1. Background
Comorbidity is a frequent observation of many psychiatric disorders (1). These comorbidities are of significant value in psychiatric evaluations since they can provide a better perspective into the etiological precursors and prognostic outcomes of a disorder (2). Comorbidities are directly associated with reduced social and occupational function (3). Obsessive-compulsive disorder (OCD) is a condition often accompanied by comorbidities such as major depressive disorder (MDD), generalized anxiety disorder (GAD), bipolar disorder, tics, and obsessive-compulsive-related disorders (4). It has been previously demonstrated that OCD can negatively affect the prognosis of accompanying conditions. Such comorbidities are known to be associated with gender differences (5), age of symptom onset (6), response to treatment, social and occupational function (7), and quality of life (8).
One of the most common forms of psychiatric comorbidity is the comorbidity of OCD and GAD (OCD-GAD), which is estimated to occur in approximately 30% of all OCD diagnoses (5, 9, 10). Generalized anxiety disorder is often specifically associated with symptoms such as worry, physical discomfort, and general functionality loss (10). However, discrimination between GAD and OCD symptoms is not easily achievable when compulsive symptoms are not evident or are hidden (11). As known, OCD-GAD comorbidity has notable associations with less intense compulsions and more frequent aggression, hostility, hoarding, checking, doubt, and uncertainty (12). There are numerous phenomenological similarities and differences between OCD and GAD. Both disorders lead to heightened anxiety in response to everyday tasks (13). However, the anxiety associated with GAD is often a result of overemphasized real-life situations (14), while OCD leads to anxiety rooted in the patients' specific obsessive thoughts (15). Nonetheless, treatment with selective serotonin reuptake inhibitors (SSRIs) and cognitive behavioral therapies are effective for both disorders (16, 17).
Despite this, there have been few studies that have specifically focused on the implications of the comorbidity of OCD and GAD in comparison to psychiatric patients who are only diagnosed with OCD. Furthermore, the variables evaluated in this study were not examined in other studies related to GAD.
2. Objectives
Our study aimed to investigate the comorbidity of OCD and GAD. We hypothesized that patients with both conditions who experience therapeutic improvements in their obsessive-compulsive symptoms would not necessarily experience improvements in their GAD symptoms, require additional medications, or demonstrate increased aggression, suicidality, or compulsions.
3. Methods
3.1. Participants
In this cross-sectional study, the participants were patients with OCD referred to two psychiatry clinics (one in Shafa Psychiatry Hospital affiliated with Guilan University of Medical Sciences (GUMS) and the other psychiatry clinic of Dr. Khalkhali and colleagues) in Rasht, Iran. Comprehensive psychiatric evaluations were performed during admission and follow-ups and recorded in the designed electronic files. The files were reviewed, and patients treated for at least two consecutive years were selected if they met the inclusion criteria. The sample selection and data analysis were done from February 2021 to June 2021. Based on the mean difference formula and information from the closest article (18), the required sample size for each group was 62 individuals, considering an alpha of 0.05 and a power of 80%. Finally, 80 individuals in the OCD group and 66 in the OCD-GAD group entered the present study.
The participants were recruited via convenience sampling. The inclusion criteria for this study were a current diagnosis of OCD and OCD-GAD based on the DSM-5-research version (SCID-5-RV) (19) criteria, age of 18 years or older, moderate or higher severity of OCD (a score of 16 or higher on the Yale-Brown Obsessive Compulsive Scale) (20), no standard pharmacologic treatment or psychotherapy for at least three months prior to admission to the clinic, at least two years of follow-up in the mentioned clinics, and no other comorbid psychiatric disorders. The exclusion criteria included dementia, bipolar disorder, intellectual disability disorder, attention deficit hyperactivity disorder (ADHD), schizophrenia spectrum and other psychotic disorders, alcohol, opioids, cannabis or stimulants-use disorders, serious physical ailments, or organic mental disorder.
