1. Background
Acceptance and commitment therapy (ACT) holds a special position among third-wave behavioral therapies due to its wide therapeutic applications and extensive research (1). Research has shown that ACT significantly improves symptoms of various psychological disorders, including obsessive-compulsive and anxiety disorders (2), co-existing anxiety and depression in bipolar disorder (3), borderline personality disorder (4), hallucinations in psychotic disorders (5), and even psychological symptoms related to physical diseases such as chronic pain (2) and body image issues in obesity (6).
Acceptance and commitment therapy aims to increase psychological flexibility in clients to help them deal with problems (7). Psychological flexibility refers to the ability to engage with the present moment and to change or persist in behavior when moving towards valued life goals. It includes the ability to differentiate oneself from inner psychological experiences (8). The opposite of psychological flexibility is psychological inflexibility, which is noted in the pathology of various psychological disorders and problems (9). According to the ACT psychopathology model, six components contribute to psychological inflexibility, with cognitive fusion being an important one (10). Gillanders et al. (11) define cognitive fusion as clinging to thoughts and the tendency to perform over-regulated and cognitively influenced behaviors. Based on this definition, Gillanders et al. (11) designed the Cognitive Fusion Questionnaire (CFQ).
Cognitive fusion plays a role in the maintenance of obsessive-compulsive disorder and anxiety disorders (12), depression (13), psychotic disorders (4), personality disorders (10), PTSD (14), self-stigma (15), obesity (16), and eating disorders (17).
Over the past decades, various tools have been developed to measure cognitive fusion, including the Automatic Thoughts Questionnaire (18), the Avoidance and Fusion Questionnaire for Youth (19), the Believability of Anxious Feelings and Thoughts Scale (20), and the Drexel Defusion Scale (21). Each of these questionnaires has limitations for measuring cognitive fusion. For example, the ATQ measures cognitive content related to depression and is used to assess the effect of cognitive therapy, making it limited as a general measure of cognitive fusion. The AFQ measures multiple processes based on ACT, so it is not a separate measure of cognitive fusion. The BAFT provides a limited concept of cognitive fusion specific to anxiety disorders. The DDS has shortcomings such as hypothetical or imaginary events, with questions that measure those specific situations. Due to these limitations, Gillanders et al. (11) created the CFQ. The CFQ is a 7-item self-report questionnaire based on the theoretical foundations of ACT, designed to measure cognitive fusion (22). The psychometric properties of the CFQ have been investigated and validated in various countries. For example, Soltani et al. (23) validated the Persian version of the CFQ in a non-clinical sample. Additionally, some studies have confirmed the validity and reliability of the CFQ in medical conditions (24, 25).
Like previous tools, the CFQ also has limitations. The general instructions and wording of the CFQ items are not sensitive to cognitive fusion over short periods. Therefore, the CFQ does not provide accurate results for cognitive fusion in experimental studies conducted over short periods or in laboratory environments (26). Despite many studies conducted on the CFQ, research in experimental settings did not use this questionnaire (26). For this reason, a state version of the CFQ (SCFQ) was designed by Bolderston et al. (26). The SCFQ was modified for experimental work and laboratory environments. This questionnaire has 7 items answered on a 7-point Likert scale. It demonstrated good reliability and validity in Bolderston et al.'s (26) study. Many studies have been conducted on tools for measuring cognitive fusion, but some research shows that these tools have not yet been used to measure cognitive fusion in people with symptoms of mental disorders (26, 27).
Based on the research background, there are no studies using the CFQ and SCFQ in an Iranian clinical sample, and the present study is the first to do so.
2. Objectives
The purpose of the current study is to investigate the psychometric properties of the Persian versions of the Trait and State Cognitive Fusion Questionnaires in various mental disorders.
3. Methods
3.1. Participants
A total of 200 individuals with mental disorders were recruited via convenience sampling from the Ebnesina and Hafez hospital wards and clinics in Shiraz during 2020 - 2021. Based on Munro’s statistical methods for health care research (28), a ratio of at least 10 participants for each variable is desirable to generalize the sample to a larger population. We selected 200 subjects according to the number of variables and the possibility of generalization. Two psychiatric residents visited different wards and psychiatry clinics to explain the purpose of the research to the individuals. The research field of cognitive fusion in people with mental disorders is in its infancy, and no research has yet shown that people with different psychiatric disorders have varying levels of cognitive fusion. Therefore, researchers did not select a specific type of these patients.
