclusion criteria. Finally, 724 questionnaires were entered into the analysis after data screening. Fortunately, the number of missing data was very small. In addition, the squared Mahalanobis distance was imputed to detect multivariate outliers, and 12 data items were determined as extreme values and excluded from the dataset. The removal of the outlying cases was performed because of their difference from other cases and their potential influence on the results.
Data obtained from the questionnaires were analyzed using SPSS.25 and AMOS 24 software. Structural equation modeling with the estimation of the maximum fit and confirmatory factor analysis was used to investigate the research questions and hypotheses and test the proposed models.
Inclusion criteria were voluntary participation, pain according to criteria for primary dysmenorrhea (cramps and spasmodic pain in the lower abdomen and lower back spreading to the thighs, occurring a few hours before or just after the onset of menstruation lasting 12 to 36 hours), no underlying disease such as ovarian cysts, uterine and myoma masses, uterine or ovarian tumors, endometriosis, pelvic complications such as inflammatory diseases of the uterus and ovaries and infections or surgery, any itching, burning, or abnormal discharge, no history of mental health problems, stress, severe anger, or sadness such as separation or death of first-degree relatives during the last 6 months, being single, not taking medication, alcohol, or tobacco, having a recent history of 3 months of painful and regular menstruation (length of menstrual cycle 21-45 days), with a VAS score of 5 or higher, and more than two years passed from menarche. Exclusion criteria were lack of consent to participate and failure to meet inclusion criteria.
3.1. Research Tools
Visual Analogue Scale (VAS): This method uses a 100-mm line, at one end of which zero (complete analgesia) and at the other end, 10 (the most severe pain imaginable), are marked by the patient. The validity and reliability of this tool were confirmed by Gallagher et al. (38, 39).
The Andersch and Milsom Scale to determine the severity of dysmenorrhea: According to this questionnaire, the severity of primary dysmenorrhea is divided into four categories: no pain (zero degrees) to severe pain (grade 3) (40, 41). Nazarpour and Khazai confirmed this tool's validity and reliability. The test-retest results also showed a correlation coefficient of 0.94 (20).
Body Image Concern Inventory (BICI): This self-report measure has two factors: (1) Dissatisfaction and embarrassment of the individuals with their appearance, checking and hiding perceived defects, (2) The degree of interference of body image concerns individual social performance. Littleton et al. showed desirable reliability and validity for this scale, with Cronbach's alpha values of 0.93, 0.92, and 0.76 for the total questions, the first and the second, respectively (42).
Mohammadi and Sajadinejad confirmed the validity of the Persian translation of this questionnaire, reporting Cronbach's alpha coefficient of 0.84 for the whole questionnaire, 0.84 for dissatisfaction with appearance, and 0.74 for the interference in social performance (43). The present study also used Cronbach's alpha to examine the reliability of the research tool, the values of which were 0.975 for the total questions and 0.915 and 0.930 for the first and the second factors, respectively.
Pain Self-Efficacy Questionnaire (PSEQ): This 10-item questionnaire assesses individuals’ ability to perform activities with ongoing pain. Nicholas obtained the questionnaire reliability by internal consistency using Cronbach's alpha of 0.92 and reported good validity for this instrument (44). Also, the validity of the Persian version of this questionnaire reflected a high correlation with the Pain Disability Questionnaire (PDQ) (45). Cronbach's alpha coefficient was 0.975 for pain self-efficacy in the present study.
Wells’ Metacognition Questionnaire (MSQ-30): The 30-item self-report scale includes five factors. The instrument’s construct validity was confirmed using factor analysis, and its reliability was reported with Cronbach's alpha between 0.76 and 0.93 for the total subscales (46).
Shirinzadeh Dastgiri et al. reported an alpha coefficient of 0.91 for the whole scale and 0.71 to 0.87 for the subscales. They also reported the retest validity of this test from 0.59 to 0.83 in the interval of four weeks (47). In the present study, Cronbach's alpha was 0.919 for metacognitive beliefs and 0.916, 0.815, 0.855, 0.833, and 0.910 for the subscales of the positive beliefs about worry, negative beliefs about the uncontrollability of thoughts, lack of cognitive confidence, beliefs about the need to control thoughts, and cognitive self-consciousness, respectively.