3.2. Data Collection
We reviewed the patients' files for the symptoms and severity of OCD, function evaluation, treatment response for OCD, and comorbid psychiatric disorders. Patients were divided into two groups based on their comorbidity: OCD patients (N = 80) and OCD-GAD patients (N = 66). Based on the treatment plan, regular evaluations were done in our clinics. We chose the evaluations carried out at 3 discrete timeframes, 3 months apart. Obsessive-compulsive symptoms and severity were assessed at the initial examination, while the number of distinct medications in the therapeutic regimen of the patients was recorded at the final follow-up (6 months after initial evaluations). A psychiatrist performed all treatments in both clinics. A clinical psychologist only conducted psychoeducational sessions for all patients. No other psychotherapy methods were used to treat the patients of the two groups. Treatments were based on standard usual treatment protocols for OCD and GAD (21, 22). Additional pharmacologic treatment for anxiety disorder was not considered.
The following tools were used to collect symptomatic and diagnostic information about the participants.
3.2.1. Hamilton Anxiety Rating Scale
Hamilton Anxiety Rating Scale (HAM-A), which is a semi-structured test with 14 parts to evaluate and follow up on anxiety levels during the therapy. Each subcategory ranges from 0-4, and the final score ranges from 0 to 56. In the study by Maier et al., the reliability of the total score of HAM-A was 0.74 (23). Also, in Iran, the test-retest reliability of the scale was reported to be 0.81 (24). The HAM-A score was estimated in the OCD-GAD patients on all the 3 different occasions.
3.2.2. Yale-Brown Obsessive-Compulsive Scale
Yale-Brown Obsessive-Compulsive Scale (Y-BOCS), which includes a symptom checklist and two subscales for the intensity of obsessive and compulsive symptoms. It has 10 items ranging from 0 (no symptom) to 4 (extreme severity) and a maximum score of 40 (20 for obsessions and 20 for compulsions). The reliability of this scale was acceptable for measuring the severity of illness in OCD patients (20). In the Iranian population, it is highly sensitive to therapeutic improvements with Cronbach's α coefficients of 0.97 and 0.95 and split-half correlation coefficients of 0.93 and 0.89 for the symptom checklist and the intensity scale, respectively. The reliability coefficient of the test-retest has been reported as 0.99 (25). The Y-BOCS score was evaluated at all 3 sessions for both groups.
3.2.3. Global Assessment of Functioning
Global Assessment of Functioning (GAF), which was used to evaluate the severity of anxiety and its effects on personal functionality, with a scoring range of 0-100. In the simultaneous incorporation of several similar scales, GAF has demonstrated notable validity and reliability (11, 26). The GAF score was documented for both groups at the first and last (6-month) sessions.
3.2.4. Brief Psychiatric Rating Scale
Brief Psychiatric Rating Scale (BPRS), which is often used in clinical and investigational settings as a measuring tool for 24 subcategories of psychiatric symptoms, ranging from depression to anxiety and schizophrenia. The interviewer assigns a 7-point severity scale ranging from 'not present' to 'extremely severe' for each subcategory (27). The internal validity of this tool is 0.809 (28). In our study, suicidality and hostility were indicated by a score of 4 or higher in the related BPRS subcategory.
3.2.5. Structured Clinical Interview for DSM-5 Disorders, Research Version
Structured Clinical Interview for DSM-5 Disorders, Research Version (SCID-5-RV), which was used by the clinician to diagnose OCD, GAD, and other comorbid disorders, based on the diagnostic and statistical manual of mental disorders (DSM-5). The SCID-5 has demonstrated adequate internal consistency (0.95 - 0.99), retest reliability (0.60 - 0.79), and Cohen's kappa inter-rater reliability (0.57 - 0.72), as well as a satisfactory agreement between interviewers (19).
3.3. Data Analysis
The data were analyzed using SPSS software, version 20 (IBM Statistics, Chicago, IL). Quantitative data were described using mean ± standard deviation (SD). The Shapiro-Wilks test was used to determine the normality of the distribution for quantitative variables. The variables were evaluated using a t-test in the case of normal distribution and a Mann-Whitney test in the case of non-normal distribution. The chi-square test was used to compare the frequency of categorical variables between the two study groups (OCD and OCD-GAD). Repeated-measures ANOVA test assessed the changes in quantitative and normal variables over time. The alpha level was 0.05 for all tests.