Individuals who wished to participate were included in the study. Inclusion criteria were as follows: Aged 18 - 65 years, diagnosed with a mental disorder according to a psychiatrist's diagnosis, and having at least a fifth-grade education. Four patients did not make a reasonable attempt to complete the questionnaires (i.e., less than 80% of items completed).
3.2. Measures
3.2.1. Cognitive Fusion Questionnaire
The 7-item CFQ assesses an individual’s tendency to be psychologically entangled with the form or content of their own thoughts such that it dominates their behavior (11). The CFQ is rated on a 7-point Likert scale (1 = never true to 7 = always true), with higher scores indicating greater cognitive fusion. The CFQ has demonstrated good reliability and validity in both Iranian and English-speaking samples (11, 23). In the current study, the Cronbach's alpha was 0.90.
3.2.2. State Cognitive Fusion Questionnaire
The 7-item SCFQ is based on the CFQ but modified to function as a state measure of cognitive fusion. The SCFQ is rated on a 7-point Likert scale (1 = never true to 7 = always true), with higher scores indicating greater cognitive fusion. This questionnaire does not have any subscales. The CFQ was first translated into Persian and standardized in a non-clinical sample in Iran (23). We modified the items to address fusion in the present moment rather than in general. The instructions asked participants to indicate how true each statement is for them at this moment (for example, item four of the CFQ—I struggle with my thoughts—was changed to I am struggling with my thoughts). The CFQ is used for general situations, while the SCFQ is used for the present moment. The SCFQ has demonstrated good reliability and validity in English-speaking samples (26).
3.2.3. Acceptance and Action Questionnaire-Second Version
The 10-item Acceptance and Action Questionnaire-Second Version (AAQ-II) assesses an individual’s tendency to engage in experiential avoidance of negative and unwanted thoughts and feelings. Acceptance and Action Questionnaire-Second Version items are rated on a 7-point Likert scale (1 = never true to 7 = always true), with higher scores indicating less experiential avoidance. The AAQ-II has demonstrated good reliability and validity in both Iranian and English-speaking samples (29). In the current study, the Cronbach's alpha was 0.78.
3.2.4. Depression Anxiety Stress Scales
The 21-item short form of the Depression Anxiety Stress Scales (DASS) is rated on a 4-point Likert scale (0 = did not apply to me at all to 3 = applied to me very much, or most of the time) and assesses depression, anxiety, and stress. Higher scores on the DASS reflect higher levels of depression, anxiety, and stress (30). The DASS has demonstrated good reliability in Iranian samples (31). In the current study, the Cronbach's alpha was 0.95.
3.2.5. Connor-Davidson Resilience Scale
The 25 items of the Connor-Davidson Resilience Scale (CD-RISC) are rated on a 5-point Likert scale (0 = not true at all to 4 = true nearly all the time) and assess stress coping ability. For the CD-RISC, respondents are asked to read each item and select the option that best reflects how they have felt over the past month (e.g., “able to adapt to change”). Higher scores on the CD-RISC reflect greater resilience. The CD-RISC has demonstrated good reliability and validity in English-speaking samples (32) and has exhibited good reliability and validity in its Iranian translation [e.g., Cronbach’s alpha = 0.93; see Jowkar (33)]. In the current study, the Cronbach's alpha was 0.95.
3.2.6. The Satisfaction with Life Scale
The 5 items of the Satisfaction with Life Scale (SWLS) are rated on a 7-point Likert scale (1 = strongly disagree to 7 = strongly agree) and assess global life satisfaction. Respondents are asked to indicate their agreement by placing the appropriate number (e.g., “the conditions of my life are excellent”). Higher scores on the SWLS reflect greater life satisfaction (18). The SWLS has demonstrated good reliability and validity in both English-speaking and Iranian samples (18, 20). In the current study, the Cronbach's alpha was 0.88.