4. Results
Data from 724 female students with a mean age of 23.82 ± 5.06 were analyzed. Among them, 553 students (76%) were pursuing a bachelor's degree, 129 students (18%) were pursuing a master's degree, and 42 students (6%) were pursuing a PhD. Other assessments indicated that the mean age of menarche was 13.13 ± 1.64, and the body mass index was 22.70 ± 4.58.
Table 1 presents descriptive statistics related to research variables.
| Variables | Possible Values | Mean ± SD |
|---|---|---|
| Metacognitive beliefs | 1 - 4 | 2.297 ± 0.825 |
| Pain self-efficacy | 0 - 6 | 2.666 ± 1.734 |
| Body image concern | 1 - 5 | 2.623 ± 1.129 |
| Dysmenorrhea | 0 - 3 | 1.890 ± 0.811 |
Table 2 presents the values of the correlation coefficient among the variables of the measurement model.
| Metacognitive Beliefs | Pain Self-efficacy | Body Image Concern | |
|---|---|---|---|
| Metacognitive beliefs | - | - | - |
| Pain self-efficacy | 0.806 ** | - | - |
| Body image concern | -0.749 ** | -0.772 ** | - |
a ** P < 0.01
The research model was examined using structural equation modeling. First, the measurement and structural models were examined using robust maximum likelihood (MLR), which is based on non-normality. The fit indices used included χ2/df, comparative fit index (CFI), tucker-lewis index (TLI), root mean square error of approximation (RMSEA), 90% confidence interval, and standardized root mean square residual (SRMSR). Hu and Bentler suggested that the RMSEA values of < 0.08 and < 0.05 would indicate an appropriate and a good fit, respectively. CFI, TLI, and NFI indices should be > 0.95, but values of > 0.90 are also acceptable. The SRMR index with values of < 0.08 indicates a good fit (48). For the χ2/df index, Marsh and Hocevar considered values between 2 and 5 to show an appropriate fit (49).
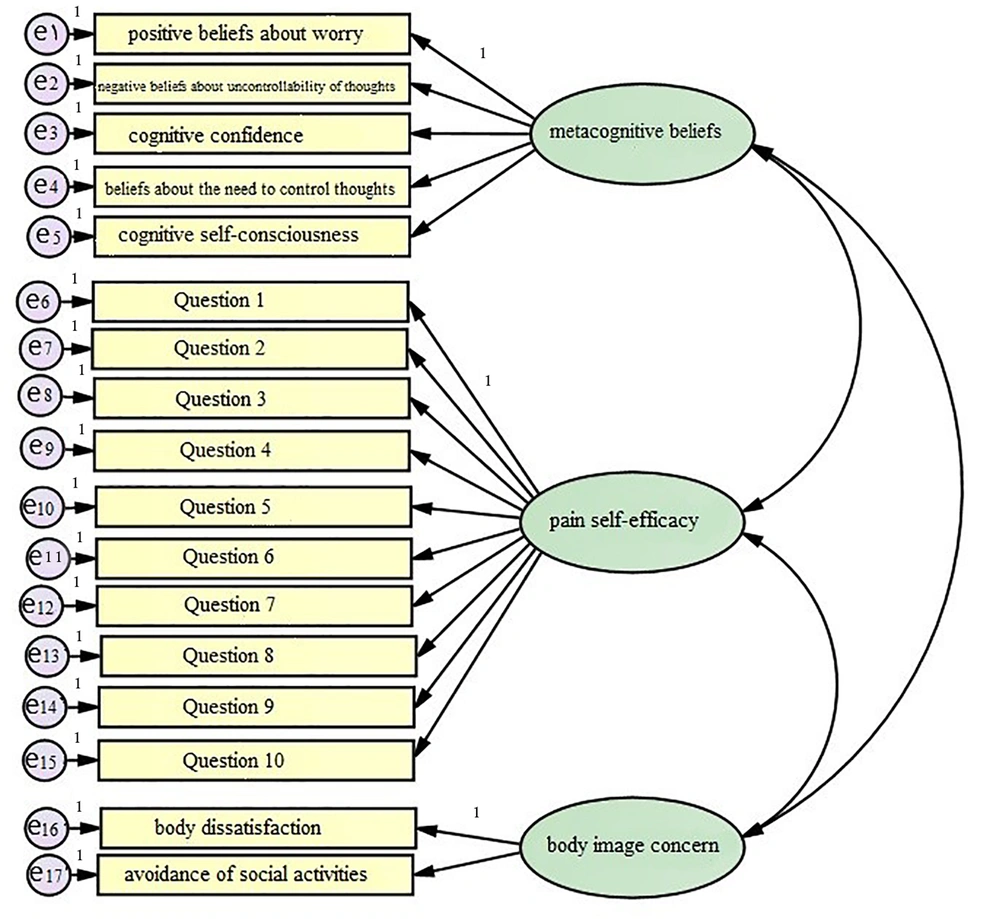
In evaluating the measurement model, the research model is examined using confirmatory factor analysis, which includes the latent variables of metacognitive beliefs, pain self-efficacy, and body image concern, along with explicit variables, as illustrated in Figure 2.