3.4. Ethical Considerations
All participants declared their written informed consent. The authors ensured the confidentiality and anonymity of the data by assigning sequential codes to the participants. This study was approved by the Ethics Committee of Guilan University of Medical Sciences (Ethical Code: IR.GUMS.REC.1397.301).
4. Results
Out of the 146 participants, 80 only had OCD, while 66 had OCD-GAD. The participants had a mean age of 39.13 ± 73.85 years, and 107 (73.3%) were female. The OCD and OCD-GAD groups showed no significant difference in age, sex, marital status, and years of education. However, the OCD-GAD group had a significantly higher employment rate than the OCD group (83.3% vs. 67.5%, P = 0.029). Table 1 compares the baseline characteristics of OCD and OCD-GAD patients. The frequencies of symmetry (P = 0.014), hoarding (P = 0.034), taboo (P = 0.023), and aggressive (P = 0.002) obsessive-compulsive symptoms were significantly higher in the OCD group.
| Characteristics | Total (N = 146) | OCD (N = 80) | OCD-GAD (N = 66) | P-Value |
|---|---|---|---|---|
| Age, y | 39.13 ± 73.85 | 38.14 ± 24.67 | 41.12 ± 63.59 | 0.146 b |
| Education, y | 10.5 ± 39.11 | 10.5 ± 64.34 | 10.40 ± 8.48 | 0.513 b |
| Gender | 0.172 c | |||
| Female | 107 (73.3) | 55 (68.8) | 52 (78.8) | |
| Male | 39 (26.7) | 25 (31.2) | 14 (21.2) | |
| Job status | 0.029 c | |||
| Employed | 109 (74.7) | 54 (67.5) | 55 (83.3) | |
| Unemployed | 37 (25.3) | 26 (32.5) | 11 (16.7) | |
| Marital status | 0.056 c | |||
| Single | 52 (35.6) | 34 (42.5) | 18 (27.3) | |
| Married | 94 (64.4) | 46 (57.5) | 48 (72.7) | |
| Frequency of obsessive-compulsive symptoms | ||||
| Contamination | 62 (77.50) | 46 (69.70) | 0.285 b | |
| Symmetry | 35 (43.80) | 16 (24.20) | 0.014 b | |
| Hoarding | 8 (10.00) | 1 (1.50) | 0.034 b | |
| Taboo | 15 (18.80) | 4 (6.10) | 0.023 b | |
| Aggression | 20 (25.00) | 4 (6.10) | 0.002 b | |
| Residual | 24 (30.00) | 17 (25.80) | 0.570 b |
Baseline Characteristics of Obsessive-Compulsive Disorder (OCD) and OCD-Generalized Anxiety Disorder (OCD-GAD) Groups a
Table 2 compares the study outcomes throughout the study between OCD and OCD-GAD groups. As the table implies, the two groups had no significant difference in BPRS domains of suicidality and hostility, neither at the baseline nor after 6 months. Moreover, over half of the patients in both groups (55.70% in OCD and 67.70% in OCD-GAD) had received only one medication at 6 months, and the number of prescribed medications was not significantly different between the two groups. Based on the standard treatment protocols, SSRIs are the first-line treatment of OCD. They can be augmented with a SAD. The third agent is a glutamatergic drug (Memantine). Therefore, the number of medications means more augmentation strategies.