3.2.7. Data Analysis Method
In this research, the psychometric properties were evaluated through confirmatory factor analysis using the first-order confirmation method, as well as convergent and divergent validity. Reliability and internal consistency were assessed with Cronbach's alpha and the item-total correlation method. Confirmatory factor analysis was performed using SPSS and LISREL to confirm the structure of the CFQ and SCFQ. Skewness and kurtosis were between -2 and +2, which are considered acceptable for proving normal univariate distribution (34). The goodness-of-fit indices assessed included CFI, TLI, RMSEA, SRMR, and normed χ2. According to Gillanders et al. (11), convergent validity should be tested using a construct that positively correlates with cognitive fusion. Therefore, the CFQ, DASS (measuring anxiety, stress, and depression), and CD-RISC were used. For divergent validity, constructs that have a negative correlation with cognitive fusion were used, including the AAQ-II and SWLS.
3.2.8. Ethical Consideration
This research was registered with the Ethics Committee of Shiraz University of Medical Sciences (IR.SUMS.REC.1399.818). The ethical issues observed in this research included: Freedom to participate in the research, non-disclosure of demographic information, freedom to leave the research, full knowledge of the research purpose, answers to any questions within the scope of the research, and explanations about cognitive fusion.
4. Results
The study sample consisted of 196 individuals (59% female; mean ± SD of age: 34.16 ± 1.04 years; education: 13.12 ± 3.11 years). The majority of participants were in the ward, while about 15% attended the clinic. Participants had various diagnoses, including number (%) of bipolar disorder: 42 (21.4%), depressive disorder: 58 (29.6%), schizophrenia and psychotic disorders: 32 (16.3%), adjustment disorder: 26 (13.3%), cluster B personality disorder: 11 (5.1%), anxiety disorders: 12 (6.1%), obsessive-compulsive disorder: 4 (2%), other mental disorders: 8 (4.1%), and unclear diagnoses: 3 (1.5%) at the time of hospitalization.