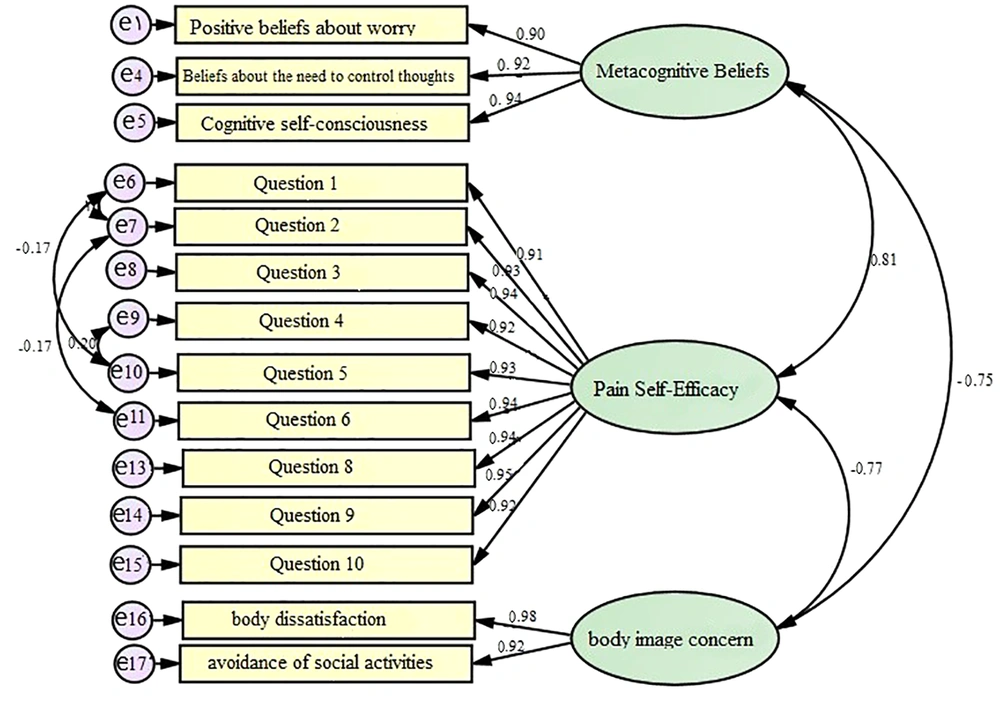
After fitting the model of Figure 2 to the research data, it was found that the variables of thought controllability, cognitive uncertainty, and question 7 of pain self-efficacy were not statistically significant (P > 0.05) and were, therefore, removed from the model. Then, the model was run again, revealing that some fit indices were not within the appropriate range and required modifications. These corrections resulted in covariance freedom between errors related to Questions 1 and 2, Questions 1 and 5, Questions 2 and 6, and Questions 4 and 5 of pain self-efficacy. Figure 3 shows the modified model with factor loadings. The fit indices of this model are as follows:
χ2/df = 3.619, CFI = 0.931, TLI = 0.910, NFI = 0.907, RMSEA = 0.060, 90%CI [0.053, 0.068], SRMR = 0.075
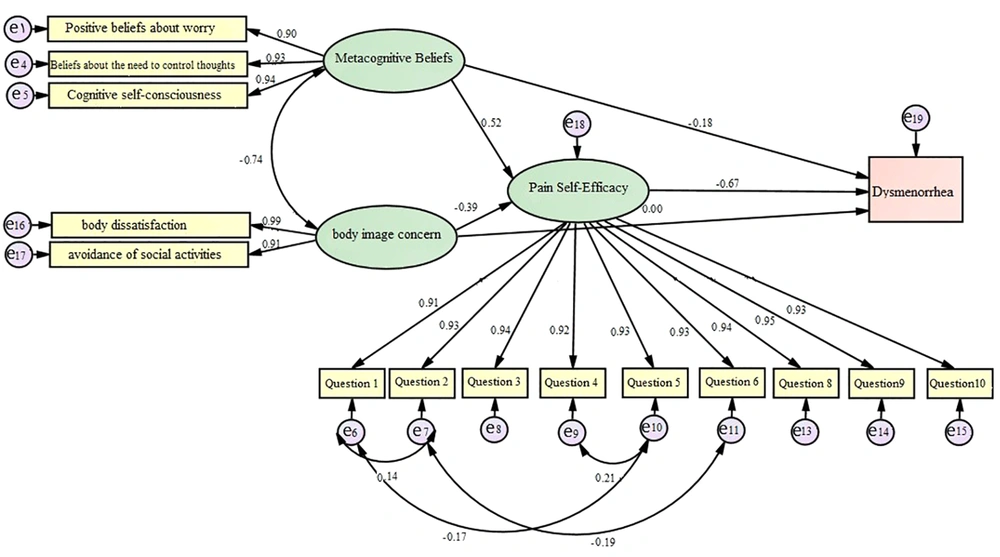
The structural model of the research was examined based on the conceptual model as presented in Figure 4. The fit indices of the structural model in Figure 4 are as follows:
χ2/df = 3.619, CFI = 0.931, TLI = 0.910, NFI = 0.907, RMSEA = 0.060, 90%CI [0.053, 0.068], SRMR = 0.077
Table 3 shows the test of research hypotheses using the results of the research structural model (Figure 4). Notably, two-tailed significance was calculated for indirect effects using the bootstrap method.
| Hypotheses | Coefficient (Lower, Upper) | Two-tailed P-Value | Result |
|---|---|---|---|
| 1. Metacognitive beliefs → Dysmenorrhea | -0.177 (-0.131, -0.031) | <0.001 | Confirmed |
| 2. Body image concern → Dysmenorrhea | 0.004 (-0.140, 0.109) | 0.922 | Rejected |
| 3 | Confirmed | ||
| Metacognitive beliefs → Pain self-efficacy | 0.517 (0.369, 0.640) | <0.001 | |
| Pain self-efficacy → Dysmenorrhea | -0.672 (-0.806, -0.544) | <0.001 | |
| Metacognitive beliefs → Dysmenorrhea (indirect) | -0.348 (-0.471, -0.248) | 0.002 | |
| 4 | Confirmed | ||