| Feature | OCD (N = 80) | OCD-GAD (N = 66) | P-Value | ||||
|---|---|---|---|---|---|---|---|
| Initial | 3-Month | 6-Month | Initial | 3-Month | 6-Month | ||
| BPRS | |||||||
| Suicidality | 11 (13.80) | - | 10 (12.50) | 9 (13.80) | - | 8 (12.30) | P0 = 0.987 b, P6 = 0.972 b |
| Hostility | 34 (43.00) | - | 32 (40.50) | 21 (32.30) | - | 21 (32.30) | P0 = 0.187 b, P6 = 0.310 b |
| Medications | |||||||
| 1 | - | - | 44 (55.70) | - | - | 42 (67.70) | 0.152 b |
| 2 | - | - | 20 (25.30) | - | - | 15 (24.20) | |
| 3 | - | - | 15 (19.00) | - | - | 5 (8.10) | |
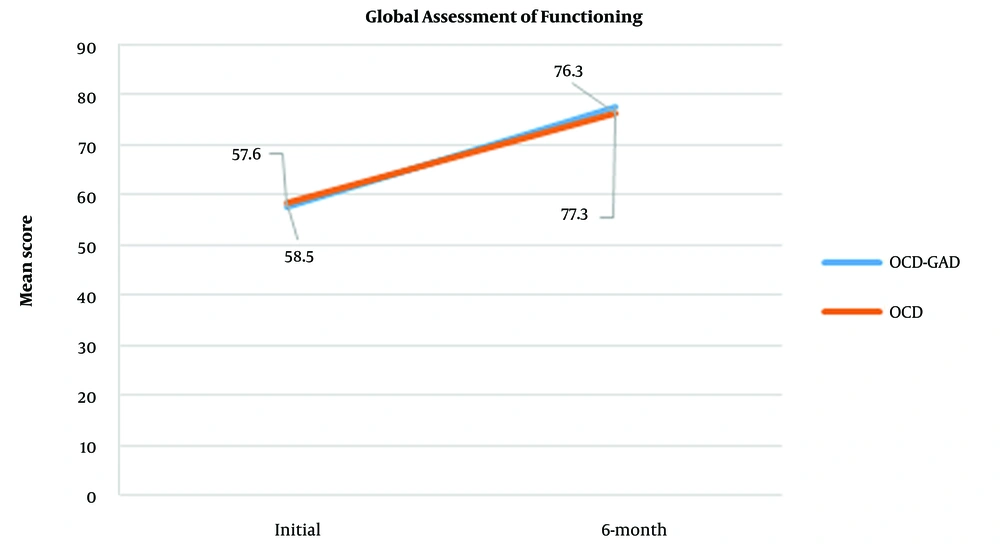
| GAF | 58.50 ± 26.58 | - | 76.30 ± 93.91 | 57.60 ± 55.61 | - | 77.30 ± 93.91 | - |
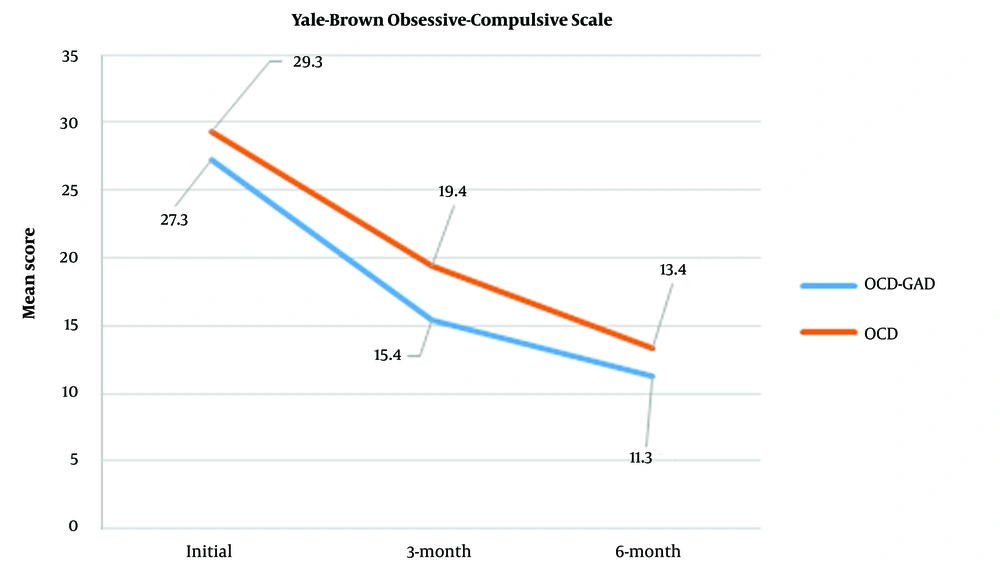
| Total Y-BOCS | 29.30 ± 20.78 | 19.40 ± 5.75 | 13.40 ± 53.03 | 27.30 ± 60.46 | 15.40 ± 59.73 | 11.30 ± 98.53 | < 0.0001 c |
| HAM-A | - | - | - | 32.60 ± 87.15 | 16.14 ± 78.48 | 11.30 ± 10.91 | < 0.0001 c |
Comparison of Study Outcomes Between Obsessive-Compulsive Disorder (OCD) and OCD-Generalized Anxiety Disorder (OCD-GAD) Groups a
The GAF evaluations were carried out on two different occasions, and the results were assessed using a repeated-measures analysis of variance. Pillai's trace multivariate test demonstrated a notable increase in GAF scores over time in both groups (P < 0.0001) (Figure 1). However, the increase in the GAF value was not statistically different between the two groups (P = 0.283) (Table 2).