4.1. Confirmatory Factor Analysis of CFQ and SCFQ
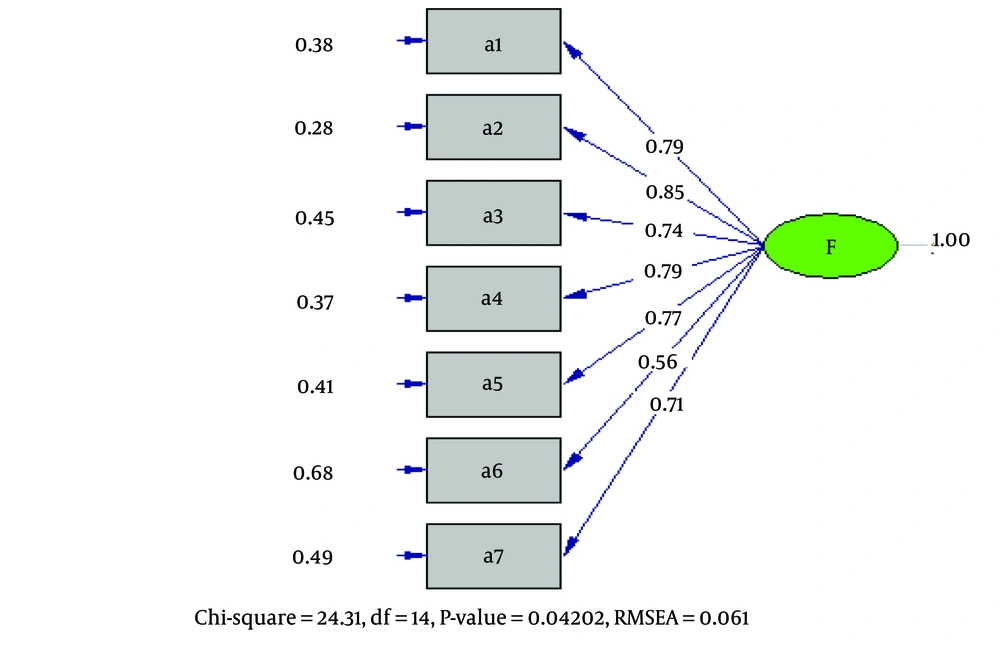
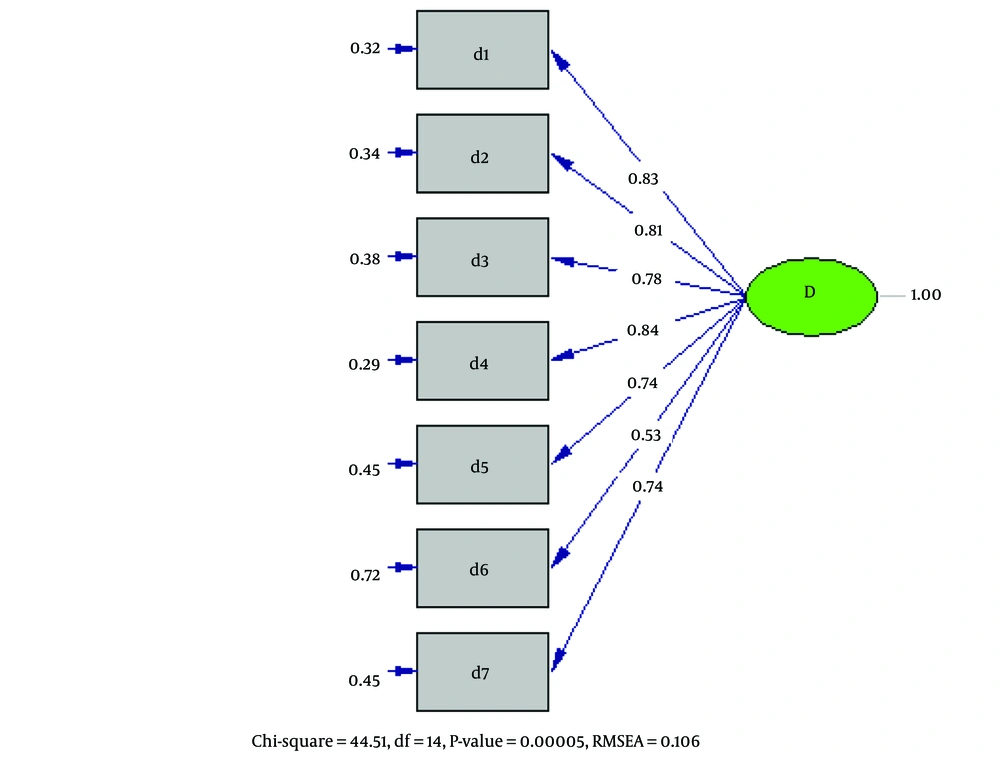
As shown in Table 1, the model fit indices for the CFQ are excellent. Specifically, the CFI and TLI are > 0.95, the SRMR is < 0.08, and the RMSEA is <.06. Moreover, the Normed χ2 is < 5, indicating an acceptable level of model fit based on Wheaton et al.'s cut-off recommendations (35). The model fit indices for the SCFQ are also excellent, with the CFI and TLI > 0.95, the SRMR < 0.08, and the normed χ2 < 5. Although the RMSEA is > 0.06, this is acceptable based on Fan et al.'s suggestion (36). Based on previous Iranian non-clinical samples and existing literature, we predicted that the CFQ and its new version would have a single factor. The results show that both the CFQ (Table 1 and Figure 1) and the SCFQ (Table 1 and Figure 2) have a unifactorial structure with excellent model fit across all fit indices.
| Variables | χ2 | df | P-Value | Normed χ2 | CFI | TLI | RMSEA | SRMR |
|---|---|---|---|---|---|---|---|---|
| CFQ | 24.31 | 14 | 0.042 | 1.73 | 0.99 | 0.99 | 0.061 | 0.028 |
| SCFQ | 44.51 | 14 | 0.00005 | 3.17 | 0.98 | 0.97 | 0.106 | 0.037 |
4.2. Norms and Internal Consistency of CFQ and SCFQ
The mean and standard deviation for the CFQ were 25.98 and 12.40, respectively. The mean and standard deviation for the SCFQ were 25.59 and 12.43, respectively. Cronbach’s alphas for both the CFQ and SCFQ were 0.90, indicating excellent internal reliability (37). The CFQ and SCFQ had McDonald's omega (ω) of 0.89 and 0.90. Table 2 provides more details about internal consistency and loading.