| Body image concern → Pain self-efficacy | -0.391 (-0.531, -0.252) | <0.001 | |
| Pain self-efficacy → Dysmenorrhea | -0.672 (-0.806, -0.544) | <0.001 | |
| Body image concern → Dysmenorrhea (indirect) | 0.263 (0.163, 0.382) | 0.008 |
5. Discussion
The present study investigated the relationship between metacognitive beliefs and body image concern on primary dysmenorrhea intensity through the mediating role of pain self-efficacy. The results showed that all fit indices were in the desired range after correction; therefore, the hypothesized model had a good fit with the research population data, confirming the main hypothesis of the research.
This study confirmed the direct effect of metacognitive beliefs and negative correlation on the severity of dysmenorrhea when examining direct pathways. Also, the examination of the indirect pathways showed that the effect of metacognitive beliefs on the severity of dysmenorrhea was mediated by pain self-efficacy, which was in line with the findings of other investigations (25, 26, 28, 29, 36).
In explaining these findings, it can be contended that according to the metacognitive approach, people suffer from chronic pain and distress because their metacognitions lead them to a specific pattern to respond to their internal experiences, evoking negative emotions and reinforcing negative beliefs (22). Psychological interventions are beneficial for many patients with chronic pain. Patients’ beliefs about the symptoms influence psychological and medical outcomes, causes, effects and consequences, duration, control, or treatment of their diseases. As metacognition contributes significantly to intensifying or alleviating pain-related cognitive components, it plays a critical role in the perception of pain in patients experiencing chronic pain (50). Banaeian’s study showed that metacognitive beliefs could predict a total of 61% variance in headache symptoms in women (23).