As shown in Table 2 and Figure 2, there was a significant decline in Y-BOCS scores in both groups over time (P < 0.0001), and the YBOCS score was higher in the OCD group than in the OCD-GAD group (P < 0.0001). In addition, the severity of the symptoms decreased more in the OCD-GAD group during the first 3 months (P = 0.006).
Moreover, the HAM-A scores were measured at 3 different time points (baseline, 3-month follow-up, and 6-month follow-up) in the OCD-GAD group. In the repeated-measures analyses, Pillai's Trace multivariate test showed that anxiety symptoms notably decreased over time (P < 0.001).
5. Discussion
This study aimed to evaluate the impact of GAD comorbidity on OCD. Only Abramowitz and Foa have performed a study on OCD with and without GAD comorbidity, mainly focused on worries and obsessions (18). In contrast, we investigated the effects of GAD on the clinical course and prognosis of OCD. The differentiation of GAD from OCD is a seemingly straightforward task when compulsions are easily identifiable; however, in the cases presenting little to no compulsive behaviors, this differentiation becomes a formidable endeavor (18, 29, 30). Health-related GAD is associated with symptoms such as excessive cleaning and fear of contamination, which are not readily distinguishable from the compulsions associated with OCD. Consequently, thorough evaluations are required to minimize the hardships of arriving at a definitive diagnosis. In the current study, participants were not only assessed by standardized tests and scales, but they were also individually interviewed to increase the accuracy of the final diagnosis.
Our study found no difference in demographic features and clinical variables between the OCD and OCD-GAD groups. Most notably, our results indicated that medical treatment significantly decreased obsessive thoughts in both groups. It should be mentioned that the severity of OCD was lower in the OCD-GAD group than in the OCD group, which remained unchanged throughout the course of treatment. In comparison, other studies reported that the presence of a comorbid disorder was often accompanied by a higher severity of OCD (7, 31). Our findings suggest that GAD comorbidity with OCD does not necessarily result in the disorder's intensification nor affect the total response to the treatment. Furthermore, our results signify that comorbidities do not necessarily intensify the disorders. Similarly, Abramowitz and Foa (18) reported that the severity of OCD symptoms is not increased when GAD is present, which does not contradict our results.
It has been demonstrated that one out of ten OCD patients attempts suicide (32). Studies also suggest that a GAD diagnosis leads to a higher rate of suicidal behavior (33) and aggression (34) in these patients than in the normal population. The risk of suicidality in individuals with OCD has been shown to vary greatly in terms of prevalence (35). This is not surprising, as studies have found that the risk of suicide is associated with more severe obsessions and less intense compulsions (32). As a result, the risk of suicide can vary depending on the specific symptoms of OCD in each case. It is also commonly believed that either depression or bipolar disorder comorbidity with OCD might commence a higher incidence of suicide (32). Contrary to this belief, our results showed that suicide and aggression rates are not higher in GAD-OCD patients than in OCD patients. Even so, it is apparent that GAD may increase suicidality and aggression in the normal population, but as OCD-GAD reduces compulsions in OCD patients, the interaction of these effects does not lead to an over-intensification of suicidality and aggression in OCD-GAD patients. Furthermore, some reports suggest that comorbid anxiety in OCD patients is a possible protective factor against suicidal thoughts and attempts (32). This occurrence could potentially be associated with the harm avoidance by-product of anxiety symptoms, ultimately improving OCD prognosis regarding suicidality.