| Items | Loading | Mean ± SD | Correlated Whole Correction | Cronbach’s Alpha by Removing Questions | Scale’s Mean Score with Deleted Items | Squared Multiple Correlation |
|---|---|---|---|---|---|---|
| Trait | ||||||
| 1 | 0.79 | 4.50 ± 2.29 | 0.73 | 0.88 | 21.49 | 0.57 |
| 2 | 0.85 | 3.61 ± 2.25 | 0.79 | 087 | 22.37 | 0.66 |
| 3 | 0.74 | 3.61 ± 2.11 | 0.70 | 0.88 | 22.37 | 0.51 |
| 4 | 0.79 | 3.46 ± 2.22 | 0.74 | 0.88 | 22.52 | 0.57 |
| 5 | 0.77 | 3.83 ± 2.36 | 0.72 | 0.88 | 22.15 | 0.55 |
| 6 | 0.56 | 3.12 ± 2.20 | 0.54 | 0.90 | 22.86 | 0.30 |
| 7 | 0.71 | 3.85 ± 2.29 | 0.69 | 0.88 | 22.13 | 0.50 |
| State | ||||||
| 1 | 0.83 | 4.47 ± 2.33 | 0.77 | 0.88 | 21.12 | 0.64 |
| 2 | 0.81 | 3.53 ± 2.21 | 0.74 | 0.88 | 22.05 | 0.63 |
| 3 | 0.78 | 3.47 ± 2.05 | 0.74 | 0.88 | 22.12 | 0.59 |
| 4 | 0.84 | 3.45 ± 2.16 | 0.79 | 0.88 | 22.14 | 0.64 |
| 5 | 0.74 | 3.81 ± 2.30 | 0.71 | 0.89 | 21.78 | 0.54 |
| 6 | 0.53 | 3.10 ± 2.17 | 0.51 | 0.90 | 22.53 | 0.29 |
| 7 | 0.74 | 3.79 ± 2.40 | 0.71 | 0.89 | 21.79 | 0.53 |
4.3. Convergent Validity of CFQ and SCFQ
Table 3 shows the correlations between the CFQ and SCFQ with other constructs. The CFQ had a strong positive correlation with the SCFQ. There was also a moderate positive correlation between both the CFQ and SCFQ with the CD-RISC. The two versions of the CFQ showed moderate to strong positive correlations with measures of psychopathology (depression, anxiety, and stress) and negative correlations with experiential avoidance (AAQ-II). Finally, there was a moderate positive correlation between both the CFQ and SCFQ with life satisfaction (SWLS). These findings indicate the convergent validity of the CFQ and SCFQ.
| Variables | AAQ-II | CD-RISC | DASS-T | DASS-D | DASS-A | DASS-S | SWLS | CFQ |
|---|---|---|---|---|---|---|---|---|
| CFQ | -0.69 | 0.43 | 0.69 | 0.65 | 0.59 | 0.69 | -0.43 | 1 |
| SCFQ | -0.70 | 0.44 | 0.71 | 0.66 | 0.62 | 0.70 | -0.38 | 0.87 |
Abbreviations: CFQ, Cognitive Fusion Questionnaire; SCFQ, State Cognitive Fusion Questionnaire; AAQ-II, Acceptance and Action Questionnaire-Second Version; CD-RISC, Connor-Davidson Resilience Scale; DASS-T, Depression Anxiety Stress Scales- Total; DASS-D, Depression Anxiety Stress Scales-Depression Subscale; DASS-A, Depression Anxiety Stress Scales-Anxiety Subscale; DASS-S, Depression Anxiety Stress Scales-Stress Subscale; SWLS, Satisfaction with Life Scale.
a All correlations significant at P < 0.001 level (2-tailed).