Failure to recognize emotions results in the inability to control and manage them while affecting thought processes. It can also affect the perception of the pain severity, which is influenced by both emotional and metacognitive factors through disruption of the adaptive thinking process, ultimately leading to the experience of more intense pain (26).
On the other hand, in Bandura's view, self-efficacy reflects an individual’s confidence in their ability to achieve the desired result. Accordingly, pain self-efficacy determines the degree of individual resilience against obstacles, unpleasant experiences, or pain. People with high self-efficacy believe that they can effectively control the events of their lives (a different opinion from those with poor self-efficacy). Thus, self-efficacy can be a critical factor in success or failure in situations such as pain (31).
This result is consistent with studies showing that self-efficacy is related to metacognitive beliefs and pain intensity. Regarding the mediating role of self-efficacy, it can be contended that people with impaired metacognition use strategies that emphasize negative emotions and cognitions to regulate emotions, cognition, and emotional information processing. These dysfunctional strategies predispose individuals to more cognitive deficits, evoking a sense of inefficiency. However, those with the right metacognition use strategies to regulate their emotions and cognition that reduce stress, create positive emotions and mental health, and enable them to take advantage of the existing opportunities. There is a high level of self-efficacy in such conditions, while environmentally stressful situations are not a cause for concern. Therefore, metacognition can be important in preventing the experience of severe pain with the mediating role of self-efficacy (51).
Also, the results of previous studies, including Lotze and Moseley showed that patients with spinal pain reported swollen back, which was only due to concerns about their body images (21), indicating that body image can predict the severity of pain (20). The results of this study showed that the effect of the direct path of body image concern on the severity of dysmenorrhea was not significant, leading to its elimination from the model, which was inconsistent with other studies (6, 17, 22). On the other hand, as we mentioned before, researchers have shown the relationship between self-efficacy and pain intensity. According to Dworkin and Breitbart people with high levels of pain self-efficacy can use the desired resources to reduce pain and discomfort and control pain (30). The results of the present study are also in line with the studies highlighting the role of pain self-efficacy in reducing pain. Also, consistent with previous studies, in examining the indirect path, the effect of body image concerns on the severity of dysmenorrhea mediated by pain self-efficacy was significant (28, 29, 34, 35).
Women with higher levels of satisfaction with their bodies feel more responsible and have more control over them. In addition, self-efficacy is the individuals’ judgment of their competencies. Thus, if women do not meet socially accepted physical criteria, they would feel inadequate, probably leading to lower levels of self-efficacy (35). On the other hand, as mentioned, greater pain self-efficacy can also reduce the severity of pain, which reflects the importance of the mediating role of pain self-efficacy in the relationship between body image concern and the severity of primary dysmenorrhea. The direct relationship between body image concern and the severity of primary dysmenorrhea was significant in previous research. At the same time, the present study found it influential through the mediating role of pain self-efficacy. Body image concerns in early dysmenorrhea may have been affected by mediating variables not considered in previous studies, and this offers a promising field for future research.
5.1. Conclusions
According to the findings of this study, the effect of metacognitive beliefs and body image concern on the severity of primary dysmenorrhea was significant with the mediating role of pain self-efficacy. These findings increase our knowledge of the influential factors in the onset and persistence of physical diseases. Given the role of primary dysmenorrhea in more effective social activities, mental health improvement is expected to enhance girls’ daily activities. This result can be the starting point for designing educational methods to enhance metacognitive beliefs and body image satisfaction among adolescent girls while increasing pain self-efficacy in primary dysmenorrhea with subsequent improvement in their menstrual health and performance.
5.2. Limitations and Suggestions
The sample of the current investigation may not represent the whole population due to the employment of the convenience sampling method. It should be kept in mind that several factors affect the severity of primary dysmenorrhea; therefore, the effect of the intervening variables on the research is not far from expected. Accordingly, future research should be conducted randomly on other populations with different demographic characteristics in the form of interdisciplinary research. Another limitation was the failure to use a screening scale to diagnose psychiatric disorders and diseases that may alter the results, which should be considered in future studies.