We found that the aggression, taboo, and ordering-counting symptoms were notably more intense in the OCD group than in the OCD-GAD group. Different studies have reported other aspects of this comorbidity, such as indecisiveness, extreme pathological responsibility, and excessive worries in OCD-GAD patients (18). Nonetheless, similar to our findings, a large-scale report has also shown that symptoms such as ordering are more frequent and intense in OCD patients without comorbidities (9). Even so, there are major inconsistencies between the reported results in comorbid studies (18, 36, 37), indicating a large gap in the current understanding of the complexities of OCD comorbidities.
Nonetheless, it is known that in almost all cases, comorbidity of more than two disorders usually results in an impeded response to medical treatment and hence, the need for a multidrug regimen. Interestingly, however, our results are inconsistent with this belief. In other words, we found that GAD does not deteriorate the course of treatment in OCD patients and does not necessitate more discrete medications. Furthermore, we found that the response rate was much higher in the GAD-OCD group at the beginning of the treatment; this difference gradually decreased with time. This inconsistency might have been due to the lower severity of obsessive-compulsive symptoms in the OCD-GAD group than in the OCD group; additionally, SSRIs are the first treatment choice for both GAD and OCD groups. The alignment of the treatment plans for both parts of the OCD-GAD comorbidity and the lessened symptoms may have had a pivotal role in the observed medication results, such that OCD-GAD does not appear to impact the course of treatment negatively. In contrast, some comorbidities with counteractive medications (i.e., psychotic and bipolar disorders) result in a diminished response to treatment (38, 39).
Our results indicated that following therapies, obsession, and anxiety levels significantly decreased with time; however, the rate of decline was not consistent at all time frames (Y-BOCS scores declined more at the first follow-up while HAM-A anxiety declined more at the second follow-up). Interestingly, however, we anecdotally found that some OCD-GAD patients who had improved obsessive symptoms following therapy were dissatisfied with the effects of therapy on their anxiety. This may hint at the presence of a GAD subtype, accompanied by OCD, with distinct clinical presentations and minimal response to treatments; consequently, further studies might aid in evaluating such possibilities.
As a chronic disorder, OCD begins in adolescence, and patients seek treatment at different time intervals from the onset of the disease and receive different treatments. Due to the large variety of treatments, we could not find a suitable model to compare previous treatments and limited ourselves to not receiving the standard treatment three months before admission and the moderate severity of the disorder. Based on the standard treatment protocols, SSRIs are the first-line treatment of OCD. They can be augmented with SADs. The third agent is a glutamatergic drug. Therefore, the number of medications shows the number of augmentation strategies. All patients received a standard dosage of SSRIs for the treatment of OCD. As the effect size of SSRIs was similar in review studies, the types of SSRIs were not considered.
A limiting factor of our study was the lack of a GAD-only group, which hindered further evaluations on the impacts of OCD-GAD comorbidity. Furthermore, our study group only consisted of outpatients seeking long-term treatment plans. Therefore, the results cannot be easily generalized to all individuals affected by the condition. Lastly, very few studies have reported on the same variables of the OCD-GAD comorbidity, which limited the extent of comparative consideration of our results. Future longitudinal studies are recommended instead of our cross-sectional method to fully appreciate the clinical significance of OCD-GAD comorbidity.
5.1. Conclusions
Our study demonstrated no negative effect of GAD comorbidity on the prognosis of OCD patients. Nonetheless, our findings do not suggest that an OCD-GAD diagnosis is a distinct subcategory of clinical disorders, and it may not be beneficial to treat it as such. Further investigations are indicated to evaluate the clinical significance of OCD-GAD comorbidity.