5. Discussion
The SCFQ and CFQ have excellent Cronbach's alpha. In this study, Cronbach's alpha was 0.90. In the study by Bolderston et al. (26), reliability with Cronbach's alpha was 0.95. The convergent validity of the SCFQ, in correlation with the CFQ, was 0.87, indicating a high correlation between these two questionnaires. This suggests that both tools measure the same construct. In Bolderston et al.'s study (26), the correlation between the CFQ and SCFQ was 0.78. The difference in correlation between the two studies may be due to differences in the sample. The current research was conducted on a clinical sample, and considering that cognitive fusion in people with mental disorders is higher than in those without symptoms of mental disorders (10), it can be concluded that the CFQ and SCFQ are likely to yield more similar results in people with mental disorders than in those without such symptoms.
Additionally, the correlation between the SCFQ and symptoms of depression, anxiety, and stress in the DASS was 0.66, 0.62, and 0.70, respectively, and 0.71 in correlation with the overall scale Depression Anxiety Stress Scales- Total (DASS-T), indicating a high correlation between these two questionnaires. The positive correlation of the SCFQ with the DASS confirms the relationship between cognitive fusion and pathological symptoms in people with mental disorders (38). The correlation between the CFQ and symptoms of depression, anxiety, and stress in the DASS, as well as the overall scale DASS-T, was 0.65, 0.59, 0.69, and 0.69, respectively. While all correlations between the SCFQ and the DASS are higher than those for the CFQ, this difference is not significant.
The correlation between the SCFQ and CFQ with the AAQ-II was 0.70 and -0.69, respectively, indicating the appropriate validity of the SCFQ. Considering that the AAQ-II measures the level of acceptance and action in moving towards values (28), the negative correlation of these two tools shows that an increase in cognitive fusion can lead to a decrease in acceptance and committed action.
The correlation between the SCFQ and CFQ with life satisfaction, based on the SWLS, was -0.38 and -0.43, respectively, indicating a moderate negative correlation. In the study by Bolderston et al. (26), the correlation between the SCFQ and SWLS was -0.55, which also indicates a moderate correlation. Life satisfaction is a cognitive and emotional concept related to a person's overall assessment of the general state of their life (39). Additionally, the negative correlation of the SCFQ with the SWLS shows that a decrease in cognitive fusion is related to an increase in life satisfaction in people with mental disorders.
The correlation of the SCFQ with the CD-RISC was 0.44, and its correlation with the CFQ was 0.43. This finding is one of the most interesting aspects of the current research. Although resilience is mostly viewed positively, recent research also highlights its negative aspects (40). People who experience life adversity and have higher resilience and adaptability to life problems are more likely to experience symptoms of mental disorders, including anxiety, depression, and PTSD (21). The positive correlation of the SCFQ with the CD-RISC indicates the damaging dimension of resilience in people with symptoms of mental disorders, suggesting that these individuals, with high resilience, become accustomed to interpreting reality based on their thoughts (cognitive fusion).
Therefore, the findings of the present study regarding the reliability and validity of the SCFQ are consistent with the findings of Bolderston et al. (26). Considering that cognitive fusion, based on the pathological model of ACT, is one of the six main components of psychological inflexibility (10), research on the CFQ and SCFQ can significantly contribute to clinical work and the development of theories in this context. Due to the nature of SCFQ questions, future research can utilize this questionnaire in experimental research and clinical environments. The Persian adaptation of the SCFQ is now a valid tool that can be used in research and clinical work related to ACT in people with mental disorders. Additionally, this research investigated the correlation of the SCFQ with quality of life, anxiety, stress, depression components, and resilience in people with symptoms of mental disorders, which can be used in clinical research, counseling, and psychotherapy.
One of the limitations of the current study was that the sample of individuals with mental disorders was not divided into separate diagnostic groups. Future research can examine the SCFQ questionnaire on different mental disorders separately. Another limitation is that the test-retest reliability was not conducted on the SCFQ. Despite these limitations, this study is one of the first to examine the SCFQ on a clinical sample and the first in a Persian-speaking culture. The findings of this study can be useful in advancing research on cognitive fusion in general, and especially for Persian-speaking populations.
5.1. Conclusions
The current study has demonstrated that the CFQ and SCFQ have good psychometric properties in Persian-speaking populations with mental disorders. This provides initial evidence justifying the future use of the Persian CFQ and SCFQ.